Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.1 Pretoria Jan. 2011
ORIGINAL ARTICLES
Abdominal and pericardial ultrasound in suspected extrapulmonary or disseminated tuberculosis
Maya Nathu PatelI; Stephen BeningfieldII; Vanessa BurchIII
IMB ChB, FCRad (Diag) (SA), MMed (Diag Rad). Department of Radiology, G F Jooste Hospital and University of Cape Town
IIMB ChB, FFRadD (SA). Department of Radiology, Groote Schuur Hospital and University of Cape Town
IIIMB BCh, FCP (SA), PhD. Department of Medicine, G F Jooste Hospital and University of Cape Town
ABSTRACT
OBJECTIVE: Tuberculosis (TB) in patients with or without advanced HIV infection may present as smear-negative, extrapulmonary and/or disseminated forms. We studied the role of pericardial and abdominal ultrasound examinations in the determination of extrapulmonary or disseminated TB.
METHODS: A prospective descriptive and analytic cross-sectional study design was used to determine the ultrasound findings of value in patients with subsequently proven TB. Ultrasound examinations were performed on 300 patients admitted to G F Jooste Hospital with suspected extrapulmonary or disseminated TB.
OUTCOME MEASURES: The presence of hepatomegaly, splenomegaly, lymphadenopathy (location, size and appearance), ascites, pleural effusions, pericardial effusions and/or splenic micro-abscesses was noted. Clinical findings, microbiological and serological data were also recorded, correlated and analysed.
RESULTS: Complete data sets were available for 267 patients; 91.0% were HIV positive, and 70.0% had World Health Organization clinical stage 4 disease. Active TB (determined by smear or culture) was present in 170 cases (63.7%). Ultrasonically visible abdominal lymphadenopathy over 1 cm in minimum diameter correlated with active TB in 55.3% of cases (odds ratio (OR) 2.6, 95% confidence interval (CI) 1.5 - 4.6, p=0.0002). Ultrasonographically detected pericardial effusions (OR 2.8, 95% CI 1.6 - 5.0, p<0.0001), ascites (OR 2.2, 95% CI 1.2 - 4.2, p=0.005) and splenic lesions (OR 1.9, 95% CI 1.0 - 3.5, p=0.024) also predicted active TB.
CONCLUSION: Pericardial and abdominal ultrasound examinations are valuable supplementary investigations in the diagnosis of suspected extrapulmonary or disseminated TB.
Extrapulmonary tuberculosis (EPTB) is defined as tuberculosis (TB) of organs other than the lungs and usually results from lympho-haematogenous dissemination of the organism. The term disseminated TB refers to TB that involves multiple body systems, including the lungs. Target areas are usually those with high vascularity and include the lymph nodes, meninges, spleen, kidneys, spine and growing ends of bones. Additional sites of involvement include the pleura, pericardium, peritoneum, liver, gastro-intestinal tract, genito-urinary tract and skin.1,2
Co-infection with HIV has a significant impact on the TB pandemic. HIV-infected individuals more commonly present with EPTB, disseminated disease and smear-negative TB, and more readily suffer recurrence of TB after treatment. EPTB occurs in only 15.0% of non-HIV TB patients and in up to 70.0% of HIV-positive TB patients, with the risks of EPTB and mycobacteraemia increasing with advancing immunosuppression.1,3,4 TB may also accelerate the progression of HIV infection to AIDS.5
Despite therapeutic advances, TB remains a serious health burden causing 3 million deaths per year globally.6 The situation in South Africa is one of the worst; in 2004 the TB case fatality rate was 79/100 000 population, a rate of over twice the global average of 32/ 100 000.7,8
The Western Cape province in South Africa has the highest national TB rate of 810/100 000 (2003), and the frequency is increasing further.9,10 Over the past 7 years the number of TB cases has increased by 66.0% in the Cape Town metropole. In 2005 there were 25 000 active TB cases in Cape Town, and two-thirds of these patients were co-infected with HIV.11
The effective control of TB depends to a significant extent on prompt diagnosis and early initiation of appropriate therapy. The diagnostic gold standard is a positive culture of the bacterium, but it may take up to 8 weeks to obtain this. Smear microscopy can provide earlier confirmation by demonstrating acid-fast bacilli (AFB), but smear-negative cases remain problematic. In these patients treatment may be delayed while awaiting culture results, increasing the risk of disease progression, disease transmission, morbidity and mortality.12
EPTB and disseminated TB are difficult to diagnose, and invasive procedures may be needed to acquire adequate specimens for testing.13 The diagnosis of active EPTB requires the presence of at least one culture-positive specimen from an extrapulmonary site, histological evidence of AFB, or strong clinical evidence.14
We evaluated the role of pericardial and abdominal ultrasound in the diagnosis of EPTB or disseminated TB with the primary objective of prospectively determining any ultrasound findings that could be used to indicate the presence of active EPTB or disseminated TB.
