Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 n.5 Pretoria May. 2011
ORIGINAL ARTICLES
Errors in drug administration by anaesthetists in public hospitals in the Free State
M LabuschagneI; W RobbetzeII; J RozmiarekIII; M StrydomIII; M WentzelIV; B J S DiedericksV; G JoubertVI
IBSc Agric (Hons), MB ChB student. School of Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein
IIBMedSc Radiation Science, BMedSc Hons (Medical Physics), MB ChB student. School of Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein
IIIMB ChB student. School of Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein
IVBMedSc Radiation Science, BMedSc Hons (Medical Physics), MB ChB student. School of Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein
VMB ChB, MMed (Anaesth), FCA (SA), BA, Dip Av Med. Department of Anaesthesiology, Faculty of Health Sciences, University of the Free State
VIBA, MSc. Department of Biostatistics, Faculty of Health Sciences, University of the Free State
ABSTRACT
OBJECTIVE: To investigate errors in administering drugs by anaesthetists working in public hospitals in the Free State province.
METHODS: Anonymous questionnaires were distributed to doctors performing anaesthesia in public hospitals in the Free State, i.e. 188 doctors at 22 public sector hospitals. Outcomes included demographic information on respondents, information regarding the administration of anaesthetics, reporting of errors, and the occurrence of errors during anaesthesia.
RESULTS: The response rate was 46.3%; 48.8% were medical officers, and 39.3% of participants were involved in at least one event of erroneous drug administration. Registrars and specialists reported the most errors. Most events were of no clinical significance, caused no permanent harm to patients, and most commonly involved fentanyl and suxamethonium. Of the respondents, 23.8% indicated that they were aware of a South African standard for colour-coding syringe labels, and 92.9% indicated that they would report anaesthetic errors if a single reporting agency for such events existed.
CONCLUSION: More than a third of participating anaesthetists were involved in a drug error at some stage in their practice. Preventive systems and precautionary measures should be put in place to reduce drug administration errors.
An error is regarded as the failure to perform an action as intended.1 Medication errors in anaesthesia arise from errors in prescription, dispensing or administration of medication, that result in a patient receiving an incorrect drug or drug dosage,1 or administration via an incorrect route. Erroneous administration of drugs causes unnecessary harm to patients, and is especially relevant in anaesthesia as potent intravenous agents are frequently injected.2,3 Their effects may be of no clinical significance, result in minor morbidity requiring immediate intervention to prevent permanent injury, or major morbidity (e.g. cardiac arrest, stroke or permanent injury or death) as the main or contributory cause.4
Errors can be categorised as system, equipment and human error. The latter is associated with knowledge and experience, and other contributory factors such as haste, fatigue, stress or illness.5 Of a total of 329 reported anaesthesia errors, 136 (41.3%) were human errors, of which 17.6% were knowledge-, 27.9% skill-and 25.7% rule-based, and 6.6% were technical errors.5
Most anaesthetists in South Africa will administer an erroneous drug at some stage,2 of which a few may lead to severe patient morbidity or death. A large study6 of more than 30 000 anaesthetics administered by specialist and/or trainee anaesthetists found that 36.9% of errors were due to misidentification of drug ampoules, 64.4% of which could be attributed to ampoules having a similar appearance. In addition to 66 errors, 45 near-misses were reported.6 Gordon et al.2 found that fatigue and distraction played a role in 14.1% and 4.7% of errors, respectively, while 10.6% of errors in another study6 could be attributed to the respondent taking medication at the time of the error. Adverse events from errors included hypertension, hypotension, cardiac arrest, tachycardia, bradycardia, prolonged paralysis, and awareness under anaesthesia.2
Doctors in South African hospitals with limited resources and large numbers of patients are often subjected to adverse factors contributing to system, equipment and human errors, which may cause stress and burnout and increase errors in the administration of anaesthesia medication.7-9 We investigated the occurrence of such events in public sector hospitals in the Free State province, that included full-time practising anaesthetists and many doctors who occasionally administer anaesthesia.
