Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.5 Pretoria may. 2011
ORIGINAL ARTICLES
Stroke outcomes in a socio-economically disadvantaged urban community
Linda de VilliersI; Motasim BadriII; Monica FerreiraIII; Alan BryerIV
IMB ChB, FCP (SA). Division of Geriatric Medicine, Groote Schuur Hospital and University of Cape Town, and PhD candidate, Faculty of Health Sciences, Stellenbosch University
IIMSc (Med), PhD. Department of Medicine, Groote Schuur Hospital and University of Cape Town
IIIDPhil. Albertina and Walter Sisulu Institue of Ageing, Department of Medicine, University of Cape Town
IVMB BCh, FCP (SA), MMed (Neurology), FC Neurology (SA), PhD. Division of Neurology, Groote Schuur Hospital and University of Cape Town
ABSTRACT
AIMS: To determine survival, disability and functional outcomes of stroke patients following their discharge from an acute stroke unit in an urban community with limited rehabilitative resources.
METHODS: Stroke patients were recruited from a district hospital in Cape Town and followed-up for 6 months. Clinical characteristics, demographic and socioeconomic data, and disability and function as measured by modified Rankin Score (mRS), modified Barthel Index (mBI) at recruitment and 3 follow-up visits, were recorded.
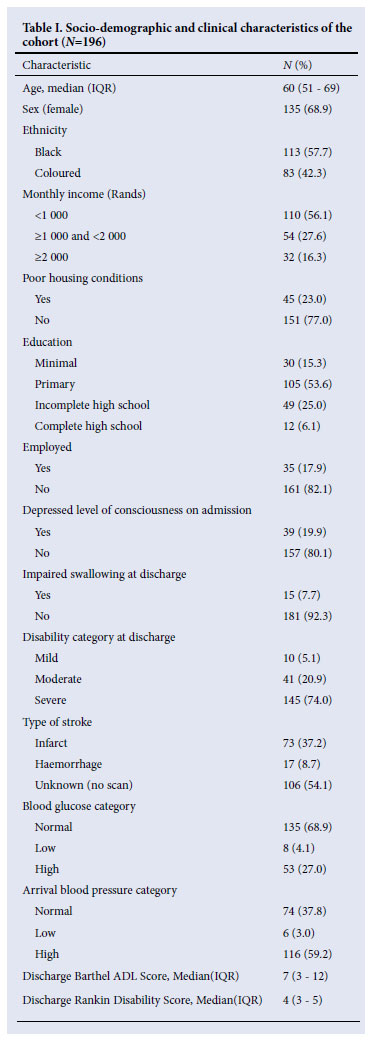
RESULTS: The study included 196 patients. Median age was 60 (IQR 51 - 69) years, 135 (68.9%) were female, 57.7% black, 42.3% coloured, and 45 (23%) died within 6 months. At discharge, median mBI score was 7 (IQR 3 - 12) and median mRS 4 (IQR 3 - 5). In the multivariate regression models, only function (mBI OR 0.88, 95% confidence interval (CI) 0.79 - 0.96, p<0.0001) and disability (mRS 0R 2.34, 95%CI 1.20 - 4.54, p<0.0001) were independently associated with risk of death. Shack housing was independently associated with moderate or severe disability (odds ratio 3.42, 95%CI 1.22 - 9.59, p=0.02). Despite limited rehabilitation resources, 67% of survivors had mild to moderate disability at 6 months.
CONCLUSION: Apart from initial stroke severity, risk factors for poor survival were a severe disability category and the presence of impaired swallowing at discharge. Shack housing was independently associated with poor functional outcomes. These findings should be helpful in allocating home-based care and inpatient rehabilitation resources to high-risk groups to improve outcomes.
The stroke unit model of care reduces mortality and dependency after stroke in developed countries.1,2 The multidisciplinary stroke unit model of care improves early outcomes in an under-resourced urban setting in South Africa.3 In such a setting, resources for rehabilitation (inpatient and outpatient) are limited and there is concern that early benefits achieved in an acute stroke unit could be eroded by a lack of adequate rehabilitation after discharge. We aimed to determine the survival, disability and functional outcomes of stroke patients following their discharge from an acute stroke unit to community based health care and rehabilitation. We sought to identify factors that predicted poor outcomes. The ability to identify patients at risk of poor outcomes could assist in developing community-based models of stroke care with effective allocation of scarce resources.
