Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.3 Pretoria Mar. 2011
ORIGINAL ARTICLES
Direct admission versus inter-hospital transfer to a level I trauma unit improves survival : an audit of the new Inkosi Albert Luthuli Central Hospital trauma unit
S CheddieI; D J J MuckartII; T C HardcastleIII; D Den HollanderIV; H CassimjeeV; S MoodleyVI
IMB ChB. Department of General Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
IIMB ChB, FRCS, MMSc. Department of General Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
IIIMB ChB, MMed, FCS. Department of General Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
IVMB ChB, FCS. Department of General Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
VMB ChB, DA, FCS. Department of General Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
VIMB ChB, FCS. Department of General Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
ABSTRACT
OBJECTIVE: To audit the performance of a new level I trauma unit and trauma intensive care unit.
METHODS: Data on patients admitted to the level I trauma unit and trauma intensive care unit at Inkosi Albert Luthuli Central Hospital, Durban, from March 2007 to December 2008 were retrieved from the hospital informatics system and an independent database in the trauma unit.
RESULTS: Four hundred and seven patients were admitted; 71% of admissions were inter-hospital transfers (IHT) and 29% direct from scene (DIR). The median age was 27 years (range 1 - 83), and 71% were male. Blunt injury accounted for 66.3% of admissions and penetrating trauma for 33.7%. Of the former, motor vehicle-related injury accounted for 87.4%, with 81% of paediatric admissions due to pedestrian-related injuries. The median injury severity score (ISS) for the entire cohort was 22 (survivors 18, deaths 29; p<0.001). Patients in the DIR group had a significantly higher mean ISS compared with the IHT group (DIR 25, IHT 20; p<0.02). The overall mortality rate was 26.3%. There were 37 deaths (31.1%) in the DIR group and 70 (24.3%) in the IHT group (p=0.19). In patients surviving more than 12 hours the overall mortality rate was 21.1% (DIR 13.7%, IHT 23.5%; p=0.042).
CONCLUSIONS: Trauma is a major cause of premature death in the young. Despite a significantly higher median ISS in direct admissions, there was no difference in mortality. Of those surviving more than 12 hours, patients admitted directly had a significant decrease in mortality. Dedicated trauma units improve outcome in the critically injured.
Almost two decades have passed since the establishment of a dedicated trauma centre was proposed as the only means of managing the burgeoning trauma epidemic by providing definitive care for complex injuries.1 In March 2007, the Inkosi Albert Luthuli Central Hospital (IALCH) level I trauma unit was commissioned.
The unit conforms to the requirements of the Committee on Trauma of the American College of Surgeons,2 with in-house registrars in general and orthopaedic surgery and anaesthesia. There are two theatres, one for orthopaedics and the other for general surgery, and a dedicated intensive care unit (ICU). All complementary surgical sub-specialties and necessary allied health care professionals are available in the hospital. Imaging facilities include ultrasound in the unit and an adjacent computed tomography scanner and angiography suite.
Entry and exit criteria were defined according to published recommendations.2 Admissions are derived direct from scene (DIR) in consultation with the pre-hospital care providers, or by interhospital transfer (IHT). The latter group may be accepted for surgery and subsequent ICU management if surgical expertise is unavailable at the referral source, for ICU admission following surgery at another institution, or for ICU management alone if surgery is not required.
Before this unit opened all trauma patients in the Ethekwini region were referred to four level II registrar-based facilities in Durban where trauma and non-trauma patients competed for attention, theatre and ICU facilities. The substantially lower risk of death when care is provided in a dedicated trauma centre instead of a general hospital3 comes at considerable cost. As South Africa has enormous challenges in providing health care, the expenditure on such dedicated centres must be shown to be justifiable. We aimed to describe the spectrum of major trauma managed at the IALCH level I trauma unit from 2007 to 2008, and to determine whether direct admission confers a survival advantage compared with inter-hospital transfers.
Patients and methods
All patients admitted from March 2007 to December 2008 were included. Data were retrieved from the unit database and chart review using the Medicom hospital information system. The study was approved by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal and the Provincial Health Research Committee of the Department of Health, KwaZulu-Natal.
