Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 n.12 Pretoria Dec. 2011
FORUM
ISSUES IN MEDICINE
Preventing disease and saving lives: the malaria season is upon us
D Moonasar; C Asomugha; L Baker; L Blumberg; K I Barnes; R Maharaj; F Benson
The burden of malaria
In South Africa, malaria is endemic in three provinces - Limpopo, Mpumalanga and KwaZulu-Natal (Fig. 1) - and transmission occurs predominantly between September and May.1 Over the past decade, the National Department of Health (DoH) has focused intense efforts on preventing the local transmission of malaria, and on ensuring the prompt and effective management of cases, especially in the endemic provinces. The DoH has recorded significant success in reducing the burden of malaria through the implementation of its key interventions: Vector Control, Case Management, Surveillance, Health Promotion, and Epidemic Preparedness and Response. Notified malaria cases in the aforementioned provinces have decreased by 88% over the past decade, from 64 622 cases in 2000 to 7 626 in 2010. In the same period, malariarelated deaths have been reduced by 81%, from 458 to 87 deaths.2

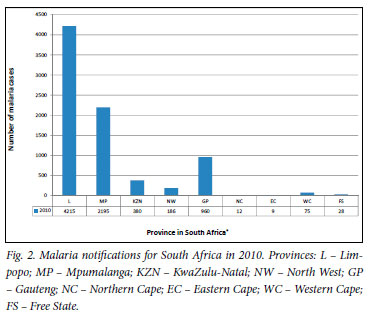
Malaria has been a notifiable disease in South Africa since 1956 (Government notice No. 2 081 of 1956). One of the key challenges that the DoH has historically faced is the irregularity of routine notifications, particularly from the private sector and public health facilities in non-endemic areas. In recent years, reporting appears to be gaining in efficiency, with an increase in malaria notifications from the non-endemic areas, especially Gauteng (Fig. 2). In this province, trends for malaria cases and related deaths show an increase over the past 2 years, with a peak in January. This seasonality is related to travellers returning from malaria-endemic areas, particularly Mozambique (Fig. 3).3
Malaria prevention and control strategies are being implemented robustly in the endemic provinces; however, similar strategies in the non-endemic provinces are lagging behind. This paper provides advice on the key measures for malaria prevention and management. Successful malaria treatment is dependent on a high index of suspicion for malaria in patients with acute febrile illness, and urgent treatment with effective medication.
Prevention of malaria
Travellers to malaria areas in southern Africa will be particularly vulnerable as the malaria risk season peaks in the coming months; therefore emphasis should be placed on prevention. Measures to avoid mosquito bites are the mainstay of malaria prevention and should be emphasised at all times. Whether or not appropriate chemoprophylaxis is warranted, should be determined by weighing up the risk of contracting malaria against the risk of adverse effects. Malaria risk is determined by travel location and accommodation, as well as season and length of stay. For example, the risk in built-up cities during the dry winter months is significantly less than that at a river-side campsite in summer. Malaria-transmitting mosquitoes feed at night; therefore people should ideally remain indoors from dusk until dawn, in rooms that have screens on the windows and doors.
The only insect repellents that are recommended are those containing diethyl 2 toluamide (DEET).4 Products containing 30% DEET 1 should be used for adults and children older than 2 months, as they give longer protection. They should, however, only be applied to exposed skin, particularly in young children. There is no benefit from using products containing more than 50% DEET.5
If the risk of contracting malaria warrants more protection than mosquito avoidance, chemoprophylaxis should be advised. There are 3 effective options available in South Africa; all require a doctor's prescription; therefore travellers should prepare for their travel timeously:
Mefloquine (weekly): start at least 1 week before entering a malaria area, take weekly while there and for 4 weeks after leaving the malaria area
Doxycycline (daily): start 1 - 2 days before entering a malaria area, take daily while there and for 4 weeks after exiting the malaria area
Atovaquone-proguanil (daily): start 1 - 2 days before entering the malaria area, take daily while there and for 7 days after leaving the area.1
All 3 medicines are effective if taken correctly and if compliance is assured.1 The chemoprophylaxis selection depends on the duration of visit, affordability, age, whether the person is pregnant or breastfeeding, has any medical conditions (e.g. epilepsy or depression), or is taking any other medication. Certain activities, such as flying or scuba diving, also need to be taken into account when choosing prophylaxis. The majority of adverse effects are mild; any severe adverse effects should be reported to the healthcare worker immediately, and the chemoprophylaxis changed if needed.
There is no scientific evidence that natural or homoeopathic products are effective against malaria; therefore their use should be avoided in the prevention of this potentially life-threatening illness.6
Diagnosis and management of malaria
Successful malaria treatment is dependent on a high index of suspicion for malaria in patients with acute febrile illness, as well as urgent treatment with effective medicines. Plasmodium falciparum accounts for the majority of malaria cases in Southern Africa, and causes almost all severe and fatal instances of the disease. South Africans, including residents of seasonal malaria transmission areas, are non-immune and are consequently at increased risk for developing severe malaria.