Methods
Our patients were recruited from a 200-bed urban district hospital in Cape Town that has a 6-bed acute stroke unit and 4 additional medical beds allocated for overflow. It is the only hospital providing primary and secondary level health care for an estimated population of more than 1 million black and coloured people, who comprise the poorest section of the total regional population that in 2001 was 4 524 335 persons.4,5
Stroke patients are referred to provincial inpatient rehabilitation centres that provide rehabilitation for stroke and also for any condition resulting in functional limitations. The province has 3 inpatient rehabilitation centres, with a total of 544 beds. The rehabilitation facility to which most patients from this study hospital are referred has 280 beds. At the time of the study, the facility was staffed by 2 occupational therapists, 2 physiotherapists, 1 speech therapist, 2 social workers and a dietician. Patients at the facility received less than 2 hours of individual rehabilitation therapy per week, which is considerably less than the hour or more of individual daily therapy achieved in European rehabilitation centres.6
Because of the limited inpatient rehabilitation resources, patients assessed as likely to have a poor prognosis for functional recovery were discharged home once medically stable, where they received home-based care. Poor prognosis was determined by the rehabilitation team on the basis of prior dependency or cognitive impairment and co-morbid illness rendering the patient incapable of participating in physical rehabilitative therapy. Patients who were immobile and dependent in Activities of Daily Living (ADLs) and assessed as having potential for functional recovery were referred for inpatient rehabilitation. Those who were mobile and not severely disabled were referred for outpatient rehabilitation at their local community health centre.
Three community health centres in the hospital district provided outpatient rehabilitation. The total rehabilitation staff across these facilities was 4 physiotherapists, 1 occupational therapist and 2 occupational therapy assistants. Stroke patients received 30 minutes' individual therapy once a week or once every second week. Outpatient speech therapy was only available at one tertiary hospital.7
Patients with a clinical diagnosis of stroke (as defined by the World Health Organization) admitted to the GF Jooste Hospital stroke unit between 24 August 2004 and 12 January 2006 were interviewed and assessed by the first author prior to discharge.8 Eligibility criteria for recruitment included any patient with a stroke, alive at the time of discharge, who lived within a 20 km radius of the hospital, and could give a fixed address. Written informed consent was obtained from the patients or their caregivers.
Patients were followed up at 2 weeks, 3 months and 6 months at their homes, using standardised follow-up questionnaires, by field workers trained in the administration of these questionnaires, interview technique and the assessment scales. Assessment scales used included the 10-item modified Barthel Index (mBI) and the modified Rankin Score (mRS).9,10
Definition of variables
For this study, type of stroke was defined as infarction or haemorrhage. Haemorrhagic stroke was only diagnosed if confirmed by CT scan but, owing to resource constraints, only 49% of patients had CT scans. Disability was defined as none or minimal (mRS <2), moderate (mRS score 3) or severe (mRS >4). Admission level of consciousness was defined as depressed if the patient was scored as drowsy on the admission Modified Early Warning Score (MEWS).11 Admission blood pressure was categorised as low if <100/60, normal or moderately elevated if between 100/70 and 160/90, or high if >160/90. Admission glucose was defined as low if <4 mmol/l (70 mg/dl), normal 4 -8 mmol/l (70 -144 mg/dl) and high if >8 mmol/l (144 mg/dl).
Housing conditions were categorised as 'poor' for a shack dwelling with no piped water. Monthly household income was defined as low (<R1 000), intermediate (R1 000 -2 000) or high (>R2 000). Patients' education was defined as minimal level (<4 years of formal education), primary level (<8 years of formal education), incomplete high school level (8 -11 years of education), and completed high school level (>12 years of education).
Two-week, 3-month and 6-month mortality was defined as the proportion of stroke patients who died (irrespective of cause) within those time-frames after discharge. Functional impairment was measured by the mBI, and disability by the Rankin score.