Methods
Study design and study participants
A prospective descriptive and analytic cross-sectional study design was used to determine the ultrasound findings of diagnostic value in patients with subsequently proven TB. It was conducted at G F Jooste Hospital, a 200-bed acute care hospital in Cape Town and serving approximately 1.3 million of the overall Cape Town metropole population of 3.4 million people. It serves Khayelitsha and Nyanga, the sub-districts with the highest rates of HIV- and TB-related deaths.15
The study comprised 300 consecutive patients admitted to the medical wards at G F Jooste Hospital between August 2004 and October 2004 with a clinically suspected diagnosis of EPTB or disseminated TB, defined as TB in any two extrapulmonary sites such as lymph nodes, pericardium, peritoneum, nervous system, skeletal system, etc.
Investigations and outcome measures
Ultrasound scans were performed with a Toshiba Eccocee machine, using a 3.5 -5.0 MHz convex probe, as well as a 7.5 MHz linear probe where indicated. Nodes were actively sought in the para-aortic, peripancreatic, peri-portal, splenic hilar, mesenteric and inguinal regions. Nodes larger than 10 mm were considered significant and their location was documented, in addition to their appearances and the minimum and maximum nodal dimensions, measured in the short axis diameter. The liver and spleen were examined for size and any focal lesions or abscesses. The presence of ascites, pleural effusions and pericardial effusions was noted.
Microbiological samples, including sputum, urine, serous fluid, cerebrospinal fluid (CSF) and lymph node fine-needle aspirates, were sent for TB microscopy and culture, and radiography was performed at the discretion of the supervising clinician(s). The study protocol did not include routine HIV testing, but this was requested if clinically warranted. Ethics approval was obtained from the University of Cape Town's Health Sciences Research Ethics Committee (rec ref 279/2004) and the Clinical Executive of G F Jooste Hospital.
Data analysis
The ultrasound findings, clinical records, radiographic findings and laboratory investigations were collected and entered into an Access (Microsoft, Redmond, WA, USA) database. The primary cohort was stratified according to the outcome measures. The data were extracted from the database onto an Excel (Microsoft) spreadsheet and analysed using STATA (Stata Statistical Software, release 7.0; StataCorp, 2001, College Station, TX, USA). Frequency and two-by-two tables were generated. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated, and chi-square and Fisher's exact tests were used for comparing proportions. A probability value (p) of <0.05 was considered significant. Logistic regression analysis, using a model building technique, was performed to determine which of the ultrasound variables predicted TB infection.
Results
Of the patients 267 (89.0%) had adequate laboratory specimens to confirm the presence or absence of active TB; 33 patients with inadequate samples were excluded. Patient ages ranged from 15 to 86 years (mean 36.4 years, standard deviation (SD) 10.8 years); 174 patients (65.2%) were female.
HIV status was known in 221 patients (82.7%), of whom 201 (91.0%) were HIV positive. Of the HIV-positive patients, 30.0% were in World Health Organization (WHO) clinical stage 3 and 70.0% in WHO clinical stage 4. Active TB (diagnosed by smear or culture) was present in 135 HIV-positive patients and 10 HIV-negative patients; the difference was not statistically significant (OR 1.9, 95% CI 0. 7 -5.2, p=0.18).
