Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.100 n.2 Pretoria Feb. 2010
SAMJ FORUM
CLINICAL IMAGES
Partial flap avulsion following refractive surgery
Roland R Berger; M D Williams; Clive A Novis
Refractive surgery, mainly laser in situ keratomileusis (LASIK), is widely used to correct refractive errors, mainly myopia. It consists of producing a corneal flap, ablating the underlying corneal stroma using laser energy, and repositioning the flap without suturing it to the underlying stroma.
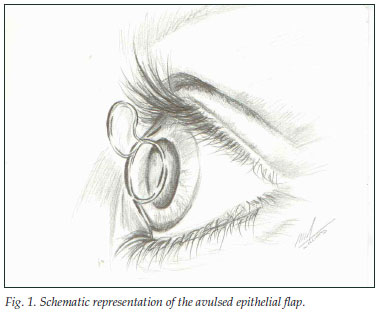
A 58-year-old man presented with blurred vision, pain and photophobia after suffering a minor injury on his right eye from a tree branch. He had had LASIK procedures 13 years ago for both eyes. The eye was congested, there was corneal fluorescein staining, and the corneal flap was partially detached and scrolled up (Fig. 1).
Under local sub-conjunctival anaesthesia the flap was irrigated, cleaned, repositioned and sutured. Methylprednisolone and gentamicin were injected subconjunctivally, and the eye was closed for 24 hours. The following day the eye was quiet with a visual acuity of 6/9 and the subsequent course was uneventful.
After a LASIK procedure the flap adheres to the corneal stroma because of the action of the endothelial pump and because the epithelium grows over the flap's margin. Scarring and fibrosis occur only at the flap's margin.1 Early and late complications are mainly haloes, glare, star-burst and dry eye. A dreaded complication is corneal ectasia.2
Traumatic dislocation has been reported after 10 days,3 1 year4 and 3 years and 5 months.5 Our report is the first to indicate the possibility of weak adhesion of the flap after a much longer time, i.e. 13 years.
References
1. Ivarsen A, Laurgern T, Moller-Petersen T. Characterisation of corneal fibrotic wound repair at the LASIK flap margin. Br J Ophthamol 2003; 87(10): 1272-1278. [ Links ]
2. Piccoli P, Gomes AAC, Piccoli FVA. Corneal ectasia detected 32 months after LASIK for correction of myopia and asymmetric astigmatism. J Catar Ref Surg 2003; 29(3): 1222-1225. [ Links ]
3. Melki SA, Talamo JH, Demetriades AM. Late traumatic dislocation of laser in situ keratomileusis corneal flaps.Ophthalmology 2000; 107(12): 2136-2139. [ Links ]
4. Tai M-C, Chen C-H, Chang C-J. Late traumatic dislocation of Lasik corneal flaps. J Med Sci 2003; 23(3): 165-166. [ Links ]
5. Tetz M, Werner L, Muller M, Dietze U. Late traumatic lasic flap loss during contact sport. J Catar Ref Surg 2007; 33(7): 1332-1335. [ Links ]
Roland R Berger, MD (Padova), Specialist in Ophthalmology (Tel-Aviv), is Senior Consultant at Tambo Memorial Hospital in Boksburg. His main interest is ophthalmic trauma; Melissa D Williams, MB BCh, is doing her community service at the same hospital; Clive A Novis, MB BCh, FCS (Ophthalmology), is in private practice. His main interests are cataract and refractive surgery.














