Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.10 Pretoria oct. 2011
ORIGINAL ARTICLES
Acute hospitalisation needs of adults admitted to public facilities in the Cape Town Metro district
E de VriesI; P RaubenheimerII; B KiesIII; V C BurchIV
IMB ChB. Mitchell's Plain District Hospital, Department of Health, Western Cape, and Division of Family Medicine, University of Cape Town
IIMB ChB, FCP (SA). Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town
IIIMB ChB, FCP (SA), FCP (Neurology). Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town
IVMB ChB, MMed, PhD, FCP (SA), FRCP (London). Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town
ABSTRACT
INTRODUCTION: Public health care delivery in South Africa aims to provide equitable access at the most appropriate level of care. We studied to what extent the acute health care needs of adults admitted to public hospitals in the Cape Town Metropole were being appropriately met.
METHODS: A retrospective study was conducted of the hospital records of adults admitted to medical beds in public hospitals in Cape Town between August and November 2008. Intensive care unit patients were not included.
RESULTS: Of 802 beds in use, the estimated occupancy was at least 95%. The average time elapsed since admission was 7.9 days; 94.3% of medical admissions were acute; 45% were severely to critically ill on admission; and co-morbid disease was present in 78.1%. Of all admissions, 31.9% were HIV-positive, and 17% had active tuberculosis. At least 396 (51.6%) patients were deemed to have required specialist or subspecialist consultation to expedite appropriate care; 386 (50.3%) accessed the appropriate level of medical care required; 339 (44.2%) accessed a more sophisticated level of care than required; and 42 (5.5%) did not access an adequate level of care. CT scan and ultrasound accounted for 59% of all restricted tests done.
CONCLUSIONS: Our findings support the plan to provide more primary care hospital facilities in the metropolitan area. Most patients needing specialised care are accessing such care, and most patients accessing a higher level of care than needed can be addressed by ensuring that they first access primary care and are referred according to protocols.
In 2002, the Department of Health (DoH) began implementing a District Health System to deliver comprehensive health care to all South Africans,1 a key feature of which is equitable access to health care at the most appropriate level of service provision. To achieve this goal, the Provincial Government of the Western Cape initiated The Comprehensive Service Plan (CSP) for Implementation of Health Care 2010, to guide transformation of public health care services with an emphasis on improving and expanding primary care services while retaining specialist and subspecialist facilities within budget constraints.2 A second feature of the plan was dividing the province into districts, including the Cape Town Metro district which was subdivided into 8 subdistricts, each served by designated health care facilities.2 Since its implementation, patients seeking health care in the Cape Town Metro district are supposed to attend their designed clinic or Community Health Centre (CHC) before referral to the appropriate district, regional or central hospital.
According to the CSP, all hospital beds in the Western Cape are classified according to three levels: L1 beds are predominantly in district hospitals staffed by primary health care nurses, general practitioners, medical officers and specialist family physicians, where available; L2 beds are largely in regional hospitals staffed by specialist-led teams; and L3 beds are restricted to central hospitals staffed by specialists practicing in their subspecialty. According to the CSP, each hospital in the Cape Town Metro district is to have a mix of L1, L1/L2 or L2/L3 beds. A key feature of the plan has been reducing the number of L3 beds to significantly increase the number of L1 and L2 beds (Table I).3
An important debate in response to this plan is opposition by clinicians to the reduction of L3 beds in central hospitals and the reclassification of some regional hospitals to district hospitals. While more L1 beds are needed, the view has been expressed that this should not take place at the expense of L3 beds. However, the CSP states that 'it is generally accepted that a significant proportion (± 40 - 45%) of the services currently rendered by regional hospitals can be classified as L1 services. A similar amount of services currently rendered by central hospitals could be classified as L2 services.'2 We studied the acute clinical care needs of adults admitted to general medical wards in public hospitals in the Cape Town Metro district in order to address the debate about appropriate CSP bed allocations and the new Strategic Plan published in 2010.2,3
Methods
A retrospective cross-sectional descriptive survey was conducted of the hospital records of medical patients admitted to 11 public hospitals in the Cape Town Metropole from August to November 2008. Each hospital was surveyed on one weekday during this period. The choice of hospital and day of survey were randomly determined by the availability of the investigators. Each folder was reviewed by a general physician with subspecialist training working as a general physician at a regional hospital, and a family physician working at a district hospital.