In total, 170 of 267 patients (63.7%) were diagnosed with active TB by positive smear or culture. Culture-positive Mycobacterium tuberculosis was present in 134 patients (Table I).
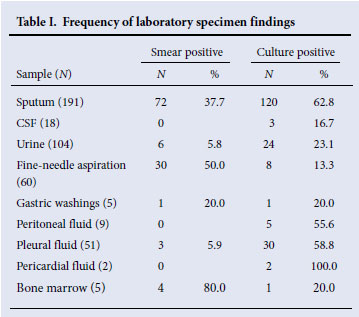
Table II displays the salient ultrasound findings. Deep abdominal lymphadenopathy correlated significantly with active TB as diagnosed by smear or culture (OR 2.6, 95% CI 1.5 -4.6, p=0.0002). In total, 55.3% of the patients with active TB (diagnosed as above) had abdominal lymphadenopathy on ultrasound. The splenic hilar, para-aortic, peri-portal and peri-pancreatic nodal locations all corresponded significantly with active TB (95% CI 1.1 -5.8, p=0.0002 - 0.021). In 23 of 125 patients (18.4%) ultrasound examination detected abdominal lymphadenopathy, but TB could not be confirmed in these cases.
The presence of an ultrasonically detectable pericardial effusion also correlated significantly with active TB (diagnosed by smear or culture) (OR 2.8, 95% CI 1.6 -5.0, p<0.0001).
Hepatomegaly and splenomegaly were present in 18.8% and 12.9% of patients, respectively, but no significant correlation was evident when comparing liver and splenic size with TB. However, the correlation between the presence of splenic lesions and active TB (diagnosed by smear or culture) was significant (OR 1.9, 95% CI 1.0 - 3.5, p=0.024).
Ascites was present in 65 cases (38.2%) and correlated significantly with active TB (diagnosed by smear or culture) (OR 2.2, 95% CI 1.2 - 4.2, p=0.005).
The combinations of abnormal ultrasound findings that correlated significantly with active TB (diagnosed by smear or culture) are set out in Table II. Logistic regression analysis determined (with a decreased deviance of 30.1 and significance at the 5% level of p=0.0000) that abdominal lymphadenopathy, ascites and pericardial effusion were the ultrasound variables with the best predictive value for active TB (diagnosed by smear or culture). The model showed that the presence of abdominal nodes was associated with a 2.6 times increased risk of active TB, ascites with a 2.2 times increased risk, and pericardial effusion with a 2.8 times increased risk. In combination, the presence of lymphadenopathy, ascites and splenic lesions was associated with a 2.9-fold increased risk of active TB.
Discussion
This study evaluating the role of abdominal and pericardial ultrasound in diagnosing patients with suspected EPTB or disseminated TB in 267 patients is the largest conducted in South Africa to date. A study published in 2002 suggested that abdominal ultrasound might be an appropriate method to diagnose TB in the setting of repeatedly negative sputum smears, but made no mention of their study sample size.16 Reviewing a total of 35 ultrasound scans in patients with HIV and abdominal pain, Hudson and Wood found that a final diagnosis of TB was made in 12 cases and concluded that the role of ultrasound in the diagnosis of TB was limited.17 Others have also concentrated on HIV and TB, but none have investigated the role of ultrasound examination in the diagnosis of smear-negative TB.12,18-20
We document a final sample of 170 patients (63.7% with suspected TB) subsequently diagnosed with active TB on the basis of smear or culture. The presence of intra-abdominal lymphadenopathy >10 mm in diameter, splenic microabscesses and ascites, alone or in combination, was associated with a 3-fold increased risk of active TB. Although abdominal lymphadenopathy is a well-described manifestation of TB, the importance of this ultrasound finding in patients with proven TB in our study highlights the value of abdominal ultrasound examination in the investigation of patients with suspected disseminated or EPTB. In the appropriate clinical context, abdominal lymphadenopathy, particularly associated with splenic lesions and/or ascites found at ultrasound examination, could be used as a surrogate marker of TB while awaiting specimen culture results.