Methods
An observational, descriptive study was conducted. Contact information for public hospitals was found on the webpage of the Department of Health.10 The 31 public hospitals in the Free State were approached to participate (the Free State Psychiatric Complex (FSPC) in Bloemfontein was excluded since no anaesthesia is administered there). If no anaesthesia was given at a hospital, it was excluded. The authors phoned the superintendent at each hospital to obtain consent, the number of doctors administering anaesthesia every week, and to identify a doctor who could act as a correspondent for the study.
Only qualified doctors administering anaesthesia participated, which included interns, community service doctors, medical officers, registrars and specialist anaesthetists.
The questionnaire used by Gordon et al.2 was modified for this investigation. It required doctors to provide information including: (i) demographic information on respondents, (ii) information regarding the administration of anaesthesia, (iii) reporting of errors, and (iv) the occurrence of errors during anaesthesia. All respondents completed sections (i) and (ii), while only respondents involved in erroneous drug administration during anaesthesia completed sections (iii) and (iv).
Questionnaires and an explanatory letter were distributed to all anaesthetists in public hospitals in the Free State. The researchers delivered and collected the questionnaires by hand at Bloemfontein based hospitals including National District, Pelonomi Regional and Universitas Academic hospitals. Questionnaires were mailed to designated correspondents at the other hospitals in the province and followed up by telephone if no reply was received within a month after confirmation of receipt of the questionnaires.
Questionnaires were completed anonymously and returned in an unidentifiable, sealed envelope to further ensure confidentiality. Responses were regarded as confidential and used for research purposes only.
A successful pilot study determined the efficiency of the questionnaire and the data, including 5 anaesthetists at Universitas Academic Hospital who did not complete another questionnaire.
Data were captured, transferred to an Excel spreadsheet and accuracy verified before statistical analysis by the Department of Biostatistics, University of the Free State (UFS). The occurrence of errors was analysed and, where possible, stratified for the different groups of participating doctors. Results were summarised as medians for numerical variables, or frequencies and percentages for categorical variables.
Approval to conduct the investigation was obtained from the Ethics Committee of the Faculty of Health Sciences, UFS. Permission was obtained from the Free State Department of Health and the superintendents of the participating hospitals.
Results
Questionnaires were distributed to 188 potential participants at 22 public sector hospitals at 15 health care centres; 87 completed questionnaires were received (46.3% response rate); 3 were eliminated owing to incomplete answers, so giving a final number of 84 questionnaires for analysis.
The period of practice of anaesthesia by participating respondents ranged between 2 months and 30 years, with a median of 36 months; 41 (48.8%) were medical officers, 16 (19.1%) registrars, 16 (19.1%) community service doctors, 6 (7.1%) interns, and 5 (6.0%) were specialists. Table I shows the median number of anaesthetics administered per week by respondents in these categories. Anaesthetics administered ranged from 1 to 100 per week. Overall, a median of 10 anaesthetics was given per week.

The questionnaire requested information regarding respondents' views on and practices in the administration of anaesthesia. None stated that they never read the name of the agent on an ampoule, 3.6% stated that they read the name on the ampoule sometimes, 21.4% most of the time, and 75.0% always read the name on the ampoule; 81.9% of respondents indicated that they performed a repeat control check before administering drugs; 20.2% asked someone else to check the name of the drug on the ampoule with them as control, and 79.8% checked on their own.
Twenty (23.8%) respondents indicated that they were aware of a South African standard for colour-coding syringe labels in the operating theatre, of whom 5 (25%) said that they regularly made use of it. Median responses to questionnaire items dealing with a colourcoded system for labelling of drug ampoules are:
• a standardised colour-coded system of labelling drug ampoules would decrease the incidence of drug errors: strongly agreed
• a standardised colour-coded system of labelling syringes in theatre would decrease the incidence of drug errors: agreed
• havingall syringes labelled with black-on-white labels would decrease the incidence of drug administration errors: moderately agreed.