During the survey, hospital beds were classified according to the highest level of on-site clinician expertise available, as outlined in the CSP.2 The Western Cape Strategic Plan for Health Care had not been published, and therefore the reclassification of some L3 beds in central hospitals, the reclassifying of GF Jooste Hospital and Victoria Hospital as district hospitals, and the conversion of some L2 beds to L1 beds in regional hospitals (New Somerset Hospital) had not taken place.3 Consequently, these changes are not reflected in the accompanying data.
In our study, the level of patient care deemed to be needed (L1, L2 or L3) was based on the severity of illness at presentation; the presence of co-morbid illness such as hypertension, diabetes mellitus, ischaemic heart disease, etc.; and the opinion of the investigators regarding the need for specialist or subspecialist consultation to expedite a diagnosis and institute treatment. The opinion of the experienced senior clinician investigators, after a detailed review of all the information available in the hospital folder at the time of the survey, was pivotal to the final decision, as they were able to use patient records to obtain an overall view of patients' hospital stay and their subsequent course. Despite numerous attempts to categorise the level of patient care needed using a rubric based on all the factors indicating severity and complexity of illness on presentation, we were unable to formulate a better model than the consensus opinion of the senior general physician and senior family physician.
The severity of illness at presentation was scored using the Modified Early Warning Score (MEWS)4 that was designed to detect medical inpatients at increased risk of deterioration and the need for urgent clinical intervention to prevent death. After validation in the UK, the MEWS has also been shown to predict the need for acute hospital admission and the risk of inpatient mortality of adult medical patients evaluated in the emergency department at a public hospital in Cape Town.5
Patients deemed suitable for inpatient care by a medical officer, with the assistance of a specialist family physician if needed, were classified as requiring L1 care; patients needing inpatient care by a general physician were classified as requiring L2 care; and patients needing inpatient care by a specialist with additional input from subspecialists were classified as requiring L3 care. This classification system was aligned with the bed classification system described in the CSP.2
We could not determine the length of hospital stay, as all surveyed patients were still hospitalised at the time of the survey, and therefore the number of days that had elapsed since admission was recorded.
Bed occupancy was estimated using the total number of adult general ward medical beds in use in regional and central hospitals in the Cape Town Metro district. The number of medical beds in district hospitals was taken to be approximately 60% of all available adult beds, since beds are not assigned to specific clinical disciplines in these hospitals. This estimate was based on a situational analysis conducted for the DOH of the Provincial Government of the Western Cape in 2007,6 and the extensive experience of the participating family physician.
Since we aimed to define the needs of adult admissions to general medical beds, intensive care unit (ICU) beds and beds in highly specialised units such as transplant units, isolation units, coronary care units and burns units were excluded. A small number of beds in L1 and L2 facilities provide additional supportive care not readily available in general wards e.g. airway protection in an obtunded drug overdose patient, management of ongoing chest pain in a patient with an acute myocardial infarct who cannot access a bed in a coronary care unit, or a patient presenting with acute diabetic ketoacidosis requiring closely supervised fluid and insulin therapy. These 'high care unit' (HCU) beds were included as they play a key role in service provision in hospitals that admit severely or critically ill patients and that lack on-site ICU services.
Data were entered into an Access database and analysed using Statistica V8.
The study was approved by the Human Research Ethics Committee of the University of Cape Town.