Ultrasound is a cheap, non-invasive radiological modality. Although operator interpretation is subjective and experience necessarily develops with time, the technique of scanning is readily taught, especially in the abdomen, and ultrasound scanning can therefore be widely practised. It could be especially useful in centres where the burden of TB is high, particularly in disseminated, smear-negative TB in HIV-positive patients. The appropriate use of ultrasound can potentially avert unnecessary delays in initiating treatment and decrease the diagnostic cost by avoiding invasive tests and tertiary referral. Since the majority of patients in our local setting are seen at the primary health care level, local access to ultrasound imaging modalities is important.
Approximately 18.0% of patients (23 of 125) had abdominal lymphadenopathy that could not be confirmed to be of tuberculous origin. In these patients TB remained a probable diagnosis, but other diagnoses should be considered in such circumstances, e.g. systemic candidiasis, mycobacteria other than TB, Kaposi's sarcoma, disseminated cryptococcosis or lymphoma. Direct sampling of these nodes was not undertaken in this study.
The presence of ultrasonically detectable pericardial fluid was associated with a 2.8 times increased risk of TB and should be routinely sought when performing abdominal ultrasound examination on patients with suspected EPTB or disseminated TB. A local study on patients with pericardial effusions of 10 mm or more in size found that tuberculous pericarditis was present in 53%, 100% had an enlarged cardiothoracic ratio, and 45.5% were HIV positive.21
Hepatomegaly and splenomegaly were not consistent findings in patients with active EPTB, in contrast to other studies.22-24 However, the presence of splenic micro-abscesses correlated significantly with active TB (OR 1.9, 95% CI 1.0 -3.5, p=0.024). This finding emphasises the need for use of high-frequency ultrasound probes for early diagnosis, since the presence of splenic micro-abscesses in TB is known to be associated with increased mortality.13,25
Ascites is a common finding in abdominal TB, and smear or culture tests on ascitic fluid are useful.24,26 Our study found ascites in 38.2% of cases and was associated with a 2-fold increased risk of active TB. Generally smears are positive in less than 5% of cases.1
Conclusion
Ultrasound examination of the abdomen and pericardial space may facilitate an early clinical diagnosis of TB in smear-negative HIV-positive patients while awaiting bacteriological evidence of active TB. HIV and TB present the most serious challenges to public health across the world and need to be addressed urgently. By improving the index of suspicion of active TB, ultrasound examination may prevent unnecessary delays in initiation of therapy, limit disease transmission, curb the development of multidrug-resistant TB and reduce morbidity and mortality, particularly in smear-negative patients with EPTB or disseminated TB.
References
1. Golden MP, Vikram HR. Extrapulmonary tuberculosis: An overview. Am Fam Physician 2005;72(9):1761-1768. [ Links ]
2. Vijayan VK. Disseminated tuberculosis. J Indian Med Assoc 2000;98(3):107-109. [ Links ]
3. Hausler H. Tuberculosis and HIV/AIDS - clinical guidelines 2000. http://www.doh.gov.za/aids/docs/tuberculosis.html (accessed 29 May 2008). [ Links ]
4. Toossi Z. Virological and immunological impact of tuberculosis on human immunodeficiency virus type 1 disease. J Infect Dis 2003;188(8):1146-1155. [ Links ]
5. Harries A, Maher D, Graham S. TB/HIV - A Clinical Manual. 2nd ed. Geneva: World Health Organization, 2004. http://whqlibdoc.who.int/publications/2004/9241546344.pdf (accessed 29 May 2008). [ Links ]