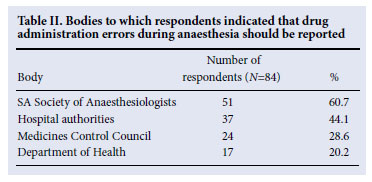
Seventy-eight (92.9%) respondents indicated that they would report anaesthetic drug errors if a single reporting agency for such events existed. Table II shows the results of respondents' suggested bodies to which errors should be reported; 8.3% of respondents recommended other options not listed in Table II, such as reporting the error to a colleague or the Head of the Department of Anaesthesia, and at departmental meetings.
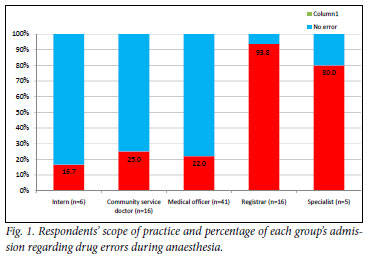
Of the total of 84 respondents, 33 (39.3%) indicated that they themselves or a nurse under their direct supervision administered the wrong drug or fluid to a patient at some point during anaesthesia (Fig. 1).
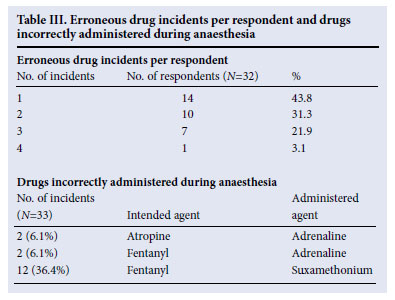
Hereafter, results are based on the 33 respondents who indicated the occurrence of erroneous events during anaesthesia. Table III gives the distribution of incidents by respondents. One respondent did not specify the number of incidents in which he/she was involved. Including this respondent, at least 60 erroneous drug incidents occurred, for which the outcome was specified in 57 (95.0%) cases.
In 29 (50.9%) for which the outcome was recorded (N=57), the incident was of no clinical significance; in 27 (47.4%) immediate intervention was required to prevent harm to the patient. Major morbidity was reported in only one (1.7%) incident, and no fatalities occurred.
More information on the erroneous event was obtained in 52 (86.7%) cases. Drug errors that occurred more than once were identified (Table III); 4 respondents administered a drug into the wrong site at some stage, e.g. into an intravenous (IV) line instead of an epidural catheter.
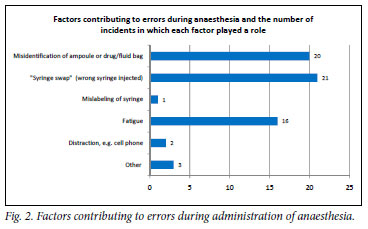
Respondents had to identify one or more factors that they regarded as contributory to their drug errors (Fig. 2). Of the 33 respondents involved in drug errors during anaesthesia, 32 indicated whether or not they reported the error, of whom only 16 (50.0%) reported the error. In 5 (15.6%) cases, the patient was informed postoperatively that an error occurred. One patient initially threatened legal action, although all patients eventually accepted the error without taking further steps.
