Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 no.1 Pretoria Jan. 2011
SCIENTIFIC LETTER
Down syndrome in paediatric outpatient wards at Durban hospitals
Horacia NaidooI; Colleen AldousIII; Hemendra RamdhaniIV; William WinshipV; Nadine HenriquesVI; Emil KormuthII
IBSc (Hons). School of Biochemistry, Genetics and Microbiology, University of KwaZulu-Natal, Durban
IIPhD. School of Biochemistry, Genetics and Microbiology, University of KwaZulu-Natal, Durban
IIIPhD. Nelson R Mandela School of Medicine, University of KwaZulu-Natal
IVMB ChB, DCH (SA), FCPaed (SA), Cert (Medical Genetics) (SA). Department of Paediatrics and Child Health, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
VMB ChB, MMed (Paed). Department of Paediatrics and Child Health, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
VIMB ChB, DCH, FC Paeds. Department of Paediatrics and Child Health, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
To the Editor: The birth of a child with Down syndrome (DS) has many serious implications - physical and mental deficiencies, medical conditions and lifestyle challenges.1 The high incidence (1 in 600 births in South Africa2) and high cost of medical care highlight the need for effective health care.2 The South African Human Genetic Policy Guidelines include a rudimentary list pertaining to the management of DS.2 In the USA, the American Academy of Pediatrics (AAP) has addressed this issue by devising clinical protocols3 focusing on improving the level of functioning and quality of life of children with DS. Countries such as Thailand4 and, to a lesser extent, South Africa, in KwaZulu-Natal,2 have adopted and adapted these guidelines. The importance of the guidelines for clinical and counselling practices and their routine adherence is a daily challenge for 3 Durban hospitals with a total of 2 staff members dedicated to genetic matters.
DS studies4,5 have recognised the value of routine screening tests and genetic counselling, as they pre-empt the need for targeted therapy, early intervention programmes and support groups, which results in better quality of health and significant developmental progress.
We investigated and compared the clinical management of DS children at King Edward VIII, Prince Mshiyeni and Inkosi Albert Luthuli Central Hospitals in Durban with that occurring in countries such as Thailand, where the guidelines are implemented.4
Method
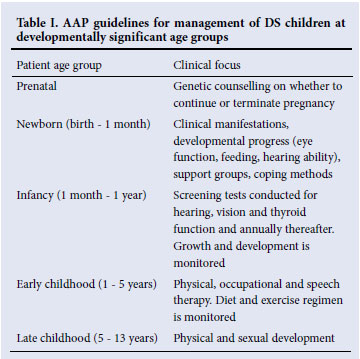
Medical chart checklists in accordance with AAP guidelines3 (Table I) were used to record information from hospital charts (Biomedical Research Ethics ref. no. BE100/08), to compare the care received by DS children and their families at Durban hospitals with the AAP recommendations and that observed in the Thai study.4 The 72 most recently treated cases of DS were assessed, and the relevant clinical staff facilitated the provision of further patient information including observation of routine patient practice in dealing with DS.
The data were captured on a Microsoft Excel spreadsheet, which allowed simple derivation of the frequencies of DS in maternal age groups, patient age groups, screening tests and counselling performed. The frequencies of screening tests conducted and genetic counselling services offered were used as a measure of efficiency of health care and compared with AAP recommendations and findings reported by a study conducted in Thailand.4
Results
Table II shows the standard of clinical care offered to paediatric DS patients in this study in terms of screening tests and genetic counselling services, and a comparison with that observed in a Thai study4 and the AAP recommendations.3 The Thai study did not have recorded data for antenatal counselling and support group referrals.
Discussion
Irregularly performed screening tests and minimal genetic counselling indicate a need for specific DS guidelines for the strict adherence and employment criteria of genetic staff.
The SA guidelines2 on the clinical management of DS offer a generalised list rather than a specific protocol. They include points addressing advanced maternal age, prenatal and postnatal diagnosis, preventive measures, rehabilitation and genetic counselling. Although relevant, there are no specific and utilisable clinical protocols on the management of DS patients in terms of the types of screening tests, preventive measures and rehabilitation. They also lack focus on the factors of age groups and development of DS patients.
Our study indicated a significant difference between AAP guidelines (Table I), the statistics from the Thai study, and the observed frequencies of tests and services offered cumulatively at the three Durban hospitals (Table II). While the Thai study adhered to the AAP recommendations, the Durban hospitals lagged in both screening tests (thyroid function, hearing and vision) and genetic counselling services (antenatal and support groups). However, screening tests for cardiac defects were performed often (84.7%) owing to their frequent occurrence and cause of morbidity and mortality in DS.6
Another concern is the large number of mothers (42.9%) of advanced maternal age and low frequency of antenatal counselling observed in the study. Advanced maternal age (a crucial factor in DS, illustrated by 80% of births being to mothers >35 years old) should be considered in a resource-poor setting such as South Africa.
Regarding genetic staff, there was during the study one full-time geneticist, one part-time geneticist, and no genetic counsellors employed across the three hospitals - a stark contrast to the recommendations made by the Human Genetics Policy of SA which prescribes a minimum of 36 genetic counsellors and 18 medical geneticists for KZN.2 The subsequent inadequate clinical care of DS patients is highlighted in this study and has prompted media attention and lawsuits for negligence.7
The provincial and national health departments bear the ultimate responsibility for implementing an agreed set of protocols that are strictly adhered to, and for employing sufficient genetic staff to ensure effective health care for DS patients and their families. Besides the financial benefit of a largely preventive health care programme, the quality of life of DS patients and their families will increase exponentially while alleviating the strain on the health care system.
We gratefully acknowledge the National Research Foundation (NRF) for funding, and the University of KwaZulu-Natal for a postgraduate scholarship.
References
1. Antonarakis SE, Lyle R, Dermitzakis ET, Reymond A, Deutsch S. Chromosome 21 and Down syndrome: From genomics to pathophysiology. Nat Rev Genet 2004;5:725-738. [ Links ]
2. National Department of Health. Human Genetics Policy Guidelines for the Management and Prevention of Genetic Disorders, Birth Defects and Disabilities. Pretoria: Department of Health, 2000. [ Links ]
3. Cunniff C, Frias JL, Kaye C, Moeschler JB, Panny SR, Trotter TL. Health supervision for children with Down syndrome. Pediatrics 2001;107(2):442-449. [ Links ]
4. Wasant P, Boonyawat B, Tritilanunt S, et al. Factors influencing development of Down syndrome children in the first three years of life: Siriraj Experience J Med Assoc Thai 2008;91(7):1030-1037. [ Links ]
5. Thornton Jones H, Hampshaw S, Solton H, Madhok R. Reviewing local screening policies - a worthwhile exercise? British Journal of Clinical Governance 2002;7(3):165-176. [ Links ]
6. Fuchs KM, Peripert JF. First trimester Down syndrome screening: Public health implications. Semin Perinatol 2005;29:267-271. [ Links ]
7. Naidu E. Our disastrous doctors. The Sunday Tribune. Durban: 2 May 2010.
Accepted 17 September 2010.
Corresponding author: H Naidoo (HoraciaN@gmail.com)














