Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.4 Pretoria Abr. 2011
EHPBA/ASSA SAGES 2011 12 - 16 April 2011, Cape Town SAGES abstracts
ORAL PRESENTATIONS
SELF-EXPANDING METAL STENTS FOR PALLIATION OF OESOPHAGEAL CANCER - A 4-YEAR REVIEW
Morganayagi GovenderI,II, Lucien FerndaleI,II, Sandie ThomsonI,III
IPietermaritzburg Metropolitan Hospitals - Department of Surgery, Grey's Hospital, KZN
IINelson Mandela School of Medicine, University of KwaZulu-Natal
IIIUniversity of Cape Town; Surgical Research Society
BACKGROUND: Endoscopic placement of self-expanding metal stents (SEMS) is widely used for palliation of dysphagia in patients with inoperable malignant oesophageal lesions. This study was undertaken to document the periprocedural experience with a pure endoscopic placement technique.
PATIENTS AND METHODS: Retrospective analysis of all patients stented for oesophageal cancer at the GI Unit at Grey's Hospital, Pietermaritzburg, over a 4-year period (2007 -2010). Data were analysed from completed procedure forms and included demographics, tumour length, the presence of fistulas, stent size and complications. Stenting was performed without radiological guidance. At endoscopy the oesophageal lesion was dilated over a guidewire, the stent passed over the wire and positioned and deployed under direct endoscopic vision.
RESULTS: A total of 394 stents were inserted over a 4-year period, 27 for benign and 367 for malignant disease. There were 347 patients in the malignant group, 30 of whom required repeat stenting. Of the 347 patients, 142 (40.9%) were female and 205 (59.1%) male. The mean age was 60 years (range 38 -101). Of the patients 328 were black (94.5%), 15 white (4.2%) and 4 Indian (1.3%).
The reasons for palliative stenting were distributed as follows: age >70 - 67 patients; tumour length >8 m - 102; presence of tracheooesophageal fistula - 23; unspecified - 142. There was also one patient who had metastases, another who refused surgery, and one stent for post-oesophagectomy leak.
Of those requiring repeat stenting, 8 had stent migration, 10 proximal tumour overgrowth, 10 distal tumour overgrowth, 1 a blocked stent and 1 a stricture. Only 3 complications were recorded (0.9%) - 2 iatrogenic tracheo-oesophageal fistulas and 1 false tract created through a long lesion. All 3 were nevertheless successfully stented.
CONCLUSION: The number of patients seen with inoperable oesophageal cancer at Grey's Hospital is sizeable. The average annual load of palliative stents is 90 patients. Pure endoscopic SEMS placement is a viable and safe option with a low periprocedural complication rate. It forms the core of palliative care for patients with dysphagia, with or without fistulas. Recurrent dysphagia can still be effectively managed by restenting. More detailed follow-up is required to assess the long-term efficacy of SEMS in our setting. A prospective analysis, including quality of life surveys, is planned.
Outcome of endotherapy in bleeding peptic ulcer patients at Groote Schuur Hospital
Dion LevinI; Gillian WatermeyerI; Eduan DeetlefsI; David MetzII; Sandie ThomsonI
IUniversity of Cape Town
IIUniversity of Pennsylvania, USA
INTRODUCTION: Endotherapy is highly effective at controlling bleeding from peptic ulceration.
AIMS: To assess the efficacy of endoscopic intervention for high-risk bleeding peptic ulcer disease and benchmark our surgical and mortality rates, for current and future comparison.
METHODS: 227 patients with high-risk peptic ulcers underwent therapeutic intervention (adrenalin injection) between January 2004 and December 2009 (median age 57 years (range 19 -87); 60.4% males).
RESULTS: Primary endoscopic haemostasis failed in 51/227 patients (22.5%); 8 patients underwent surgery, of whom 1 died; 5 patients were deemed unfit or died prior to further intervention; 38 patients underwent second endoscopic endotherapy, and 10 of these underwent surgery, of whom 3 died; 24 patients had successful second endotherapy; and 18/227 patients (7.9%) required surgery for bleeding not controlled at initial (44.4%) or second endoscopy (56.6%). Surgical patients had a higher Forrest classification (odds ratio (OR) 0.4 (2a/2b v. 1a/1b), p=0.01) and required more blood (OR 1.4, p=0.0001), but demonstrated no difference in mortality. Overall 30 patients (13.2%) died, 5.3% by day 3 and 7.9% by day 30; 4 patients died after surgery, 2 by day 3 and 2 by day 30; and 16 patients, all of whom had significant co-morbid medical conditions, died after successful primary endotherapy. Rebleeding was the only predictor of death in patients who died at day 3 (OR 14.9, 95% confidence interval (CI) 2.6 - 83.4). A high Rockall score was the only predictor of death at day 30 (OR 2.09, 95% CI 1.3 - 3.17).