Results
Bed occupancy
A total of 841 medical beds were listed in the CSP document for the Cape Town Metro district.2 The 802 beds we identified in use during the survey formed the basis of the survey (Table II).6 (Situation analysis of the health care needs in the Western Cape and personal communication with hospital authorities, where possible). Of the 11 hospitals surveyed, 4 were staffed by medical officers and family physicians, where available; 5 had on-site general specialist services; and the 2 central hospitals (Groote Schuur and Tygerberg) had on-site specialist and subspecialist services. Of the 802 beds, only 20 (2.5%) provided additional monitoring and support for patients needing extra care not readily available in a general ward (HCU beds). A total of 767 patient records were surveyed. All unoccupied beds were counted as usable beds. The estimated bed occupancy across the Metro district was at least 95.6%, which is an underestimation of true bed occupancy because patients 'away from the ward' at the time of the survey, or 'booked' patients not in the ward at the time, were counted as part of the denominator, i.e. as 'empty' active beds in use. Their hospital folders could not be reviewed because clinical case notes accompany patients leaving a ward for an investigation or procedure to be performed.
Days elapsed since admission
Overall, the average number of days elapsed since admission was 7.9 days (range 0 - 55 days). Patients considered to need L3 care had spent more time in hospital than patients thought to need L1 or L2 care (Table III). Importantly, patients in district hospitals (L1 beds) needing L2 or L3 care had at least 30% longer stays recorded than when managed by specialists or subspecialists, and the hospital stay of patients requiring L1 care was not prolonged when managed by specialists in L2 or L3 facilities.
Acuity of illness
Most medical admissions (94.3%, N=723) were acute in nature; only 44 (5.7%) were elective admissions, 40 of whom were admitted to L3 beds. Therefore, only 15.4% of patients admitted to L3 beds were non-urgent, elective admissions for further investigation and management.
Co-morbidity and severity of illness on admission
Co-morbid disease was present in 78.1% (N=599) of patients surveyed; 112 (86.8%) in L1 beds, 283 (77.5%) in L2 beds and 204 (74.7%) in L3 beds. Co-morbid conditions included diabetes mellitus, hypertension, ischaemic heart disease, asthma, chronic obstructive pulmonary disease, post-TB bronchiectasis, chronic liver disease and other common conditions including symptomatic HIV infection and active tuberculosis. Noteworthy is that co-morbidity was highest in patients admitted to L1 beds.
Fig. 1 shows the distribution of MEWS (an indicator of severity of illness at presentation) for all the patients surveyed. There was a wide spread of scores, with a mean score of 2.5 (95% CI 2.4 - 2.7). Patients in L2 beds had the highest mean admission MEWS (3.3) while patients in L3 beds had the lowest mean admission MEWS (1.5).
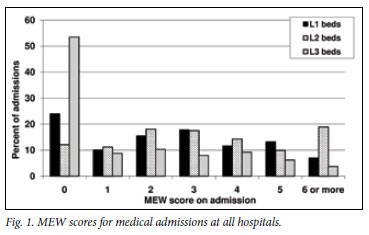
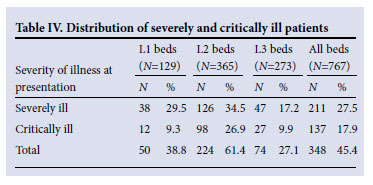
Of patients surveyed, 27.5% were severely ill on admission with a MEWS of 3 or 4 (Table IV). A further 17.9% were critically ill with a MEWS >5. Therefore, 45.4% (N=348) of all medical admissions were severely to critically ill on admission; 61.4% (N=224) of severely or critically ill patients were admitted to L2 beds.
HIV and TB burden of disease
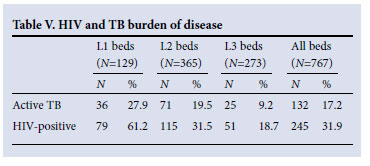
Overall, 245 (31.9%) patients had symptomatic HIV infection and a further 18 (2.3%) were suspected of being HIV-positive. A total of 61.2% of patients in L1 beds were HIV-positive (Table V); 132 (17.2%) had active tuberculosis, of whom 107 (81.1%) were admitted to L1 or L2 beds.