Discussion
A response rate of 46.3% was obtained (87/188 questionnaires), which was satisfactory compared with the response rate of 18.5% reported by Gordon et al.,2 and similar to the 53% by Llewellyn et al.6
Although anaesthesia was administered most frequently by interns, only 16.7% of them admitted to making an error during anaesthesia. Among respondents who practised anaesthesia full-time, more incidents were reported; 15 (93.8%) of the 16 registrars and 4 (80%) of specialists reported errors during anaesthesia. This finding may reflect the statistical reality that more errors occur when more anaesthetics are administered, but may also indicate reluctance of less-experienced doctors to report or their greater level of vigilance. Llewellyn et al.6 also observed a higher incidence of errors among very experienced doctors administering anaesthesia, and that this could be attributed to them becoming less cautious, with increasing familiarity with the procedure, or being more comfortable regarding honesty about errors and reporting them.6
Most (75.1%) respondents who were involved in errors during anaesthesia reported the occurrence of 1 or 2 incidents (Table III). Although these were of no clinical significance in 50.9% of cases reported, and immediate intervention prevented further harm to the patient in 47.4%, anaesthetists should not be unjustifiably content with the outcomes. Undetected errors might have occurred or could not be ruled out, and only recognised errors could be attended to immediately. Major morbidity occurred in a case when calcium chloride was administered into the spinal cord instead of bupivacaine, resulting in prolonged paralysis and chronic pain syndrome.
The most common drug error involved fentanyl and suxamethonium. In 12 incidents, fentanyl was intended but suxamethonium was administered instead. In one incident, fentanyl was administered when suxamethonium was intended. Fentanyl is an opioid analgesic used in surgical procedures as supplement in total intravenous induction of anaesthesia. Suxamethonium is a depolarising muscle relaxant used intra-operatively. This erroneous drug exchange will result in muscle fasciculations and paralysis. If this mistake is made before the patient is asleep (fentanyl is frequently used pre-induction), the patient may experience paralysis while awake, causing great anxiety. When fentanyl is administered instead of suxamethonium, paralysis required for surgery is not obtained. Gordon et al.2 also found syringe swaps, with fentanyl and suxamethonium the most common drug-related error during anaesthesia.
Gordon et al.2 reported that errors involving vasoactive drugs was of concern; 14% of all drug errors involved vasoactive drugs such as adrenaline; 13 incidents involved vasoactive drugs, yielding 22.8% of the incidents considered.2 Llewellyn et al.6 reported that muscle relaxants were most commonly involved in errors during anaesthesia. In our study, 4 (12.1%) incidents involved the erroneous administration of adrenaline, which can pose serious consequences in patients with hypertension and/or cardiovascular problems (Table III).
The most frequently reported contributions to errors during anaesthesia included syringe swaps, misidentification of drugs, and fatigue (Fig. 2). Although 81.9% of our respondents indicated that they repeated control checks before administering a drug during anaesthesia, it is of concern that 18.1% did not double-check by themselves or with someone else assisting. This omission could be a main reason for the occurrence of syringe swaps. Fatigue that could result in errors was identified as a main contributory factor, especially where two drug names are closely related or the ampoules appear similar. The repeat control check may unintentionally be omitted owing to exhaustion. Misidentification of syringes could be attributed to only 23.8% of respondents being aware of a South African standard for colour coding syringe labels in the operating theatre, which is also not available in these and many other state hospitals. Only a quarter of respondents who were aware of this system used it when administering anaesthesia.
Most (92.9%) of our respondents indicated that they would report errors if a single agency for this purpose existed, whereas Gordon et al.2 reported that only 60% of respondents would do so. More than 60% of our respondents suggested that errors should be reported to the SA Society of Anaesthesiologists.
Most errors (84.5%) were not reported to the patient, which could be attributed to it being of no clinical significance or could be rectified and harm prevented. Further factors could be fear of legal prosecution and that doctors lacked communication skills.11 Doctors may find it difficult to convey bad news to patients and therefore disregard the problem, and most health professionals may be reluctant to admit their mistakes.12 Non-disclosure of this information may aggravate the problem of drug errors since contributing factors and situations cannot be identified and adjusted.
