Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.4 Pretoria abr. 2011
SAMJ FORUM
CLINICAL PRACTICE: POLICY
Routine cryptococcal antigen screening for HIV-infected patients with low CD4+ T-lymphocyte counts - time to implement in South Africa?
Joseph N Jarvis; Thomas S Harrison; Nelesh Govender; Stephen D Lawn; Nicky Longley; Tihana Bicanic; Gary Maartens; Francois Venter; Linda-Gail Bekker; Robin Wood; Graeme Meintjes
Cryptococcal meningitis (CM) is a major cause of death among HIV-infected individuals. It causes an estimated 957 900 cases and 624 700 deaths worldwide annually, the vast majority of them in sub-Saharan Africa.1 In Cape Town, CM is now the most common cause of adult meningitis (63% of all microbiologically confirmed cases2), and acute outcomes are poor.3 Even with optimal treatment in study settings, 10-week mortality rates are between 24% and 37%.4,5 In 2009, in a routine care setting at an urban hospital in Johannesburg, 67% of patients had died or were lost to follow-up at 3 months (N Govender et al., unpublished data). Unfortunately almost half of South African patients still receive sub-optimal initial treatment with oral fluconazole rather than intravenous amphotericin B.3,6 Clearly, given the substantial mortality and morbidity associated with CM, preventive interventions should be prioritised.
As CM primarily affects patients with CD4+ T-cell counts < 100 cells/µl, the incidence should fall during scale-up of antiretroviral therapy (ART) programmes, as in the high-income countries.7 However, despite recent progress in expanding access to ART in South Africa,8 the median CD4+ T-cell count of patients initiating ART remains low, and a high risk of new AIDS events and mortality persists during the first months of ART.9 Numbers of CM cases in Cape Town remained constant between 2003 and 2008 despite a large increase in ART coverage,10 and national surveillance shows slight increases in the incidence of reported CM cases year on year.11
With expanding ART access, an increasing proportion of CM diagnoses occur among patients already receiving ART - 20% in a cohort of CM patients from Cape Town.12 Most of these patients had recently initiated ART (median duration 41 days), and their in-hospital mortality was high (29%).12 CM is therefore a leading contributor to the high early mortality in African ART programmes. It accounts for up to 20% of all deaths,9 many of which are thought to be due to 'unmasking' cryptococcal disease among patients who had sub-clinical disease when starting ART.13,14
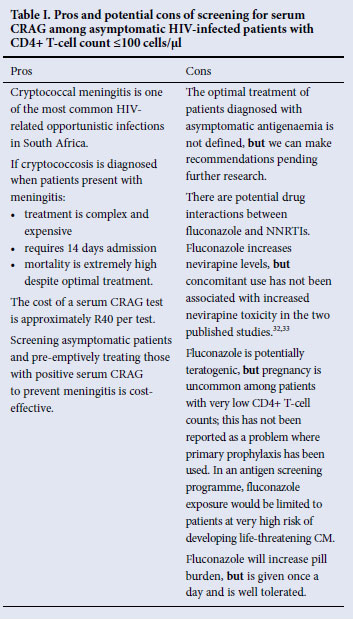
To date, preventive strategies have consisted of routine fluconazole primary prophylaxis for all patients with low CD4+ T-cell counts. Although this approach reduces the incidence of CM,15 concerns exist: fluconazole resistance may develop with widespread use;16,17 it is not cost-effective;18-21 it is teratogenic; and fluconazole has potential interactions with both ART and tuberculosis (TB) medication (Table I). These issues have led to very limited uptake of fluconazole primary prophylaxis in HIV treatment programmes.
Fortunately, research has demonstrated that nearly all patients at risk of developing CM during ART could be identified on entry into ART programmes by screening for sub-clinical infection using cheap (ZAR38.95), simple and highly sensitive cryptococcal antigen (CRAG) blood tests.22 In 707 patients initiating ART in Cape Town, stored serum samples from 13% of patients with CD4+ T-cell counts <100 cells/µl tested positive for CRAG in a retrospective analysis. Prospective screening for CRAG in this cohort would have been 100% predictive of subsequent development of CM within the first year of treatment.22 If identified prospectively, such patients could be given 'pre-emptive' treatment to prevent progression from cryptococcal antigenaemia to life-threatening meningitis. Such a 'targeted' prevention strategy would avoid many potential problems of widespread fluconazole use with a blanket primary prophylaxis approach.