Inpatient consultation needed
The investigators identified the most appropriate level of care for each patient based on their overall impression of the clinical notes information. The most important considerations when making this decision were admission MEWS, the presence of co-morbid disease,
and the level of clinician expertise thought to be required to make an accurate diagnosis and formulate an appropriate treatment plan. Fig. 2 shows that 105 (81.4%) patients in L1 beds required L1 care, while 19 (14.7%) and 5 (3.4%) required L2 or L3 care, respectively; 215 (58.9%) in L2 beds only required L1 care; 36.2% (N=132), required L2 care, and 4.9% (N=18) needed L3 care. Of the 273 patients in L3 beds, 54.6% (N=149) required L3 care; 26.7% (N=73) required L2 care, and 18.7% (N=51) only required L1 care.
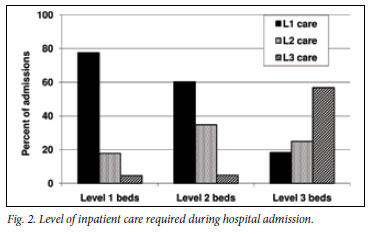
The main findings in Fig. 2 were that a total of 373 (93.9%) patients who needed specialist or subspecialist consultation accessed appropriate services; 44.2% of all admissions accessed an inappropriately sophisticated level of care, and only 24 (6.1%) did not access an adequate level of care.
Further evaluation of the patients admitted to L3 beds, but assessed as only requiring L1 care, showed that most had a limited spectrum of clinical problems; 66.6% had chronic heart failure, tuberculosis, cerebrovascular accident, pneumonia or drug overdose as a primary diagnosis. All were judged to be appropriate for care by an experienced medical officer or family physician with outreach by a general physician if needed.
The investigators encountered 104 patients (13.6%) in whom consensus regarding the most appropriate level of care needed was not reached. For the purpose of the study, these patients were assigned the highest level of care agreed upon by the investigators; 10 patients needed L1 care, 56 patients required L2 care, and 38 patients required L3 care.
Investigations performed
A total of 736 diagnostic procedures were performed of which 412 procedures, performed on 291 patients, were available at certain hospitals only; 70.4% (N=290) procedures could only be routinely done at Groote Schuur or Tygerberg hospitals. Only 3 investigations (computerised tomography (CT) scan (N=121), ultrasound (N=122) and echocardiography (N=41)) accounted for 68.9% of all restricted investigations done (Table VI).
Special beds required
Of 767 patients surveyed, 11.5% (N=88) required a bed for longer term care; 46 (52.3%) required a TB hospital bed; 21 (23.9%) required chronic care (long term placement); 16 (18.2%) required Hospice care and 5 (5.7%) required inpatient rehabilitation.
Sources of referral
A total of 41.9% of all admissions were referred from local CHCs; 220 (28.7%) were self-referred from home without prior evaluation at the nearest CHC. This referral pattern was mostly observed in patients using their own transport or ambulance to the nearest hospital at the discretion of the emergency care practitioner; the remaining 29.4% were admitted via the inpatient or outpatient services at district, regional or central hospitals. Overall, therefore, 329 (71.3%) of admissions followed the correct referral pathway either through the local CHC or via an outpatient service at one of the hospitals in Cape Town.
Discussion
Our survey provides an overview of the acute clinical care needs of adults admitted to general medical wards in public hospitals in a metropolitan district in South Africa. Public hospitals in the Cape Town Metro district are operating at medical bed occupancy rates >95%, which explains regular bed shortages and periodic closure of emergency units when hospitals have reached or exceeded their bed capacity. The Provincial Government of the Western Cape has recognised the need for additional hospital beds, and 2 new L1 facilities are under construction.
An important function of the highly specialised component of central hospitals is the capacity to electively evaluate complex medical problems. In this study, only 15% of central hospital admissions were elective in nature, supporting the argument that emergency admissions create a situation of 'access block' that currently curtails subspecialist services rendered by central hospitals.7 The need for more acute L1 and L2 beds to protect L3 services is being addressed.