Conclusion and recommendations
Most anaesthetists have been or will be involved in a drug error at some stage. We included non-specialist anaesthetists to determine their incidence of errors. Although most errors were of no clinical significance and all patients recovered completely where intervention was required, all anaesthetists, whether regular or infrequent practitioners, should be aware of the possibility of this problem. Systems can be put in place to reduce drug errors: a standardised colour-coding system would decrease errors, and special attention should be given to drugs that are commonly confused, such as fentanyl and suxamethonium. Specialists and registrars reported the most errors, and interns the least. We deduced that the longer work experience of senior practitioners made them more at ease about admitting their mistakes. A central reporting agency that can collect information regarding errors and identify trends and other factors that can prevent mistakes, may motivate anaesthetists to report errors without fear of prosecution. Communication skills are important and should simplify the reporting of errors to patients and others. Since fatigue plays an important role in many errors, doctors should not work excessively long shifts, and should take precautions when tired, e.g. ask a colleague to perform repeat control checks together. However, working long hours is usually beyond a doctor's control. Rigid practice routines such as the syringe size and colouring for specific drugs, routine double check (with or without a third party), and arrangement of syringes on the work surface may reduce errors. Physicians administering anaesthesia must be aware of the SANS 26825 colour-coded system for syringes approved by the South African Bureau of Standards (SABS) in June 2009. These require labels to be attached to syringes for the correct identification of their contents during anaesthesia.13 Electronic methods may contribute to reducing mistakes in future.
The authors acknowledge the administrative staff of the Department of Anaesthesiology, UFS, for assistance with telephone calls, photocopying and general support; Dr Elzaan Groenewald for suggestions on the report; all correspondents and participants at public sector hospitals in the Free State for their involvement; and Daleen Struwig, medical writer, Faculty of Health Sciences, UFS, for technical and editorial preparation of the manuscript.
References
1. Wheeler SJ, Wheeler DW. Medication errors in anaesthesia and critical care. Anaesthesia 2005;60:257-273. [ Links ]
2. Gordon PC, Llewellyn RL, James MFM. Drug administration errors by South African anaesthetists - a survey. S Afr Med J 2006;96:630-632. [ Links ]
3. Fasting S, Gisvold SE. Adverse drug errors in anesthesia, and the impact of coloured syringe labels. Can J Anaesth 2000;47:1060-1067. [ Links ]
4. Orser BA, Chen RJB, Yee DA. Medication errors in anesthetic practice: a survey of 687 practitioners. Can J Anaesth 2001;48:139-146. [ Links ]
5. Khan FA, Hoda MQ. A prospective survey of intra-operative critical incidents in a teaching hospital in a developing country. Anaesthesia 2001;56:171-182. [ Links ]
6. Llewellyn RL, Gordon PC, Wheatcroft D, et al. Drug administration errors: a prospective survey from three South African training hospitals. Anaesth Intensive Care 2009;37:93-98. [ Links ]
7. Bruce SM, Conaglen HM, Conaglen JV. Burnout in physicians: a case for peer-support. Int Med J 2005;35:272-278. [ Links ]
8. McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 2002;359:2089-2090. [ Links ]
9. Kluger MT, Townend K, Laidlaw T. Job satisfaction, stress and burnout in Australian specialist anaesthetists. Anaesthesia 2003;58:339-345. [ Links ]
10. Department of Health. Contact details of public hospitals in South Africa. Pretoria: Department of Health. http://www.doh.gov.za/hosp_contacts-f.html ( accessed 20 January 2009). [ Links ]
11. Sanson-Fisher R, Maguire P. Should skills in communicating with patients be taught in medical schools? Lancet 1980;2(8193):523-526. [ Links ]
12. Ausman JI. The international disease of doctors. Surg Neurol 1997;48:425-426. [ Links ]
13. South African Bureau of Standards . SANS 26825 (2009). Anaesthetic and Respiratory Equipment- User-applied Labels for Syringes containing Drugs used during Anaesthesia: Colours, Design and Performance. Pretoria: South African Bureau of Standards. https://www.sabs.co.za/content/ uploads/files/06-09.pdf (accessed 1 November 2010). [ Links ]
Accepted 11 November 2010.
Corresponding author: J Diedericks (diedericksbjs@ufs.ac.za)