Cape Town data also show that 73% of ART-naïve patients presenting with CM have already been diagnosed with HIV, a median of 4 months before CM, but developed disease before starting ART.23 CRAG screening could also identify these patients, allowing for pre-emptive therapy and fast-tracking for rapid ART initiation - an issue of particular priority given the exceptionally high mortality of South African patients in this pre-treatment period.24-26 If all patients who had previously tested HIV-positive (both those on ART and the 73% who were known to be HIV-positive but not on ART) had been screened, and effective interventions given, up to 78% of cases of CM could have been prevented.
CRAG screening directed at all newly diagnosed HIV-positive patients with CD4+ T-cell counts <100 cells/µl is likely to detect most cases. At a programmatic level, plasma from ethylenediaminetetraacetic acid (EDTA) samples sent for CD4 count testing could automatically be tested for CRAG at the laboratory if the CD4+ T-cell count was <100 cells/µl for the first time in that individual, and in the future, development of point-of-care CRAG tests could allow testing at the clinic level, greatly simplifying the process.
The optimal treatment of asymptomatic CRAG-positive patients has not been studied. Natural history data from Cape Town suggest that ART alone is sufficient to clear asymptomatic antigenaemia in around 50% of cases.22 However, the remaining 50% are at very high risk of developing symptomatic CM and death, so proactive management is needed. One approach would be to perform lumbar punctures for examination of cerebrospinal fluid on all antigenaemic patients to assess for CNS involvement. However, this may not be necessary among asymptomatic patients, would heavily burden an overstretched public health service, and would potentially render a screening programme unworkable. A more pragmatic strategy is to treat all asymptomatic antigenaemic patients with fluconazole according to dosing recommendations in national guidelines: 400 mg daily for 8 weeks followed by fluconazole 200 mg daily for at least 10 months (or until the CD4+ T-cell count rises to >200 cells/µl) and starting ART after the initial 2 weeks of fluconazole. Evidence that higher doses of fluconazole are more rapidly fungicidal27 may change this dosing schedule in future to 800 mg daily for 8 weeks followed by 400 mg daily for at least 10 months. However, evidence to support empiric treatment of CRAG antigenaemia without CSF analysis is lacking, and studies are required. Whether CRAG titres could be used to stratify risk of progression to CM and guide treatment decisions and optimal timing of ART initiation in such patients must also be defined.
The reduction in morbidity and mortality, and the potential economic benefits of a screen-and-treat prevention strategy, are substantial.28 In a cohort of South African patients starting ART, 31% of inpatient admission days within the first 32 weeks of ART were due to CM.29 Each patient admission with CM is estimated to cost ZAR20 980 (at 2001 costing).30 A cost-effectiveness analysis in Uganda, where CRAG testing costs four times more than in South Africa, suggested a cost of only US$190 for each case of CM prevented, and US$266 for each life saved.31 Using data from a retrospective study of a South African cohort, 52 patients with CD4 counts <100 cells/µl initiating ART would have to be screened to prevent one case of CM.22 At the current cost of ZAR39.85 (National Health Laboratory Service tariff), it would cost ZAR2 072 per case of CM prevented22 - substantially less than the cost of hospital admission. But while evidence for the utility of CRAG screening to identify patients at risk of CM is compelling, key questions remain of how best to implement a screening policy and how to manage the asymptomatic CRAG-positive patients identified.
Further studies are planned to clarify these unresolved questions. However, we believe that the strength of the available evidence, coupled with the high ongoing mortality secondary to CM among South African HIV-positive patients, justifies implementation of CRAG screening in the South African HIV programme. This should involve a CRAG test on all patients diagnosed with HIV with a CD4+ T-cell count <100 cells/µl and treating all antigenaemic patients with fluconazole.
JNJ, SDL and GM are funded by the Wellcome Trust, London, UK.
1. Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 2009;23(4):525-530. [ Links ]
2. Jarvis JN, Meintjes G, Williams A, Brown Y, Crede T, Harrison TS. Adult meningitis in a setting of high HIV and TB prevalence: findings from 4961 suspected cases. BMC Infect Dis 2010;10(1):67. [ Links ]
3. Lessells R, Mutevedzi P, Heller T, Newell ML. Poor long-term outcomes from cryptococcal meningitis in rural South Africa. S Afr Med J 2011;101:251-252 (this issue). [ Links ]
4. Bicanic T, Meintjes G, Wood R, et al. Fungal burden, early fungicidal activity, and outcome in cryptococcal meningitis in antiretroviral-naive or antiretroviral-experienced patients treated with amphotericin B or fluconazole. Clin Infect Dis 2007;45(1):76-80. [ Links ]
5. Bicanic T, Wood R, Meintjes G, et al. High-dose amphotericin B with flucytosine for the treatment of cryptococcal meningitis in HIV-infected patients: a randomized trial. Clin Infect Dis 2008;47(1):123-130. [ Links ]
6. Govender N, Cohen C, Meiring S, et al. Trends in treatment of adults with incident cryptococcosis, South Africa, 2005 to 2008. 17th Conference on Retroviruses and Opportunistic Infections, San Francisco, 6-19 February 2010 (abstract 800). [ Links ]
7. Mirza SA, Phelan M, Rimland D, et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992-2000. Clin Infect Dis 2003;36(6):789-794. [ Links ]
8. World Health Organization. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector: progress report. Geneva 2007 (April). http://www.who.int/hiv/toronto2006/towardsuniversalaccess.pdf (accessed 25 January 2011). [ Links ]
9. Lawn S, Harries A, Anglaret X, Myer L, Wood R. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS 2008;22(15):1897-1908. [ Links ]
10. Jarvis JN, Boulle A, Loyse A, et al. High ongoing burden of cryptococcal disease in Africa despite antiretroviral roll out. AIDS 2009;23:1181-1185. [ Links ]
11. Govender N, Cohen C, eds. Group for Enteric, Respiratory and Meningeal disease Surveillance in South Africa. GERMS-SA. Annual Report 2009. http://www.nicd.ac.za/units/germs/germs.htm (accessed 8 January 2011). [ Links ]
12. Jarvis JN, Meintjes G, Harrison TS. Outcomes of cryptococcal meningitis in antiretroviral naive and experienced patients in South Africa. J Infect 2010;60(6):496-498. [ Links ]
13. Lawn SD, Bekker LG, Myer L, Orrell C, Wood R. Cryptococcocal immune reconstitution disease: a major cause of early mortality in a South African antiretroviral programme. AIDS 2005;19(17):2050-2052. [ Links ]
14. Haddow LJ, Colebunders R, Meintjes G, et al. Cryptococcal immune reconstitution inflammatory syndrome in HIV-1-infected individuals: proposed clinical case definitions. Lancet Infect Dis 2010;10(11):791-802. [ Links ]
15. Chang LW, Phipps WT, Kennedy GE, Rutherford GW. Antifungal interventions for the primary prevention of cryptococcal disease in adults with HIV. Cochrane Database Syst Rev 2005(3):CD004773. [ Links ]
16. Goldman M, Cloud GA, Smedema M, et al. Does long-term itraconazole prophylaxis result in in vitro azole resistance in mucosal Candida albicans isolates from persons with advanced human immunodeficiency virus infection? The National Institute of Allergy and Infectious Diseases Mycoses Study Group. Antimicrob Agents Chemother 2000;44(6):1585-1587. [ Links ]
17. Apisarnthanarak A, Mundy LM. The impact of primary prophylaxis for cryptococcosis on fluconazole resistance in Candida species. J Acquir Immun Defic Syndr 2008;47(5):644-645. [ Links ]
18. John L, Nelson M. Primary prophylaxis for cryptococcal meningitis. HIV Med 2004;5(3):131-132. [ Links ]
19. Scharfstein JA, Paltiel AD, Freedberg KA. The cost-effectiveness of fluconazole prophylaxis against primary systemic fungal infections in AIDS patients. Med Decis Making 1997;17(4):373-381. [ Links ]
20. Yazdanpanah Y, Goldie SJ, Paltiel AD, et al. Prevention of human immunodeficiency virus-related opportunistic infections in France: a cost-effectiveness analysis. Clin Infect Dis 2003;36(1):86-96. [ Links ]
21. Freedberg KA, Scharfstein JA, Seage GR, 3rd, et al. The cost-effectiveness of preventing AIDS-related opportunistic infections. JAMA 1998;279(2):130-136. [ Links ]