Variables included referral source, mechanism of injury, age and sex distribution, injury severity score (ISS) and mortality. The ISS was calculated using the 1990 Abbreviated Injury Scale. We compared patients admitted DIR and IHT with respect to mechanism and severity of injury, time to reach definitive care (which was defined as ICU admission), and outcome. Outcome assessments included an overall mortality rate and the mortality rate in patients admitted to the ICU, which excluded deaths on arrival, during resuscitation, in theatre and within 12 hours of admission to the ICU where further care was deemed futile. This sub-analysis allowed a fair comparison between the DIR and IHT groups, because the excluded patients listed above would automatically be excluded from IHT.
An unpaired Student's t-test was used to compare ISS between the groups and the chi-square test to analyse differences in mortality. A value of p<0.05 was used to determine significant differences.
Results
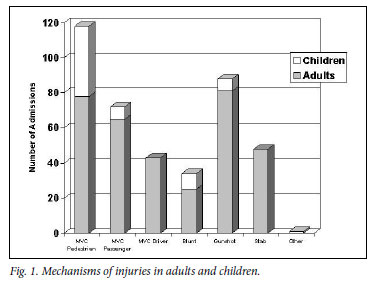
A total of 407 patients were admitted; 289 (71%) were males and 118 (29%) females. The median age was 27 years (inter-quartile range 21-35); 64 (16%) were children (age <16 years). The mechanisms of injury are shown in Fig. 1. Blunt trauma accounted for 66.3% of admissions and penetrating injury for 33.7%. Of the former, motor vehicle collisions (MVCs) were the commonest cause, being responsible for 87.4% of blunt injuries. Collisions involving pedestrians accounted for 50% of MVC-related injuries, passengers comprised 31% and drivers 19%. With the exception of passenger-related trauma, males dominated all categories of injury. MVCs accounted for 85.1% of paediatric admissions, of whom 81% were pedestrians, accounting for nearly half of all pedestrian-related trauma. Gunshots were responsible for 64.2% of penetrating injuries.
There were 119 (29%) DIR admissions and 288 (71%) IHTs (Table I). No significant differences in age and sex distribution were apparent between the groups, although there were significantly more patients with penetrating trauma in the IHT group and significantly more MVC-related injuries in the DIR group.
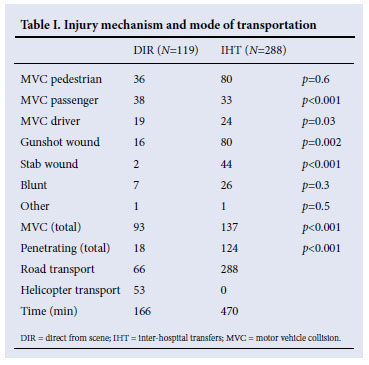
Table II shows the median ISS and inter-quartile range for all admissions, survivors and deaths. The full range of ISS was from 1 to 57 in survivors and from 4 to 75 in deaths. Patients scoring only one point had suffered acute kidney injury following sjambok beatings. No injury other than minor skin abrasions was obvious, thereby precluding any higher score. The significant difference in overall mean ISS between the DIR and IHT groups was accounted for by the significantly higher ISS in those who died. There was no significant difference between survivors in the two groups. A significant difference (p<0.01) between survivors and deaths in all groups was found.
Two hundred and eleven initial and 57 revisional operations were performed. Mechanisms of injury requiring revisional surgery were gunshot wounds following initial damage control surgery (32%), MVCs (15.8%, predominantly for orthopaedic fixation), blunt trauma (7%), and stab wounds (5.2%). The mortality rate in patients undergoing initial surgery was 26.8% and that in patients requiring revisional surgery 45.8%. Surgery for blunt trauma had the highest mortality rate (50%), followed by gunshot wounds (30.5%) and MVCs (21.8%). Fiftythree patients were referred after surgery at the initial hospital and had no further procedures, and 106 were managed non-operatively.
