Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 n.6 Pretoria Jun. 2011
ORIGINAL ARTICLES
Interruptions in payments for lay counsellors affects HIV testing at antenatal clinics in Johannesburg
Vivian BlackI; Courtenay SpragueII; Matthew F ChersichIII
IMB BCh, BSc. WITS Reproductive Health and HIV Institute, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
IIPhD, double MA. Graduate School of Business Administration, University of the Witwatersrand
IIIPhD, MB BCh. Centre for Health Policy, School of Public Health, University of Witwatersrand; and International Centre for Reproductive Health, Department of Obstetrics and Gynaecology, University of Gent, Belgium
ABSTRACT
HIV testing uptake at 3 antenatal clinics in Johannesburg was 53% (1 333/2 502) during 4 months when lay counsellors were unpaid, which was lower than the 7 months when payment was provided (79%; 3 705/4 722; p<0.001), and a subsequent 12-month period (86.3%, 11 877/13 767; p<0.001) when counsellors were paid. Consistent remuneration of lay counsellors could markedly improve services for preventing mother-to-child HIV transmission.
To reduce the contribution of HIV to maternal, infant and under-5 mortality in South Africa,1,2 the quality of services for preventing mother-to-child transmission (PMTCT) of HIV, and antiretroviral therapy (ART) for HIV in pregnant women, must be substantially enhanced. Access to these services is, however, contingent on diagnosing HIV infection - a role commonly performed by lay counsellors in South Africa through provider-initiated testing and counselling.3 Lay counsellors also prepare patients for ART, and provide counselling on adherence to ART regimens and on infant-feeding options.
Employment and remuneration arrangements for lay counsellors in South Africa are characterised by the payment of stipends, rather than formal employment contracts. This arrangement is probably due to the cadre being relatively recent, with a rapidly evolving scope of work. Moreover, the Department of Health commonly contracts with intermediary non-governmental organisations (NGOs) to manage and pay lay counsellors.4 Late payment and poor working conditions are reportedly frequent, and ambiguity in employment status limits the counsellors' protection under labour laws. We investigated whether these conditions affect HIV testing at 3 clinics in inner-city Johannesburg.
Methods
We reviewed the uptake of HIV testing among women at their first antenatal clinic (ANC) visit from March 2007 -December 2009. Administrative staff recorded the number of women attending ANCs, and midwives determined the number completing HIV testing and counseling at their first ANC visit. The proportion completing HIV testing in the months that counsellors received remuneration was compared with months without payment. Analysis excluded data during a national public sector strike in June 2007.
Testing uptake in a first period (March 2007 -February 2008) was also compared with a second period from March 2008 -December 2009 when no further payment interruptions occurred. Remuneration systems in this second period were administered by a university research unit using international donor funding. As several public holidays in December might have influenced clinic attendance and worker performance, we analysed data including and excluding the December months.
Data were entered into Microsoft Excel 2003 and analysed using Graph Pad Calculator (2002-2005 Graph Pad Software Inc., San Diego, CA, USA). Chi-square tests were used to detect differences between proportions, and an unpaired Student's t-test compared the mean number tested in each group.
The Human Research Medical Ethics Committee of the University of the Witwatersrand granted ethics approval for the study (protocol number M081160).
Results
In the first period, 7 451 pregnant women attended antenatal clinics. Excluding June (the month of the strike when only 277 women attended ANC), the mean monthly attendance was 657 (standard deviation (SD) 128; 95% CI confidence interval (CI) 653 -661). Lay counsellors did not receive remuneration in July, August, September and November 2007. Payment for July -September was made at the end of October and for November at the end of December 2007 (Fig. 1).
