Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.10 Pretoria oct. 2011
SCIENTIFIC LETTERS
Success rate of myringoplasty at Groote Schuur Hospital
Juanita BeckerI; Darlene LubbeI
Ifinal-year medical student. Faculty of Health Sciences, University of Cape Town
IIFCORL (SA). Division of Otolaryngology, Groote Schuur Hospital and University of Cape Town
ABSTRACT
OBJECTIVES: The aim of this study was to determine the success rate of myringoplasty surgery performed at Groote Schuur Hospital and to evaluate some of the presumed prognostic factors.
DESIGN: The study design was a retrospective analytical cohort.
SETTING: Groote Schuur Hospital (tertiary medical centre), Cape Town.
SUBJECTS: This study assessed the success rate of 341 myringoplasty operations performed by surgeons in the Department of Otolaryngology from January 2005 to December 2009.
OUTCOME MEASURES: An unsuccessful operation was classified as a residual perforation seen at the 3-month follow-up visit that remained present at all subsequent visits. Presumed prognostic factors such as the rank of the surgeon, size of the perforation, location of the perforation, graft used and whether it was a revision procedure, were also evaluated. Where possible, the audiometric gain following surgery was calculated.
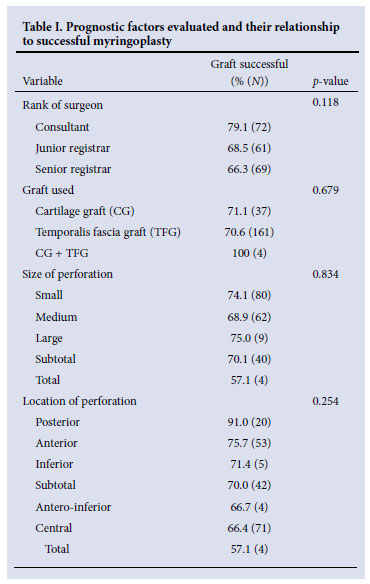
RESULTS: The overall success rate in terms of an intact tympanic membrane following myringoplasty was 71%. The average improvement in pure tone average following myringoplasty was 12.4 dB. In 64% of patients, socially acceptable hearing levels were present postoperatively (air-conduction of less than 30 dB). None of the presumed prognostic factors was a statistically significant determinant (p>0.05).
CONCLUSION: The success rate for myringoplasty (in terms of perforation closure) of 71% at Groote Schuur Hospital compares well with that quoted in the literature. There is no ethical dilemma from a surgical outcomes perspective of registrars performing myringoplasties.
To the Editor: Myringoplasty is the surgical restoration of the perforated tympanic membrane by grafting, with the principal goals being a 'dry ear' and improved hearing.1 Myringoplasty is a challenging procedure, and there is great variation in outcomes among various surgeons and institutions.2 The Royal College of Surgeons comparative ENT audit published in 1993 suggested that perforation closure could be expected in 65% of cases, with hearing improvement in 53%,3 but a study in 2002 proposed that the success rate for myringoplasty among British surgeons ranged between 74% (small perforation) and 56% (large perforation).4 An audit at Groote Schuur Hospital in 1993 by Black and Wormald found that perforation closure could be expected in 78% of cases.5 However, no recent data are available on the success rate, making it difficult to accurately inform patients as part of the consent process. At Groote Schuur Hospital, where registrars perform myringoplasty as part of their early training, the question also arose whether the results of trainees were poorer than specialists, and whether patients should be asked for consent accordingly.
Methods
We assessed the success rate and presumed prognostic factors in 341 myringoplasty operations performed at Groote Schuur Hospital by surgeons in the Department of Otolaryngology from January 2005 to December 2009. The study design of choice was a retrospective cohort using medical patient records. Prognostic factors such as the rank of the surgeon, size and location of the perforation, graft used (cartilage or temporalis fascia) and whether it was a revision procedure, were also evaluated. Where possible, the audiometric gain following surgery was calculated. Patients were followed up at 6 weeks, 3 months and 6 months. The operation was considered to have failed if a perforation were still present at 3 months. The size and location of the perforation was determined by microscopic evaluation, and the pure tone average was calculated by audiometric tests before and after surgery.
Results
The overall myringoplasty success rate was 71%. The average improvement in pure tone average was 12.4 dB, with 64% of patients achieving socially acceptable hearing levels postoperatively. The success rate in patients who had revision surgery was 72.4%. None of the prognostic factors assessed in Table I was statistically significant (p>0.05). Unfortunately, 16.7% of patients were lost to follow-up beyond 6 weeks.