CONCLUSION: Our overall benchmark mortality is 13.2% and surgical mortality 22%. More than half of the patients who died did so as a result of medical co-morbidity, despite successful primary endotherapy. Our rate of failed primary endoscopic haemostasis is 22.5%. Rebleeding after primary endoscopic intervention is a predictor of death at day 3. This study supports the use of the Rockall score to predict mortality at day 30.
Amylase and alanine transaminase levels as discriminators of aetiology in an urban South African population with acute pancreatitis
Zaheer Moolla; Frank Anderson; Sandie Thomson
University of KwaZulu-Natal, Durban
INTRODUCTION: In acute pancreatitis (AP), serum elevations of amylase and alanine transaminase (ALT) have been shown in Western series to be predictive of aetiology. We analysed these predictors in the context of a South African cohort which includes antiretroviral therapy and hypertriglyceridaemia.
MATERIALS AND METHODS: A prospectively collected database of 386 AP patients admitted to Addington Hospital, Durban, between 2001 and 2008, was analysed. The relationship between admission amylase or ALT and aetiology based on history, abdominal ultrasound and serum triglycerides was studied: 238 patients (17 females) were admitted with acute alcoholic pancreatitis (AAP), 76 (21 males) with acute gallstone pancreatitis (GSAP), 42 (15 males) with pancreatitis secondary to antiretroviral therapy (ARVAP) and 30 (4 males) with AP due to hypertriglyceridaemia (HAP).
RESULTS: The levels according to aetiology are set out in the table.

Amylases and ALT levels in GSAP were significantly higher than those for all other aetiologies and were similar for non-biliary causes. An ALT level of >56 U/l had a sensitivity of 71%, a specificity of 80% and a negative predictive value of 91% for gallstones.
CONCLUSION: GSAP average amylases were double those for other aetiologies. A normal ALT was highly predictive of non-gallstone aetiology. Neither amylase nor ALT could help differentiate the other aetiologies.
Cox-2 and pparg expression in colorectal cancer: a role for inflammation?
Mary Ngaira; Ernst Fredericks; Gill Dealtry; Saartjie Roux
Nmmu, Port Elizabeth, South Africa
BACKGROUND: In 2010 we showed that PPARg, a nuclear receptor involved in cell signalling and promoting normal differentiation, is 7.5-fold down-regulated in colorectal cancer (CRC) patients compared with normal. Inflammation and oxidative stress can modulate PPARg expression. Inflammation could therefore be one of the important causes of CRC as indicated by the higher incidence of CRC among inflammatory bowel disease (IBD) patients.
AIM: To investigate the role of COX-2 as a marker of inflammation in the pathogenesis of CRC.
METHOD: Colon biopsies of 99 patients in the following groups: control, IBD (Crohn's and ulcerative colitis (UC) - inflammatory group) and irritable bowel syndrome (IBS) (diarrhoea (D) or constipation (C) predominant - non-inflammatory group). Immunohistochemical analysis was performed and compared with PPARg qPCR.
RESULTS: A striking increase in COX-2 protein expression was observed in the lamina propria of CRC patients, as previously reported. In the IBD group, UC patients had higher total COX-2 expression in both lamina propria and epithelial cells compared with Crohn's disease patients, regardless of treatment. Surprisingly, D-IBS patients had significantly higher (p<0.01) COX-2 expression in the epithelial cells than the control group, unlike the C-IBS group. The reason for this is not clear.
Although the CRC patients had raised COX-2 expression in the epithelial cells as well as the lamina propria and low PPARg expression, a direct relationship between PPARg and COX-2 expression could not be established in the other colorectal pathologies investigated.