Statistical analysis
Categorical variables (sex, ethnicity, income category, housing, education category, admission level of consciousness, impaired swallowing, type of stroke, disability category, blood glucose category and blood pressure category) were compared using the χ2 test, or Fisher exact test when appropriate, and continuous variables (age, mBI, mRS) were compared, owing to non-normality of distribution of variables analysed, using the Mann-Whitney or Kruskal-Wallis non-parametric test. Predictors of 6-month mortality were determined by fitting univariate and multivariate Cox hazard regression models. Univariate and multivariate logistic regression models were fitted to determine factors associated with functional impairment (severe v. mild or moderate) at 6 months. All tests were 2-sided, and a p value <0.05 was considered significant. The experience of this cohort was compared with a similar study. Chi-square tests were performed to examine the differences in function at 6 months as measured by the mBI.
The study protocol was approved by the University of Cape Town Research and Ethics Committee. Funding was granted by the South African Circulatory Diseases Research Foundation (CDRF), the Swedish International Development Co-operation Agency and the South African National Research Foundation.
Results
The inclusion criteria were satisfied by 221 patients; 24 of them were excluded, 1 refused to participate and 23 were untraceable at the given address. There were no significant differences at recruitment between these patients and the 196 included in the analysis. The median length of hospital stay was 8 days (range 1 -36 days). The socio-demographic and baseline clinical criteria of these patients are described in Table I.
Mortality
Of the 196 patients included in the analysis, 45 (23%) died within 6 months. The cumulative mortality within 14 days was 3%, and 18% at 3 months. The cause of death was the incident stroke in 21, recurrent stroke 3, aspiration pneumonia 5, pulmonary embolus 1, cardiac causes 6, hypoglycaemia 1, and unknown in 7 patients.
Of the 45 patients with severe stroke who were discharged home or to a care facility because they were not considered candidates for rehabilitation, 20 (44.4%) died within 6 months. Of the 14 patients with impaired swallowing necessitating nasogastric tube feeding at discharge, all of whom had severe strokes, all 3 discharged died; and of the 11 discharged to inpatient rehabilitation, 5 (45.5%) died within 6 months.
Mortality rates differed significantly by housing condition, depressed level of consciousness on admission, impaired swallowing at discharge, disability category at discharge, discharge mBI and discharge mRS (Table II). In the multivariate Cox hazards regression model, variables independently associated with risk of death were discharge mBI (hazards ratio (HR) 0.88, 95% CI 0.79 -0.96, p=0.005), discharge mRS (HR 2.34, 95% CI 1.20 -4.54, p=0.01) and disability category at discharge for the severe and moderate categories, respectively (HR 0.10,95% CI 0.01 -0.81, p=0.02 and HR 0.02, 95% CI 0.002 -0.33), compared with the mild category.
Functional outcome
At discharge, the median mBI score was 7 (IQR 3 -12) and median mRS was 4 (IQR 3 -5). By 6 months, the median mBI score in the survivor group was 17 (IQR 13 -19) and median mRS was 2 (IQR 2 -3). Overall, of the 117 survivors at 6 months, 25 (22%) had severe disability, 31 (26%) had moderate disability, and 61 (52%) had mild or no disability.
In a multivariate logistic regression model, apart from disability at discharge, poor housing conditions was independently associated with severe disability at 6 months (odds ratio 3.42, 95%CI 1.22 -9.59, p=0.02).
Discussion
In contrast with other sub-Saharan Africa studies, this study had a larger sample size with relatively few patients lost to follow-up (89% follow-up at 6 months post discharge).12,13 The strength of the study is that it was conducted in a community hospital, which takes all patients, and not a tertiary hospital, as in other African studies, where access and referral patterns introduce bias into the sample.12,13 A limitation of this study was the lack of CT facilities for all patients with suspected stroke, which resulted in 49% of patients having CT brain scans. To limit the number of non-vascular lesions included in the study, all patients <50 years of age, those with no vascular risk factors, and those with HIV, syphilis or Mycobacterium tuberculosis infection, had CT scans. Although our mortality rates appear to be similar to those in European studies, such comparisons are inappropriate, considering the difference in the patient case mix (e.g. the younger age of our cohort, median age 60 years) and that patients with milder strokes were often not admitted to hospital owing to bed pressure.14 The 6-month mortality in this setting appears less than in other African countries such as The Gambia (47%) and Nigeria (46%), where patients were not treated in a stroke unit and there were no rehabilitative services.13,15
The rural arm of our study reported a 3-month mortality of 30%.16 However, given the small sample size (N=30) of the rural study, the apparent reduction of mortality in this study should be interpreted with caution. As expected, stroke severity, especially if swallowing was impaired, was predictive of poor outcomes. Despite limited rehabilitative resources, most survivors improved in terms of function and disability, and 67% of survivors had mild to moderate disability at 6 months. Poor housing was an independent predictor of poor functional outcome, suggesting that these patients access less rehabilitative resources, which could be overcome by prioritising them for inpatient rehabilitation.