Discussion
The success rate of myringoplasty (in terms of perforation closure) of 71% corresponds well with figures quoted in the literature.6 In some studies where the success rate was as high as 90%, the operation was performed by highly specialised surgeons with considerable experience in the procedure and a special interest in otology.7 Even though multiple studies have been conducted evaluating the influencing factors in myringoplasty, many of these remain unresolved.8
Rank of surgeon
At Groote Schuur Hospital, uncomplicated tympanic membrane repairs are generally performed by registrars in their first year of training. Our study showed a difference in the success rate between consultants and registrars in the department, but it was not statistically significant. Statistically significant results were demonstrated in the literature.6,8,9 In contrast, Palva et al.10 showed that success might depend more upon technical skill and attention to detail than the level of training or experience of the surgeon.
Location and size of perforation
The location of the perforation did not reflect significantly different results, with posterior perforations having the best result in our study (91%). Worse results are described in the literature for anterior perforations.10 However, some studies show worse results for posterior2 perforations, while other studies showed that the location of the perforation had no effect on success.11,12 Lee et al.4 and Onal et al.6 found significantly higher success rates with perforations smaller than 50%, but the size of the perforation was not found to be a significant parameter in our and other studies.11,13
Graft material used
The type of graft used did not have a significant effect on success. It is has been suggested that, in the case of grossly inflamed mucosa, repair should be performed with cartilage rather than temporalis fascia.7
Conclusion
The 71% success rate of myringoplasty, in terms of perforation closure, compares well with figures quoted in the literature, where the success rate in a teaching programme seems to be between 74% (small perforation) and 56% (large perforation).9 We also infer that there is no ethical dilemma, from a surgical outcomes perspective, in registrars performing myringoplasties.
Acknowledgement. We tender special thanks to Mr Rauf Sayed and Ms Roxanne Beauclair from the Department of Biostatistics at the University of Cape Town for their assistance in data analysis.
References
1. Merchant SN, Rosowski JJ, McKenna MJ. Tympanoplasty. Operative techniques in otolaryngology. Head and Neck Surgery 2003;14:224-236. [ Links ]
2. Albera R, Ferrero V, Lacilla M, Canale A. Tympanic reperforation in myringoplasty: Evaluation of prognostic factors. Ann Otol Rhinol Laryngol 2006;115:875-879. [ Links ]
3. Ryan RM, Brown PM, Cameron JM, Fowler SM, Grant HR, Topham JH. Royal College of Surgeons comparative ENT audit 1990. Clin Otolaryngol Allied Sci 1993;18:541-546. [ Links ]
4. Lee P, Kelly G, Mills RP. Myringoplasty: does the size of the perforation matter? Clin Otolaryngol Allied Sci 2002;27:331-334. [ Links ]
5. Black JH, Wormald PJ. Myringoplasty - effects on hearing and contributing factors. S Afr Med J 1995;85:41-43. [ Links ]
6. Onal K, Uguz MZ, Kazikdas KC, Gursoy ST, Gokce H. A multivariate analysis of otological, surgical and patient related factors in determining success in myringoplasty. Clin Otolaryngol 2005;30:115-120. [ Links ]
7. Gleeson M. Scott-Brown's Otorhinolaryngology, Head and Neck Surgery Vol. 1, 7th ed. London: Hodder Arnold, 2008:932-941. [ Links ]
8. Emir H, Ceylan K, Kizilkaya Z, et al. Success is a matter of experience: type 1 tympanoplasty: influencing factors on type 1 tympanoplasty. Eur Arch Otorhinolaryngol 2007;264:595-599. [ Links ]
9. Vartiainen E. The results of chronic ear surgery in a training programme. Clin Otolaryngol 1998; 23:329-335. [ Links ]
10. Palva T, Ramsey H. Myringoplasty and tympanoplasty - results related to training and experience. Clin Otolaryngol 1995;20:329-335. [ Links ]
11. Meranda D, Koike K, Shafiei M, et al. Tympanometric volume: a predictor of success of tympanoplasty in children. Otolaryngol Head Neck Surg 2007;136:189-192. [ Links ]
12. Singh GB, Sidhu TS, Sharma A, et al. Tympanoplasty type 1 in children: an evaluative study. Int J Pediari Otorhinolaryngol 2005;69:1071-1076. [ Links ]
13. Pignataro L, Berta LGD, Capaccio P, Zaghis A. Myringoplasty in children: anatomical and functional results. J Laryngol Otol 2001;115:369-373. [ Links ]
Accepted 16 May 2011.
Corresponding author: J Becker (bckjua001@uct.ac.za)