CONCLUSION: Our surprising observation of low COX-2 expression in IBD patients is supported by Vong et al., 2010. This partially explains the exacerbation of IBD when treated with COX-2 inhibitors. The pathogenesis of CRC is not necessarily COX-2 driven, but may involve other cytokines. It is clear that more research is needed on the regulation of the different cytokines and homeostatic control of the colon environment.
POSTER PRESENTATIONS
Identifying families with lynch syndrome in South Africa
S MacaulayI; J F BothaII; A KrauseIII
INational Laboratory Service, Johannesburg
IIUniversity of the Witwatersrand, Johannesburg
IIISandton Medi-Clinic, Johannesburg
BACKGROUND: Lynch syndrome (hereditary non-polyposis colorectal cancer (HNPCC)) is an autosomal dominant condition predisposing individuals to the development of colorectal and endometrial cancers as well as stomach, hepatobiliary, small-bowel and central nervous system cancers. Lynch syndrome occurs as a result of mutations in one of four main genes (MLH1, MSH2, MSH6 and PMS2) involved in the DNA mismatch repair pathway.
AIM: The study aimed to highlight the necessary steps clinicians and genetic counsellors need to take in order to assess the likelihood and then confirm a diagnosis of Lynch syndrome. We present cases of South African Caucasian families in whom a diagnosis of Lynch syndrome was suspected.
METHODS: Baseline analysis involved drawing the family pedigree. On the basis of the family history alone it can be determined whether or not a family is at high risk for a genetic cancer syndrome.
Secondly, immunohistochemistry (IHC) analysis on histology blocks was performed. In an ideal situation, microsatellite instability analysis should also be performed; however, this is not available in South Africa, so IHC in conjunction with pedigree analysis is relied upon. IHC has its own limitations and the interpretation of results requires technical expertise.
Thirdly, diagnostic genetic testing was performed on patients' DNA once the work-up suggested a likely diagnosis of Lynch syndrome.
RESULTS: In one family a novel MSH2 mutation was identified (c. 1811C>A). Extensive IHC and genetic testing was required in order to confirm its pathogenicity. Another family had a rare MSH6 (c. 644dupT) mutation identified.
CONCLUSION: Genetic counselling is important in baseline pedigree ascertainment and risk assessment. It also serves an important role in educating and informing such families about the condition and providing options for genetic testing and management. These cases illustrate the complex process of confirming and managing Lynch syndrome in South African families.
Case report: upper gastro-intestinal kaposi's sarcoma in an hiv-positive patient without cutaneous disease as a cause for anaemia and abdominal pain
Nazeer Ahmed Chopdat; Reidwaan Ally
African Institute of Digestive Disease, Soweto, Johannesburg
BACKGROUND: In June 2010 a 31-year-old woman was referred to our outpatient clinic. She had been diagnosed with HIV 1 month before her referral. She complained of constant abdominal pain, and difficulty and pain on swallowing. She had lost 10 kg over the past month. On physical examination she was wasted, pale and weak. She had generalised lymphadenopathy and oral thrush. No evidence of cutaneous karposis sarcoma lesions was seen.
INVESTIGATION AND MANAGEMENT: Laboratory investigations revealed an albumin level of 11 g/l, a haemoglobin concentration of 7.8 g/ dl and a normal mean cell volume of 85 fl. The CD4 count was 95 cells/µl. The patient underwent oesophago-gastro-duodenoscopy which revealed oesophageal candidiasis and multiple plaque-like lesions. Histological examination and immunohistochemistry of the biopsy specimens were consistent with Kaposi's sarcoma, positive nuclear staining for HHV 8 and Helicobacter pylori-associated chronic gastritis. The patient was started on eradication therapy, referred for highly active antiretroviral therapy (HAART) and sent to a specialised oncology unit to commence chemotherapy. She was, however, lost to follow-up.
DISCUSSION: Infection with HIV results in a wide range of opportunistic infections and tumours, commonest of which is Kaposi's sarcoma. Gastro-intestinal Kaposi's sarcoma is usually most common in patients with extensive cutaneous disease; however, mucosal involvement without cutaneous involvement, though rare, has been described. We might well have attributed our patient's symptoms to candidiasis, and had we not performed endoscopy we would have failed to diagnose the gastro-intestinal Kaposi's sarcoma.
CONCLUSION: Biopsy of all suspicious lesions is necessary in HIV-positive patients. Early diagnosis of gastro-intestinal Kaposi's sarcoma is desirable from prognostic and therapeutic points of view. Symptoms may resolve and progression of disease be delayed with HAART and chemotherapy.
