Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 n.10 Pretoria Oct. 2011
IZINDABA
Denying reality no longer an option : stark HR report
Hastily re-opened nursing colleges need to churn out 51 200 professional nurses over the next decade and medical campuses double their output of GPs over the next 15 years - just to maintain the current (dismal) ratios to population (Fig. 1).
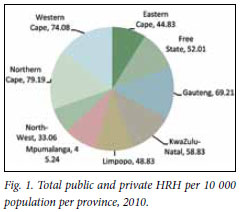
The full extent of the herculean task required to just maintain the status quo - let alone make a dent in the shortfall - emerged this August with the release of the government's long-awaited draft human resources (HR) for health strategy document.1 Scenario assumptions, drawing on key research and reports of many of the country's top experts, show that at a constant GDP growth rate and with 'concerted investment' for the next five years (3 - 5% annual growth rate in health staff spending), it is possible to close the gap in 'realistic numbers' in 20 years. The report takes a vital, unprecedented eagle's eye look at the haemorrhaging GP and specialist cadres and the skeletal, ageing and special skills-starved nursing sector in what it frankly describes as a 'failing health system'.
'Hire, hire'... not the top option
Recognising staffing and training budget limitations (filling currently listed public sector 'vacancies' across 27 key health professions would cost R40 billion), the draft HR strategy wisely seeks primary responses elsewhere. Engagement of additional professionals is cited as a 'second priority', although improved retention is flagged as critical to a successful overall outcome. Instead, the favoured front-line weapons are to be: overhauling management (accountability), design (task shifting, as in using mid-level workers to fill the skills gap between the nurse-based delivery system and doctors) and increased productivity. 'Moonlighting' and remuneration for work outside of the public service (RWOPS) are identified as issues affecting productivity and quality of care. The entirely re-engineered approach will require 'scopes of practice' of key disciplines to be reviewed, an in-depth probe and revision of referral patterns, and urgent development of training and career paths. The strategy paper openly admits that the occupation-specific dispensation (OSD), introduced disparately across provinces two years ago to improve career-pathing and address salary anomalies, 'had negative consequences', burying the opportunity to identify inhospitable working locations and remunerate scarce skills.
The phasing-in of mid-level workers, called clinical associates (currently being trained at Wits, Pretoria and Walter Sisulu faculties of health sciences), to staff all district hospitals (five per hospital, totalling 1 350), would take 17 years (until 2028). Again, this would require what the report modestly calls 'a steep increase in output'.
The 'problem statement' in the discussion document reads like a litany of woes, portraying a historical, professional neglect of human resources for health at national co-ordination level that borders on criminal.
Disparate provincial HR systems, forests of frozen academic clinical posts snowed in by top-heavy administrations and managements, unplanned and unfunded public sector posts, and inefficient management and recruitment processes are but a few. The attrition rate of health professionals from South Africa is conservatively estimated at 25% - working conditions and management cited as the biggest 'push' factors, followed by the risk of contracting HIV/AIDS/TB, workload and personal safety. By comparison, lifestyle and income hardly show up on the radar.
Wheels wobble two years into transition
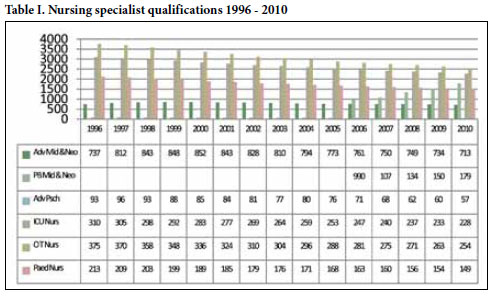
The most debilitating period from an HR perspective came between 1996 and 2008, when growth stagnated and key categories such as specialists and specialist nurses declined. Specialist medical staff plummeted by 25% between 1998 and 2006, with most leaving or being retrenched as academic hospital posts were frozen. Simultaneously, administration and management staff burgeoned at the expense of clinical appointments and nursing numbers dropped by 10 000, levelling off just above the 1997 level in 2007 as nursing colleges closed. From 2007 onwards there was slow (but unsustainable) growth with poor retention of graduates in all disciplines, unplanned and unfunded public sector posts and inefficient management and recruitment processes. Specialist nurse numbers declined even faster, especially in intensive care, operating theatres, advanced midwifery and psychiatry. The report cites medical specialists as complaining that operating theatre time was seriously constrained by the lack of appropriately qualified nurses.
The nursing workforce is reported as ageing, with 46% now over 50 years old and 16% already at retirement age (60) (Table I). The number needed to qualify over the next decade just to replace those retiring and leaving and to sustain the current ratio to population was 51 200. Overall, 70% of new graduates in the key professions over the last 10 years were not absorbed into the public sector, with 80% of physiotherapists and occupational therapists not retained in the public sector.
The cost in human life ...
This, to a large extent, is what lies under South Africa's high cost/poor performance health outcomes when compared with peer countries, most tragically the maternal mortality ratio that has nearly doubled from 369 (per 100 000 live births) in 2001 to 625 in 2007 (20 times higher than the 2015 Millennium Development Goal (MDG) target of 38). Only 43.7% of these deaths can be attributed to AIDS. The under-five mortality rate went from 59 in 1998 to 104 in 2007 (per 1 000 live births), a 'far cry' from the MDG target of 20.
The strategy paper says that ongoing foreign recruitment is necessary to ensure an adequate number of health professionals (especially academic clinicians and those willing to work in rural areas), but current policy and legislation severely undermine this and need urgent revision. To get 1 053 extra MB ChB graduates annually by 2025 requires increasing enrolment of medical students from 8 589 to 15 549 (a doubling of the current training platform) (Fig. 2).
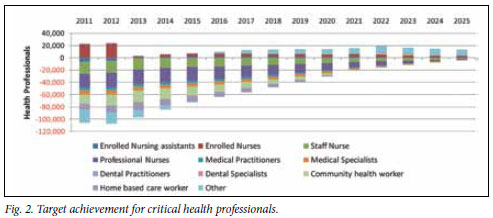
Retention scenarios showed that with 25% attrition, in 15 years the numbers of doctors 'do not increase significantly in the population'. Private GPs would have to be actively recruited to serve in the primary health care system and in district hospitals.
Eight strategic priorities are suggested. Leadership and governance, intelligence and planning (a centre for workforce intelligence is mooted), a workforce for new service strategies (to ensure 'bang for buck'), up-scaling and revitalising education, training and research, new academic training and service platform interfaces (e.g. rurally based), HR management, quality professional care and access to health professionals in rural and remote areas. These would nestle on six key foundations: community health workers, a predominantly nurse-based system (currently 80%), the introduction and rapid expansion of mid-level workers, expansion of general medical doctors and selected specialist doctors and public health specialists. The new model provides projections for over 100 'registerable' health professions and is designed to be flexible around baseline data and several assumptions for each profession.
'Tempting though it is, we simply cannot afford to be overwhelmed,' one observer on Dr Olive Shisana's Ministerial Advisory Task Team for National Health Insurance, commented, on condition of anonymity. The data are startling and stark, but denying reality is gladly (it seems from this official consultative report) no longer an option.
Chris Bateman
chrisb@hmpg.co.za
1. Human Resources for Health for South Africa 2030. Draft HR Strategy for the Health Sector: 2012/13 - 2016/17. Consultation Document. August 2011. http://www.doh.gov.za/docs/ stratdocs/2011/draftHRstrategy_Consultation.pdf [ Links ]