At least 45% (N=348) of admissions were severely or critically ill, and 61% were admitted to general ward medical beds in L2 facilities since there are only approximately 20 non-ICU beds (HCU) offering additional monitoring and care facilities in the Cape Town Metro district. This case load is an additional burden on the system and lends weight to the suggestion that more HCU beds should be made available in L1 and L2 hospitals lacking ICU facilities.8 The data clearly demonstrate the important gatekeeping role that general specialists in L2 facilities play by dealing with a significant proportion of severely or critically ill patients. This point is borne out by the observation that the mean admission MEWS was highest for patients admitted to L2 facilities, and lowest for patients admitted to L3 general medical ward beds. The latter probably reflects the availability of on-site ICU services taking care of a significant proportion of the severely or critically ill patients admitted to these two hospitals.
The average number of days that had elapsed since admission was 7.9 days, which exceeds the Western Cape DoH's target of 3 days for L1 facilities, 4 days for L2 facilities and 6 days for L3 facilities.2 Important factors that determine length of hospital stay include the presence of comorbid illness, high MEWS on admission, and the level of expertise required to expedite care and keep the duration of hospital stay as short as possible. In our study, 78% of hospital admissions had comorbid disease with the highest prevalence among patients admitted to L1 facilities. Furthermore, when patients requiring L2 or L3 care were admitted to an L1 facility, their stay was considerably longer than when admitted to an L2 or L3 facility. This fact endorses the need for improved specialist outreach to L1 district hospitals, e.g. once- or twice-weekly problem-oriented ward rounds where difficult cases are discussed with a view to transfer for specialist care if needed. Our data suggest that appropriate specialist input may shorten the duration of hospital stay of complex patients, admitted to L1 facilities, by up to 30%.
At least 32% of adult medical ward admissions were HIVpositive, and at least 17% had active tuberculosis. HIV-positive patients admitted to hospitals in South Africa have advanced disease, are acutely ill with opportunistic infections and/or tuberculosis co-infection, and frequently have hospital stays >10 days.9-11 These factors may partly explain the anticipated hospital stays that were greater than the provincial targets in this study. Furthermore, patients with TB who require in-hospital care are very ill and often require much longer hospital stays; this is supported by the finding in this study that more than half of patients requiring longer-term in-hospital care had TB.
About half of the acute adult medical admissions required specialist or subspecialist consultation during their hospital stays. While this figure could be debated, it is clear that the severity of illness and extent of comorbid disease endorses the need for experienced hospitalists at all levels of care and further emphasises the need for structured specialist outreach services to primary care services.
Of patients accessing hospital care, 71.3% used the correct referral pathway. A total of 93.9% of patients who needed specialist or subspecialist consultation accessed appropriate services; 44.2% of all admissions accessed an inappropriately sophisticated level of care, and only 6.1% did not access an adequate level of care. These findings support the plan to allocate more beds to L1 and L2 services to address current needs. Access to appropriate care was achieved for 94.5% of patients requiring L3 care. These data suggest that access to highly specialised care is being achieved by almost all cases needing such care.
Of investigations required, 56% could only be performed at certain hospitals. CT and ultrasound scans accounted for 59% of all restricted tests done; their increased need is probably linked to the rising prevalence of tuberculosis and HIV infection in Cape Town. HIV-positive admissions frequently require investigation for smearnegative disseminated tuberculosis, and ultrasound examination of the abdomen is useful in this setting.12-14 Furthermore, HIVpositive patients with focal neurological signs often require CT investigation.15 Delayed access to these investigations, particularly at L1 facilities where most of the HIV-positive patients co-infected with tuberculosis are managed, is another reason why hospital stays currently exceed projected targets.
Our study has several limitations. It only provides a single crosssectional overview of the clinical activities of the hospitals surveyed. Therefore, the data are an approximation of services rendered in a dynamic setting. We gathered the information from the clinical case notes and did not interview or examine patients. The findings are therefore limited to this information, and inaccuracies cannot be excluded. We did not interview the doctors looking after the patients surveyed, and the authors' opinion of the level of care needed was only based on information obtained from patient folders. ICU beds were not surveyed because the focus was on general medical beds, which could be considered a limitation. Despite these limitations, this survey provides an overview of the acute hospitalisation needs of adults admitted to public health care facilities in a metropolitan district of South Africa.