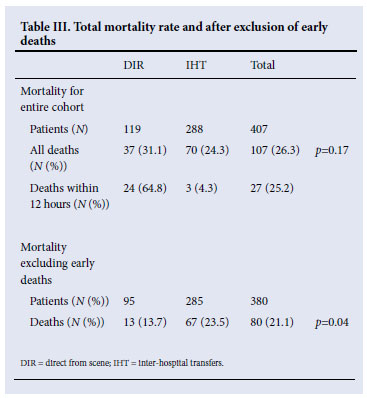
Table III illustrates the mortality rates for the entire cohort and after excluding early deaths. No significant association was found with injury mechanism and there was no significant difference in overall mortality rate between the DIR and IHT groups. Of the 107 deaths, 27 occurred within the first 12 hours of admission (15 during resuscitation, 5 in theatre, and 7 within 12 hours of ICU admission); 24 were in the DIR and 3 in the IHT group. Excluding these early deaths, the overall mortality rate for patients surviving more than 12 hours in the ICU was 21.1%. Despite there being no significant differences in mean ISS or between survivors and deaths in the DIR and IHT groups, the mortality rate was significantly lower in DIR patients, being 13.7% in the DIR group and 23.5% in the IHT group.
Discussion
Trauma is a major contributor to the burden of disease in South Africa. The National Injury Mortality Surveillance System (NIMSS) report estimated that 60 000 non-natural deaths occurred in 2004, which accounted for 12% of all deaths. The most common non-natural death in South Africa was accidental/unintentional injuries, accounting for 39.8% of fatal injuries; violence and homicide accounted for 39.3%. The pattern of fatal injuries in KwaZulu-Natal was different, violence and homicide accounting for 45.9% and accidental injuries for 33%.4 Of the latter, 84% were transport related.
Despite campaigns to reduce the incidence of motor vehiclerelated injury, little improvement has been evident. These campaigns are targeted towards safer driving, but pedestrians remain a constant problem, especially children, most of whom in this study had been knocked down by a vehicle. The Johannesburg Trauma Unit reported a significant increase in pedestrian-vehicle collisions from 1985 to 2001, which was attributed to widespread urbanisation and lack of road safety education and awareness.5 Road safety campaigns must address children from low-income environments.6 Alcohol and drug abuse are important contributors to MVCs,1 with over 30% being alcohol related.7,8 This is exceptionally problematic in adult pedestrians, where legislation is non-existent.
Mortality rates are the best reflection of the efficacy of management of severe trauma. Our results demonstrate that direct admission to a dedicated trauma unit improves survival. Despite a significantly higher mean ISS in the DIR group for the entire cohort, there was no significant increase in mortality. Excluding early deaths during resuscitation or in theatre, which are not represented in the IHT group, for equally severe injuries as graded by the ISS, survival is significantly improved by direct transfer to a level I trauma unit. This is not due to lack of expertise in the referring centres but because delay in transportation of critically ill patients to centres offering definitive care is substantially detrimental to outcome.9-12 In our urban environment the 6-hour difference between direct and inter-hospital admissions undoubtedly contributed to an increased mortality rate. This may not apply to rural trauma, where initial evaluation and stabilisation at small local hospitals is crucial before transferring patients for definitive care. Having said that, it is critical that outreach programmes are developed for these hospitals and that access to a level I centre is available from any primary care facility without referral to an intermediate-level hospital.
We found no significant difference in mortality between patients transported by ambulance versus air. Often the time taken to reach definitive care is not hastened by airborne transport, the helicopter being dispatched only after road-based emergency services have stabilised the patient and assessed the need for an air ambulance.13 Primary response and transfer by helicopter to a level I trauma centre markedly reduces mortality. We believe that the air emergency services are grossly under-utilised and are negotiating to station the helicopter at IALCH as the primary response vehicle.