6. WHO Global Partnership to Stop TB. The global plan to stop tuberculosis. 2003. http://www.who.int/tb/publications/global_plan_to_stop_tb/en/index.html (accessed 4 March 2006). [ Links ]
7. Kaiser Family Foundation. US global health policy. Country data. http://www.globalhealthreporting.org (accessed 29 May 2008). [ Links ]
8. World Health Organization. WHO global tuberculosis control. http://www.who.int/tb/publications/global_report/2005/download_centre/en/ (accessed 29 May 2008). [ Links ]
9. Millennium development indicators for South Africa, 2003. http://www.sarpn.org.za/documents/d0000875/docs/UNDP%20MDG%20Indicators%20-%202004.pdf (accessed 29 May 2008). [ Links ]
10. Western Cape Department of Health World TB Day 2006. http://www.capegateway.gov.za/Text/2006/5/tb_stats_2006.pdf (accessed 29 May 2008). [ Links ]
11. Tuberculosis. www.capetown.gov.za/clusters/health.asp?IDPathString=1123-13743258&clusid=259&catparent=3258 (accessed 24 June 2006). [ Links ]
12. Smart T. Improving the diagnosis of active TB in people with HIV. HIV and AIDS treatment in practice No. 60, 2005. http://hivinsite.ucsf.edu/InSite?page=pa-hatip-60 (accessed 29 May 2008). [ Links ]
13. Barthwal MS, Rajan KE, Deoskar RB, Sharma SK. Extrapulmonary tuberculosis in human immunodeficiency virus infection. Medical Journal Armed Forces India 2005;61(4):340-341. [ Links ]
14. Wares F, Balasubramanian R, Mohan A, Sharma SK. Extrapulmonary tuberculosis: Management and control. Tuberculosis control in India. Chapter 11. http://www.tbcindia.org/pdfs/Tuberculosis%20Control%20in%20India11.pdf (accessed 29 May 2008). [ Links ]
15. Population, age and sex distribution, Cape Town 2003. http://www.capetown.gov.za/clusters/health (accessed 24 June 2006). [ Links ]
16. Emby DJ, Hunter M. The value of ultrasound in the HIV-infected patient with a fever of undetermined origin. S Afr Med J 2002;92(8):566. [ Links ]
17. Hudson CP, Wood R. Ultrasound for the diagnosis of HIV-associated tuberculosis. S Afr Med J 2003;93(6):440-441. [ Links ]
18. Meintjies GA. Delay in the diagnosis of TB. Poster presentation at the South Africa AIDS Conference, Durban, August 2003. [ Links ]
19. Wilson D, Nachega J, Morroni C, Chaisson R, Maartens G. Diagnosing smear-negative tuberculosis using case definitions and treatment response in HIV-infected adults. Int J Tuberc Lung Dis 2006;10(1):31-38. [ Links ]
20. Hudson CP, Wood R, Maartens G. Diagnosing HIV-associated tuberculosis: reducing costs and diagnostic delay. Int J Tuberc Lung Dis 2000;4(3):240-245. [ Links ]
21. Reuter H, Burgess LJ, Doubell AF. Role of chest radiography in diagnosing patients with tuberculous pericarditis. Cardiovasc J S Afr 2005;16(2):108-111. [ Links ]
22. Ortona L, Federico G. Pulmonary and extrapulmonary tuberculosis. Rays 1998;23(1):64-77. [ Links ]
23. Raviglione MC, Narain JP, Kochi A. HIV-associated tuberculosis in developing countries: clinical features, diagnosis and treatment. Bull World Health Organ 1992;70(4):515-526. [ Links ]
24. Uzunkov A, Harma M, Harma M. Diagnosis of abdominal tuberculosis: experience from 11 cases and review of the literature. World J Gastroenterol 2004;10(24):3647-3649. [ Links ]
25. Mukadi YD, Maher D, Harries A. Tuberculosis case fatality rates in high prevalence populations in sub-Saharan Africa. AIDS 2001;15(2):143-152. [ Links ]
26. Pitchenik AE, Fertel D, Bloch AB. Mycobacterial disease: epidemiology, diagnosis, treatment, and prevention. Clin Chest Med 1988;9(3):425-441. [ Links ]
Accepted 3 May 2010.
Corresponding author: M N Patel (mpfiles@iafrica.com)