22. Jarvis JN, Lawn SD, Vogt M, Bangani N, Wood R, Harrison TS. Screening for cryptococcal antigenemia in patients accessing an antiretroviral treatment program in South Africa. Clin Infect Dis 2009;48(7):856-862. [ Links ]
23. Jarvis JN, Meintjes G, Wood R, Harrison TS. Testing but not treating: missed opportunities and lost lives in the South African antiretroviral therapy programme. AIDS 2010;24(8):1233-1235. [ Links ]
24. Lawn SD, Myer L, Orrell C, Bekker LG, Wood R. Early mortality among adults accessing a community-based antiretroviral service in South Africa: implications for programme design. AIDS 2005;19(18):2141-2148. [ Links ]
25. Fairall LR, Bachmann MO, Louwagie GM, et al. Effectiveness of antiretroviral treatment in a South African program: a cohort study. Arch Intern Med 2008;168(1):86-93. [ Links ]
26. Ingle SM, May M, Uebel K, et al. Outcomes in patients waiting for antiretroviral treatment in the Free State Province, South Africa: prospective linkage study. AIDS 2010;24(17):2717-2725. [ Links ]
27. Longley N, Muzoora C, Taseera K, et al. Dose response effect of high-dose fluconazole for HIV-associated cryptococcal meningitis in southwestern Uganda. Clin Infect Dis 2008;47(12):1556-1561. [ Links ]
28. Micol R, Tajahmady A, Lortholary O, et al. Cost-effectiveness of primary prophylaxis of AIDS associated cryptococcosis in Cambodia. PLoS ONE 2010;5(11):e13856. [ Links ]
29. Harling G, Orrell C, Wood R. Healthcare utilization of patients accessing an African national treatment program. BMC Health Serv Res 2007;7:80. [ Links ]
30. Haile B, Maartens G, Wood R. Economic evaluation of cryptococcal meningitis and inpatient tuberculosis treatment for HIV-infected adults in South Africa. American Public Health Association 129th Annual Meeting, Atlanta, Georgia, 21-25 October 2001(abstract 25431). [ Links ]
31. Meya DB, Manabe YC, Castelnuovo B, et al. Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cell count < or = 100 cells/microL who start HIV therapy in resource-limited settings. Clin Infect Dis 2010;51(4):448-455. [ Links ]
32. Manosuthi W, Athichathanabadi C, Uttayamakul S, Phoorisri T, Sungkanuparph S. Plasma nevirapine levels, adverse events and efficacy of antiretroviral therapy among HIV-infected patients concurrently receiving nevirapine-based antiretroviral therapy and fluconazole. BMC Infect Dis 2007;7:14. [ Links ]
33. Wakeham K, Parkes-Ratanshi R, Watson V, Ggayi AB, Khoo S, Lalloo DG. Co-administration of fluconazole increases nevirapine concentrations in HIV-infected Ugandans. J Antimicrob Chemother 2010;65(2):316-319. [ Links ]
Joseph N Jarvis, Desmond Tutu HIV Centre, Institute of Infectious Disease and Molecular Medicine, University of Cape Town, Infectious Diseases Unit, G F Jooste Hospital, Cape Town, Centre for Infection, Department of Cellular and Molecular Medicine, St George's University of London, and Division of Infectious Diseases and HIV Medicine, Department of Medicine, UCT; Thomas S Harrison, Centre for Infection, St George's University of London; Nelesh Govender, Mycology Reference Unit, National Institute for Communicable Diseases, a Division of the National Health Laboratory Service, and Faculty of Health Sciences, University of the Witwatersrand, Johannesburg; Stephen D Lawn, Desmond Tutu HIV Centre, UCT, and Department of Clinical Research, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine; Nicky Longley, Desmond Tutu HIV Centre, UCT, and Centre for Infection, St George's University of London; Tihana Bicanic, Centre for Infection, St George's University of London; Gary Maartens, Division of Clinical Pharmacology, Department of Medicine, UCT; Francois Venter, Wits Institute for Sexual & Reproductive Health, HIV and Related Diseases and Department of Medicine, Wits; Linda-Gail Bekker and Robin Wood, Desmond Tutu HIV Centre and Division of Infectious Diseases and HIV Medicine, UCT; Graeme Meintjes, Infectious Diseases Unit, G F Jooste Hospital, Division of Infectious Diseases and HIV Medicine, UCT, and Institute of Infectious Diseases and Molecular Medicine, UCT.
Corresponding author: J N Jarvis (joejarvis@doctors.net.uk)