The poorest survival was in patients with severe strokes discharged directly home, particularly if they needed nasogastric tube feeding. Such patients should in future be prioritised for intensive home based care by practitioners trained in the care of stroke and in nasogastric tube management. Our findings should be of value in directing future research into the determinants of poor outcome in the groups identified as being at risk, which could inform the future planning and implementation of community-based stroke services in an under-resourced setting such as our own, which would also be applicable to other developing countries.
References
1. Rudd AG, Hoffman A, Irwin P, Lowe D, Pearson MG. Stroke unit care and outcome: results from the 2001 National Sentinel Audit of Stroke (England, Wales and Northern Ireland). Stroke 2005;36(1):103-106. [ Links ]
2. Indredavik B, Bakke F, Solberg R, Rokseth R, Haaheim LL, Holme I. Benefit of a stroke unit: A randomized controlled trial. Stroke 1991;22: 1026-1031. [ Links ]
3. de Villiers L, Kalula SZ, Burch VC. Does multidisciplinary stroke care improve outcome in a secondarylevel hospital in South Africa? International Journal of Stroke 2009;2:89-93. [ Links ]
4. City of Cape Town. Reports and Publications: Socioeconomic Characteristics of the Suburbs. Cape Town: Cape Metropolitan Council, 2000. [ Links ]
5. Statistics South Africa. Census 2001. Key results. Pretoria: Statistics South Africa, 2002. http://www.statssa.gov.za/census01/html/default.asp (accessed 19 December 2008). [ Links ]
6. De Wit L, Putman K, Schuback B, et al. Motor and functional recovery: a comparison of 4 European rehabilitation centres. Stroke 2007;38:2101-2107. [ Links ]
7. Misbach S. The implementation of the rehabilitation service package in the Metropole Health District, Western Cape Province, South Africa. MPH thesis, UWC, 2004. http://etd.uwc.ac.za/usrffiles/modules/etd/docs/etd_init_4624_1176816743.pdf (accessed 19 December 2008). [ Links ]
8. Hanato S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Org 1976;54:541-553. [ Links ]
9. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14:61-65. [ Links ]
10. Rankin J. Cerebral vascular accidents in patients over the age of 60: 2 prognosis. Scott Med J 1957;2:200-215. [ Links ]
11. Burch VC, Tarr G, Morroni C. Modified early warning score predicts the need for hospital admission and inhospital mortality. Emerg Med J 2008;25(10):674-678. [ Links ]
12. Walker RW, Rolfe M, Kelly PJ, George MO, James OFW. Mortality and recovery after stroke in the Gambia. Stroke 2003;34:1604-1609. [ Links ]
13. Garbusinki JM, van der Sande MA, Bartholome EJ, et al. Stroke presentation and outcome in developing countries: a prospective study in the Gambia. Stroke 2005;36(7):1388-1393. [ Links ]
14. Thorvalsden P, Asplund K, Kulaasma K, Rajakangas AM, Schroll M. Stroke incidence, case fatality, and mortality in the WHO MONICA Project. Stroke 1995;26:361-367. [ Links ]
15. Ogun SA, Ojini FI, Ogungbo B, Kolapo KO, Danesi MA. Stroke in south west Nigeria, a 10-year review. Stroke 2005;36:1120-1122. [ Links ]
16. Wasserman S, de Villiers L, Bryer A. Community-based care of stroke patients in a rural African setting. S Afr Med J 2009;99(8):579-583. [ Links ]
Accepted 6 December 2010.
Corresponding author: L de Villiers (linda.devilliers@uct.ac.za)