The merit of dedicated trauma care is evident by a distinct survival advantage for severely injured patients transferred directly to a level I trauma centre where a dedicated trauma team with comprehensive allied services is available 24 hours a day.2 However, success comes at a price as the cost of trauma care is high. The IALCH trauma unit's annual budget (excluding salaries) is approximately R11 million, with an average cost per ICU bed per day of R5 604. In the UK the mean hospital cost per trauma patient was £7 983.14 Since trauma afflicts the economically active workforce of society, the socio-economic impact of this association is immeasurable. The most cost-effective method of reducing the cost of trauma care is to prevent trauma from happening, and spending on trauma prevention programmes would be a prudent investment.
In 1997 the ICU mortality rate in a local regional hospital without a dedicated trauma service was 28.3%,15 little different from that in the IHT group in our cohort. In contrast, this audit shows a substantial survival advantage in trauma victims admitted directly to a level I trauma unit conforming to the requirements for optimal care of the severely injured. In 1991, dedicated trauma facilities in South Africa were portrayed as a fairytale and trauma as the Cinderella of the medical profession.1 With the inception of the level I facility at IALCH that fairytale has come true.
References
1. Muckart DJJ. Trauma - the malignant epidemic. S Afr Med J 1991;79:93-95. [ Links ]
2. Committee on Trauma American College of Surgeons. Resources for Optimal Care of the Injured Patient. Chicago: American College of Surgeons, 1993. [ Links ]
3. MacKenzie EJ, Rivara FP, Jurkovich FJ, et al. A national evaluation of the effect of trauma-centre care on mortality. N Engl J Med 2006;354:366-378. [ Links ]
4. Prinsloo M, ed. A Profile of Fatal Injuries in South Africa: 7th Annual Report of the National Injury Mortality Surveillance System. Tygerberg: Medical Research Council, University of South Africa, Crime, Violence and Injury Lead Programme, 2005. http://www.sahealthinfo.org.za/violence/nimss. htm (accessed 9 September 2008). [ Links ]
5. Bowley DMG, Khavandi A, Boffard KD, et al. The malignant epidemic - changing patterns of trauma. S Afr Med J 2002;92:798-802. [ Links ]
6. Sukhai A. A profile of childhood pedestrian fatalities in South Africa in 2001. Injury & Safety Monitor 2003;2(1):2-4. http://www.mrc.ac.za/crime/aug2003.pdf (accessed 9 September 2008). [ Links ]
7. Bradshaw D, Nannan N, Laubscher R, et al. The South African Burden of Disease Study 2000: Estimates of Provincial Mortality. Cape Town: South African Medical Research Council, 2004. [ Links ]
8. Sukhai A. Sentinel Surveillance of Substance Abuse and Trauma at Addington Hospital, Durban: Final Report of the Trauma & Drug Study, 1999 to 2001. Durban: Medical Research Council, University of South Africa, Crime, Violence and Injury Lead Programme, 2003. http:/www.sahealthinfo.org/violence/addington%2099.pdf (accessed 9 September 2008). [ Links ]
9. Harrington DT, Connolly M, Biffl WL et al. Transfer times to definitive care facilities are too long: A consequence of an immature trauma system. Ann Surg 2005;241(6):961-968. [ Links ]
10. Svenson J. Trauma systems and timing of patient transfer: are we improving? Am J Emerg Med 2008;26:465-468. [ Links ]
11. Sampalis J, Denis R, Frechette P, et al. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma 1997;43(2):288-296. [ Links ]
12. Nathens AB, Maier RV, Brundage SI, et al. The effect of interfacility transfer on outcome in an urban trauma system. J Trauma 2003;55(3):444-449. [ Links ]
13. Biewener A, Aschenbrenner U, Rammelt S, et al. Impact of helicopter transport and hospital level on mortality of polytrauma patients. J Trauma 2004;56(1):94-98 [ Links ]
14. Christensen MC, Nielsen TG, Ridley S, et al. Outcomes and costs of penetrating trauma injury in England and Wales. Injury 2008;39:1013-1025. [ Links ]
15. Muckart DJJ, Bhagwanjee S, Gouws E. Validation of an outcome prediction model for critically ill trauma patients without head injury. J Trauma 1997;43:934-938. [ Links ]
Accepted 22 October 2010.
Corresponding author: D J J Muckart (davidmuc@ialch.co.za)