We therefore recommend early endoscopy in all patients with HIV who have persistent upper gastro-intestinal symptoms.
Dietary intake and total dietary fibre intake in patients with irritable bowel syndrome
C Stevenson; E Fredericks; R Theunissen; G Dealtry; S Roux
Nelson Mandela Metropolitan University, Port Elizabeth, E Cape
INTRODUCTION: In the USA and the European Union, adult dietary fibre intake falls well below the recommended range of 20 -35 g per day. Poor fibre intake is reflected in altered gut microbiota and short-chain fatty acid production.
AIM: To assess the dietary intake of patients with irritable bowel syndrome (IBS) and compare this with healthy controls and international recommendations (dietary reference intakes, DRIs).
METHODS: Three-day estimated food records were obtained from 26 C-IBS, 10 D-IBS and 21 controls.
RESULTS: Total energy intake and macronutrient distribution did not differ significantly between the groups. Total protein and carbohydrate consumption was higher than the recommended DRIs in all three groups. Fat intake was higher than the acceptable DRI range of 20 -35% for the D-IBS group (D-IBS 37.59%, C-IBS 35.26%, controls 33.46%). Total dietary fibre intake did not reach the recommended intake for all three groups, but was higher in the control group than both the C-IBS and D-IBS groups (D-IBS 13.64 g, C-IBS 14.59 g, controls 16.73 g, p=0.363). Intakes of insoluble and soluble dietary fibre were low in all three groups, but the controls had a better intake than either of the IBS groups (insoluble fibre D-IBS 3.68 g, C-IBS 3.48 g and controls 5.01 g, p=0.126; soluble fibre D-IBS 2.66 g, C-IBS 2.71 g and controls 3.83 g, p=0.111). The D-IBS group had a statistically significant lower intake of vitamin A compared with the C-IBS and control groups (D-IBS 411.80 RE, C-IBS 695.76 RE, controls 893.97 RE, p=0.06) and significantly lower intakes of total carotenoids, A-carotene and B-carotene.
CONCLUSION: This study highlighted that IBS patients did not meet recommendations for fibre intake and that intake was poor. The D-IBS group had an insufficient intake of vitamin A and carotenoids. This is similar to the findings of Aller et al. (2004), and warrants further research.
Over-the-counter sale of non-steroidal anti-inflammatory drugs should be banned!
Theshni Govender; Martin Brand
University of the Witwatersrand, Johannesburg
BACKGROUND: Non-steroidal anti-inflammatory drugs (NSAIDs) are known for their complications. The US FDA issued a ruling in 2009 that made it compulsory to list the gastro-intestinal and cardiac side-effects of NSAIDs on all NSAID packaging. Large proportions of patients admitted to our hospital with upper gastro-intestinal (GIT) complaints are users of NSAIDs, and appear to be unaware of their significant side-effects. It is of concern that in South Africa NSAID preparations are freely available over the counter.
METHODS: We performed a retrospective study from 1 January 2010 to 31 December 2010 at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH). All patients who were admitted with an upper GIT complaint, and subsequently underwent oesophagogastro-duodenoscopy or a surgical procedure and who did not have portal hypertension, were included. We used a university-associated hospital's cost structure, including hospital and doctors' fees, to calculate the cost of these NSAID-associated upper GIT complications.
RESULTS: In 2010, 163 patients were admitted with epigastric pain, upper GIT haemorrhage or perforation. Of 94 patient files collected to date, 36 confirmed NSAID use. Of these patients, 4 underwent laparotomy.
Each of such admissions cost R20 520, which included only the following: 4 days in a general ward, consultation fees and oesophagogastro-duodenoscopy, and excluded intensive care unit admission and blood products. Each patient who required a laparotomy accrued a cost of R88 800. The estimated cost for these 36 patients was R1 093 920.
CONCLUSION: The cost to the CMJAH associated with NSAID use is substantial. This may be minimised by making NSAIDs available on prescription only.
Questran colonic crystal: bystander or offender?
Kgaogelo MoengI,II; Adam MahomedI,II
IUniversity of the Witwatersrand, Johannesburg
IICharlotte Maxeke Johannesburg Academic Hospital, Johannesburg
AIM: To report on a rare but previously described gastrointestinal complication of a commonly used anion exchange resin, cholestyramine, and to explore the possibility of this agent's being a cause of mucosal lesions.