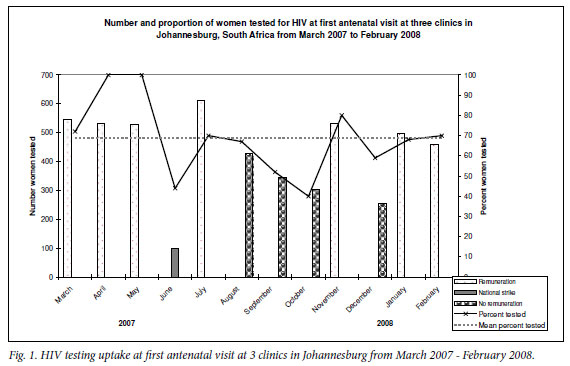
In the 7 months following receipt of payment, 79% of women received HIV results (3 705/4 722). By contrast, only 53% tested in the 4 months following non-payment (1 333/2 502; risk ratio (RR) 1.47; 95% CI RR 1.12 -1.53; p<0.001); which was similar to the proportion tested in the month of the strike (100/227; 44%). The mean number of women tested for HIV in the months that followed lay counsellor payment was 529 (SD 46.9), compared with 326 (SD 84.3) following non-payment (p<0.001). Excluding December did not alter the findings (data not shown).
Comparison of the two time periods
Overall, 69.0% of women completed HIV testing in the first 12 months (5 138/7 451), lower than the 86.3% uptake in the period from March 2008 -December 2009 (11 877/13 767 women; p<0.001). HIV testing in this second period was also 1.17 times higher than in the months of the first period when counsellors received regular payment (95% CI RR 1.14 -1.21).
Discussion
Late payment of lay counsellors markedly reduced uptake of HIV testing, which remains the key barrier to performance of PMTCT services in South Africa.5 As the practice of paying lay counsellors through intermediaries and late remuneration are common in South Africa,4 it is likely that unstable employment conditions affect HIV testing in many other parts of the country. Given that barriers to testing such as HIV stigma and fear of a positive result remain high, it is critical that constraints at a health system level are minimised, especially concerning modifiable factors around poor performance of health workers.
Others have also shown that inconsistent remuneration of community health workers negatively affects their performance.3 Late payment probably undermines motivation and, more practically, the ability of counselors to fund their transport to work, leading to absenteeism. Negative effects on overall motivation may account for the lower testing figures even in the months when payment was received in the first period, compared with the period with secure long-term payments.
Full recognition of the role that lay workers play - together with the provision of formal employment contracts and labour protection - could significantly improve public health HIV service delivery. It may mark an important step towards reversing the impact of HIV on maternal and infant deaths, almost all of which are avoidable. In a country with limited personnel in the public sector, it is imperative that all opportunities are fully exploited to mitigate the impact of HIV on women and children.
The authors thank PEPFAR and UNAIDS who assist with funding of staff working in the antenatal clinics; the South African Department of Health in whose clinics the research was conducted; and the lay counsellors at the study sites.
References
1. Bradshaw D, Nannan N. Mortality and morbidity among women and children. In: Ijumba P, Padarath A, eds. Durban: South African Health Review, 2006. [ Links ]
2. Black V, Brooke S, Chersich MF. Impact of HIV treatment on maternal mortality at a tertiary center in South Africa: a five year audit. Obstet Gynecol 2009;114:292-299. [ Links ]
3. Lehmann U, Sanders D. Community health workers: What do we know about them? Evidence Report for WHO. 2007. http://www.hrhresourcecenter.org/node/1587 (accessed 15 September 2009). [ Links ]
4. Mthembu GT. South African's health system requires a state of emergency. 2006. http://www.tac.org.za/community/node/2188 (accessed 15 September 2009). [ Links ]
5. Saving Mothers 2005-2007. Fourth report on Confidential Enquiries into Maternal Deaths in South Africa. Pretoria: Department of Health, 2009. http://www.doh.gov.za/docs/reports/2007/savingmothers.pdf (accessed 15 September 2009). [ Links ]
Accepted 19 August 2010.
Corresponding author: V Black (vblack@rhru.co.za)