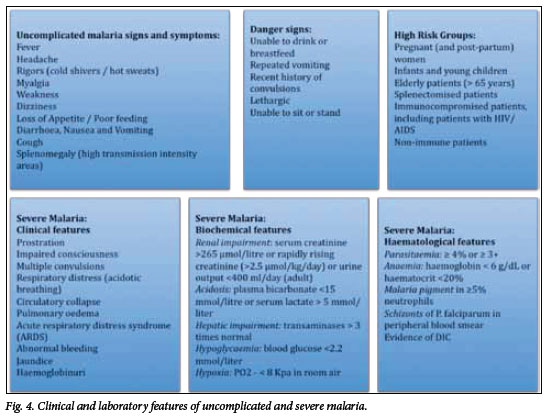
The diagnosis and management of malaria is urgent; delayed diagnosis and inappropriate treatment are associated with significantly increased morbidity and mortality.7 Classically, malaria presents with fever, rigors, headache and myalgia (Fig. 4), but the clinical features are nonspecific and may be confused with many other diseases, especially influenza. A definitive diagnosis should be made promptly by detection of the parasite with microscopic examination of a blood smear, or with the use of a rapid malaria antigen test. An initial negative test does not exclude the diagnosis of malaria, and repeat testing is mandatory in patients with continued symptoms and no alternative definitive diagnosis. All patients with malaria require careful clinical and parasitological follow-up.
For uncomplicated malaria, artemether-lumefantrine (Coartem) is recommended for first-line therapy. Alternatively, quinine plus either doxycycline or clindamycin can be used, if artemether-lumefantrine is unavailable or contra-indicated. High-level resistance precludes the use of chloroquine and sulfadoxine-pyrimethamine (SP) for P. falciparum malaria; halofantrine is not recommended.8
The major complications of malaria include: cerebral malaria, hypoglycaemia, anaemia, renal failure, acute respiratory distress syndrome (ARDS) and metabolic acidosis (Fig. 4). These carry high mortality rates, especially in children, pregnant women and those with HIV/AIDS. These complications indicate the need for urgent hospital admission, and require specific management.
For patients with severe malaria, intravenous artesunate is the preferred treatment; extensive studies in adults and children in Africa and Asia have shown that artesunate drastically reduces in-hospital mortality.9,10 Artesunate is not yet registered in South Africa, but is available in sentinel hospitals for the treatment of infected adults and children through the Parenteral Artesunate Access Programme. Where artesunate is not available, parenteral quinine is recommended, with an initial loading dose, and should be combined with doxycycline or clindamycin.
Despite being a preventable and readily treatable disease, malaria continues to cause thousands of cases in South Africa each year, with a high risk of life-threatening disease, if diagnosis is delayed or ineffective treatment is given.
1. Department of Health. Guidelines for the Prevention of Malaria in South Africa 2009. Pretoria: Department of Health, 2009. [ Links ]
2. Department of Health. Malaria Notifications 2011. Pretoria: South African Department of Health, 2011. [ Links ]
3. Weber IB, Baker L, Mnyaluza J, et al. The burden of imported malaria in Gauteng Province. S Afr Med J 2010;100(5):300-303. [ Links ]
4. American Academy of Pediatrics (AAP) Committee on Environmental Health. Follow safety precautions when using DEET on children. AAP News 2003; 22:200399. [ Links ]
5. Chiodini P, Hill D, Lalloo D, et al. Guidelines for Malaria Prevention in Travellers from the United Kingdom. London: Health Protection Agency, 2007. http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1203496943523 (accessed 11 October 2011). [ Links ]
6. Bradley DJ, Bannister B. Guidelines for malaria prevention in travellers from the United Kingdom for 2003. Communicable Diseases and Public Health 2003;6(3):180-199. [ Links ]
7. Mehta U, Durrheim DN, Blumberg L, et al. Malaria deaths as sentinel events to monitor healthcare delivery and antimalarial drug safety. Trop Med Int Health. 2007;12(5):617-628. [ Links ]
8. Department of Health. Guidelines for the Treatment of Malaria in South Africa 2010. Pretoria: Department of Health, 2010. [ Links ]
9. Visser Kift E, Kredo T, Barnes KI. Parenteral artesunate access programme aims at reducing malaria fatality rates in South Africa. S Afr Med J 2011;101(4):240-241. [ Links ]
10. Jones KL, Donegan S, Lalloo DG. Artesunate versus quinine for treating severe malaria. Cochrane Database of Systematic Reviews 2007(4); CD005967. [ Links ]
11. World Health Organization. International Travel and Health, Chapter 7. Geneva: WHO, 2011. http://www.who.int/entity/ith/chapters/ith2011chap7.pdf (accessed 11 October 2011). [ Links ]
Dr Moonasar is Director of Malaria at the National Department of Health (DoH) and a member of the National Malaria Advisory Group (MAG) and Global Malaria Elimination Group (MEG).
Dr Asomugha is Medical Advisor and Acting Director for Public Healthat the Gauteng Department of Health and Social Development. He is also Technical Head of the Gauteng Outbreak Response Team and a member of the Malaria Elimination Task Team.
Mrs Baker is a medicine information pharmacist, manages the Amayeza Information Centre, and is a member of both SCAT (Subcommittee on Chemoprophylaxis and Treatment of Malaria for MAG) and the EXCO of SASTM (South African Society of Travel Medicine).
Professor Blumberg is a medical microbiologist, a travel health and infectious disease specialist, and head of the Travel Health Unit at the NICD (NHLS). She is also a member of MAG.
Professor Barnes is a clinical pharmacologist in the Department of Medicine at UCT, and a member of MAG.
Professor Maharaj is Director of the Malaria Research Unit of the MRC, and a member of MAG and MEG.
Dr Benson is the DoH Cluster Manager for Communicable Diseases and Chairperson of the Multi-sectoral National Outbreak Response Team.
Corresponding author: D Moonasar (moonad@health.gov.za)