CASE SUMMARY: A 32-year-old immunocompromised patient was found to have colonic mucosal crystal deposits on histopathological specimens while being investigated for chronic diarrhoea. The mucosal biopsies were obtained after the patient had been treated with Questran 4 g 3 times a day for 6½ days. Endoscopy revealed associated fungating, ulcerating lesions with necrotic areas. An additional diagnosis of MTB was made from specimens obtained.
DISCUSSION: Ion exchange resins are commonly used in clinical practice, with not many reported complications. Kayexalate and kalimate, the cation exchange resins used to treat hyperkalaemia, and cholestyramine (Questran), a bile-acid-binding anion exchange resin, have all been previously described as potential causes of gastrointestinal mucosal crystal deposits. While kayexalate and kalimate have both been found to cause mucosal ulceration, haemorrhage and necrosis, there is a paucity of information regarding such lesions in relation to cholestyramine. Our patients had tuberculosis of the colon, which could have been the cause of the ulcerating lesions found at endoscopy.
CONCLUSION: Ion exchange resins can cause gastro-intestinal mucosal crystal deposition in some patients. It is, however, not clear whether cholestyramine causes mucosal lesions in addition to crystal deposition. Our patient had MTB, which could potentially have caused the mucosal lesions.
Jaundice as an unusual presentation of Hodgkin's Lymphoma in a patient with tuberculosis
Mfanufikile NomveteI,II; Keith NewtonI,II; VG NaidooI,II; Sadia SaeedII
IUniversity of KwaZulu-Natal, Durban
IIInkosi Albert Luthuli Central Hospital, Durban
INTRODUCTION: Cholestatic jaundice is a rare paraneoplastic complication of Hodgkin's lymphoma.
CASE: A 36-year-old black man was started on antituberculosis (TB) therapy at a peripheral hospital on an unclear basis. Cholestatic jaundice preceded the commencement of the anti-TB treatment and persisted despite discontinuation of the therapy. He had no risk factors for chronic liver disease, and presented with pruritus, dark urine and normal stools. Physical examination revealed deep jaundice, pallor, cervical lymphadenopathy, 4 cm hepatomegaly and 2 cm splenomegaly. Laboratory results showed a total bilirubin level of 384.5 µmol/l (conjugated 276.7 µmol/l), alkaline phosphatase 681 U/l, gamma-glutamyl transferase 107 U/l, and alanine transferase 130 U/l. A chest radiograph was normal and an abdominal ultrasound scan confirmed hepatosplenomegaly and displayed no features of biliary obstruction or lymphadenopathy. A magnetic resonance cholangiopancreatogram was equivocal and an endoscopic retrograde cholangiopancreatogram revealed no biliary obstruction. Sputa were positive for acid-fast bacilli (AFB) and confirmed to be drug sensitive, so anti-TB treatment was re-instituted. A liver biopsy revealed homeostasis, no granulomas or AFB and no neoplastic infiltrate, and 6-week TB culture was negative. Hodgkin's lymphoma (HL) was diagnosed on a lymph node biopsy and subsequent bone marrow biopsy. A staging computed tomography scan revealed intraabdominal lymphadenopathy, but none at the porta hepatis or peripancreatic area. Following successful chemotherapy for the HL, the patient's liver function test results normalised.
DISCUSSION: Cholestatic jaundice is an uncommon presentation of HL. Mechanisms involved usually include hepatic tumour infiltration, portal tract destruction or biliary tree obstruction, or the condition is secondary to chemotherapy. Very rare is idiopathic cholestasis, which is thought to be mediated by inflammatory cytokines that alter the functioning of the bile salt exporter proteins. This paraneoplastic syndrome improves after treatment of the lymphoma.
CONCLUSION: Unexplained cholestasis should be carefully assessed to exclude an underlying potentially treatable systemic disorder.
Massive and multi-organ intraabdominal hydatid disease: case report
Orlando Zamora Santana
Nelson Mandela Academic Hospital, Mthatha, E Cape, and Enriquez Academic Hospital, Havana, Cuba
Hydatid disease is endemic in the Middle East as well as other parts of the world such as India, Africa, South America, New Zealand, Australia, Turkey and southern Europe. Hydatid cysts can occur in any organ, but infestation most commonly occurs in the liver, followed by the lung.