The findings support the Provincial Government of the Western Cape's plan to provide more primary care hospital facilities in the Cape Town Metro district. Most patients needing specialised care access such care, but a large proportion of patients are accessing a higher level of care than needed, which can be addressed by ensuring that patients first access primary care and are referred according to protocols that are being developed.
References
1. National Department of Health. A District Hospital Service Package for South Africa. A Set of Norms and Standards. Pretoria: Directorate: Quality Assurance, Department of Health, 2002. http://www.ruralrehab.co.za/uploads/3/0/9/0/3090989/norms_and_standards_district_hospital.pdf (accessed 23 May 2011). [ Links ]
2. Department of Health, Provincial Government of the Western Cape. Comprehensive Service Plan for the Implementation of Healthcare 2010. Cape Town: Provincial Department of Health, May 2007. http://www.capegateway.gov.za/Text/2007/7/may15,2007-csp_2.pdf (accessed 23 May 2011). [ Links ]
3. Department of Health, Provincial Government of the Western Cape. Strategic plan 2010/11-2014/15. Cape Town: Provincial Department of Health, February 2010. http://www.capegateway.gov.za/ Text/2010/3/strat_p_2010_11_final_1.pdf (accessed 23 May 2011). [ Links ]
4. Subbe CP, Kruger M, Rutherford P, et al. Validation of a modified early warning score in medical patients. Q J Med 2001;94:521-526. [ Links ]
5. Burch VC, Tarr G, Morroni C. Modified early warning score predicts need for hospital admission and inhospital mortality. Emerg Med J 2008;25:674-678. [ Links ]
6. Department of Health, Provincial Government of the Western Cape. Situational Analysis of Health Care Needs of the Western Cape. Cape Town: Provincial Department of Health, May 2007. [ Links ]
7. Bond K, Ospina MB, Blitz S, et al. Frequency, determinants and impact of overcrowding in emergency departments in Canada: a national survey. Healthcare Quarterly 2007;10:32-40. [ Links ]
8. Van Zyl-Smit RN, Burch VC, Willcox PA. The need for appropriate critical care services at non-tertiary hospitals in South Africa. S Afr Med J 2006;97:268-272. [ Links ]
9. Colvin M, Dawood S, Kleinschmidt I, Mullick S, Lallo U. Prevalance of HIV and HIV-related diseases in the adult medical wards of a tertiary hospital in Durban, South Africa. Int J STD & AIDS 2001;12(6):386-389. [ Links ]
10. Kevany S, Meintjes G, Rebe K, Maartens G, Cleary S. Clinical and financial burdens of secondary level care in a public sector antiretroviral roll-out setting (G F Jooste Hospital). S Afr Med J 2009;99(5):320-325. [ Links ]
11. Burch VC, Benatar SR. Rational planning of health care based on observed needs. S Afr Med J 2006;96:796-802. [ Links ]
12. Malik A, Saxena AC. Ultrasound in abdominal tuberculosis. Abdominal Imaging 2003;28(4):574-579. [ Links ]
13. Patel MN, Benningfield S, Burch V. Abdominal and pericardial ultrasound in suspected extrapulmonary or disseminated tuberculosis. S Afr Med J 2011;101:39-42. [ Links ]
14. Wilson D, Nachega J, Morroni C, Chaisson R, Maartens G. Diagnosing smear-negative tuberculosis using case definitions and treatment response in HIV-infected adults. Int J Tuberc Lung Dis 2006;10(1):31-38. [ Links ]
15. Modi M, Mochan A, Modi G. Management of HIV-associated focal brain lesions in developing countries. Q J Med 2004;97:413-421. [ Links ]
Accepted 13 July 2011.
Corresponding author: V Burch (vanessa.burch@uct.ac.za)