A 25-year-old man presented with a 3-year history of vague abdominal pain and progressive swelling of the abdomen. Clinical examination revealed non-tender firm masses in the abdomen. The liver was palpable, reaching about 10 cm below the costal margin. Rectal examination revealed globular masses in the pouch of Douglas.
We present the investigations done and our surgical findings and results.
It is important to emphasise that this disease should be suspected in patients with cystic lesions affecting any organ, especially in endemic areas of the world.
The spectrum of the operative management of acute appendicitis at a district hospital
Muhammed Zaki Shaik; Sandie R Thomson
Nelson R Mandela School of Medicine and Addington Hospital, Durban
BACKGROUND: In the era of the active adoption of laparoscopy, the spectrum of operative options employed in the management of suspected acute appendicitis in the state sector has not been well studied. We utilised a highly accurate prospective operative database to document and analyse current practice.
METHODS: Data from the first 2 years were extracted and analysed from the Addington Hospital operative electronic database. Demographics, hospital stay, operative time, conversion rate, primary surgeon (registrar versus consultant), mortality and relaparotomy were extracted for the patients according to the surgical management (Lanz incision appendectomy, laparoscopic appendicectomy and laparotomy for complicated appendicitis). Statistical analysis was done using a two-sample t-test.
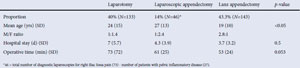
RESULTS: There were a total of 322 operations for appendicitis from 2009 to 2010.
In the laparotomy group, 3 patients had a right hemicolectomy. The rest were appendectomies with peritoneal toilet. Fifteen patients required relaparotomies, and 5 patients died. The age difference between the Lanz group and laparoscopic group was significant. Of the diagnostic laparoscopies for right iliac fossa pain, 63% (46/73) were diagnostic for appendicitis. The rest were diagnostic for pelvic inflammatory disease (PID). Eighteen operations were done by registrars. Five of the laparoscopic approaches were converted to laparotomy.
CONCLUSION: Advanced-stage appendicitis managed by laparotomy remains common, with associated morbidity and mortality. It results in double the hospital stay and an increased operating time when compared with the other two operative methods, for which hospital stay and operative times are similar. The utility of laparoscopy in differentiating acute appendicitis from PID is supported and is reflected in the increased female/male ratio in this treatment group.
Case report: the cystic spleen - a diagnostic dilemma
Mohamed Feroz Suliman; Nazeer A I Chopdat; Sunil Philip; Reid Ally
Chris Hani Baragwanath Hospital, Johannesburg, and African Institute of Digestive Diseases, Johannesburg
BACKGROUND: In October 2010 a 45-year-old woman was referred to our hospital with a history of left upper quadrant pain and increasing swelling over the past 6 months. She denied any weight loss, night sweats or dyspeptic symptoms. She had a loss of appetite, intermittent nausea and vomiting but no diarrhoea. She had no previous medical, surgical or travel history. She denied any recent trauma, but on re-evaluation after obtaining her histology results we learned that she had been involved in a bomb explosion a few months previously while working in a laboratory. On physical examination she was found to be generally in good health. There was a mass in the left upper quadrant, with an asymmetrical abdomen.
SPECIAL INVESTIGATIONS AND MANAGEMENT: An ultrasound scan revealed a large splenic cyst, and a computed tomography scan of the abdomen a 10x15x11 cm cystic lesion within the spleen.
Routine laboratory tests including hydatid serology were negative. The patient was taken to theatre for splenectomy. The rest of the abdomen was normal. Histological examination revealed a 10x15x11 cm pseudocyst lined with fibrin and filled with fibrinous material. The remainder of the spleen measured 5x5x8 cm and contained smaller pseudocysts with fibrin. No granulomatous inflammation, neoplasia or echinococcus infection was identified.
DISCUSSION: Pseudocysts of the spleen are classified as secondary cysts, which account for 70 -80% of non-parasitic splenic cysts. They have thick collagenous walls with shaggy haemorrhagic centres containing brown/greenish-brown fluid. The risk of rupture increases with a size greater than 5 cm.
CONCLUSION: This case suggests that traumatic splenic injury should always be considered as a differential diagnosis in patients with large splenic cysts.