Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.100 n.1 Pretoria Jan. 2010
SAMJ FORUM
CLINICAL IMAGES
Myopathy with a normal creatine kinase level in juvenile myopathic dermatomyositis
Ntobeko B A Ntusi; Jeannine M Heckmann*
Dr Ntusi is a senior medical registrar and Dr Heckmann an associate professor in the Division of Neurology, Department of Medicine, Groote Schuur Hospital and University of Cape Town
A 14-year-old boy was referred to our division with a diagnosis of 'progressive myopathy with psoriasis' after a normal calf muscle biopsy excluded a previously suspected diagnosis of muscular dystrophy. The referring clinician had rejected a diagnosis of inflammatory myositis, based on repeatedly normal serum creatine kinase (CK) levels. Described as a 'lazy child' who refused to play games such as soccer, he had developed increasing weakness over 3 years, a rash and, more recently, hard painless lumps in both axillae and groins. The weakness affected proximal limbs, resulting in difficulty with standing up from a low chair, getting out of bed and walking more than 200 meters. Climbing stairs was a challenge, and he could not carry objects such as grocery bags.
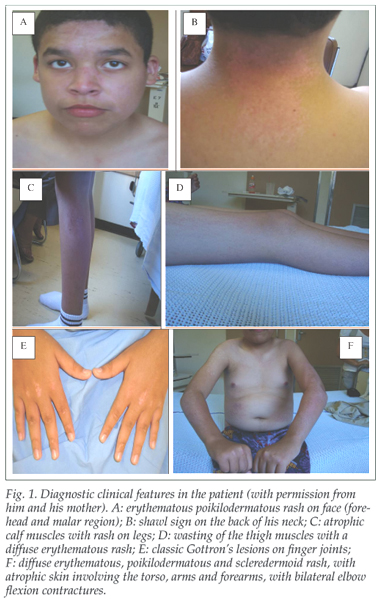
He demonstrated classic Gottron's lesions on both hands, subcutaneous calcinosis in both axillae and groins, and a shawl sign on the back of his neck, associated with a diffuse erythematous, poikilodermatous and sclerodermoid rash, with atrophic skin involving the face, arms, forearms and legs. He had bilateral elbow flexion contractures (Fig. 1). His thigh and calf muscles were atrophic, with marked proximal myopathy and inability to stand up from a chair with arms folded or to rise from a recumbent position. Nailfold capillaroscopy showed dilated, tortuous, haemorrhagic vessels with telangiectasia and drop-out. His vital capacity and other systems were normal. His serum CK was 108 (normal <140 units/litre (U/1)), and electromyography showed myopathic units (low amplitude, short duration, polyphasic) with evidence of active denervation (fibrillation potentials and positive sharp waves) consistent with an active inflammatory myositis. Dermatomyositis (DM) was diagnosed, and the patient was treated with oral prednisone, with good improvement in muscle strength and enhanced performance.
Discussion
In 1863, Wagner first recognised dermatomyositis/polymyositis. Unverricht, in 1891, first described dermatomyositis as we know it today. Idiopathic inflammatory myopathies, comprising dermatomyositis, polymyositis and inclusion body myositis,1 represent the largest group of acquired and potentially treatable causes of skeletal muscle weakness. Childhood or adolescent DM is an uncommon inflammatory disease classically encompassing hallmark cutaneous changes, proximal muscle weakness and laboratory evidence of myositis.3 The average age of onset is 7 years.2
Our case of juvenile myopathic dermatomyositis was unrecognised because of a falsely normal serum CK level and a muscle biopsy in a relatively spared muscle. The CK is the most widely used and most sensitive and specific diagnostic test, but it is not the most useful in monitoring disease activity and response to treatment.3 An elevated CK is seen in 80 - 95% of adult DM patients,3 and in only two-thirds of patients with juvenile DM.2 Although the mean CK elevation is usually tenfold, the level does not always correlate with disease activity,4 and particularly not in juvenile subjects with DM.2 Hence, other markers of muscle disease should be looked for when DM is suspected but the CK is not elevated (e.g. aldolase, aspartate transaminase, type 1 and type 5 lactate dehydrogenase isoenzymes, carbonic anhydrase III, myoglobin, troponin I, troponin T, and glutamate pyruvate transaminases).5
In the context of a myositis, a normal CK may reflect burnt-out disease,6 the presence of an inhibitor7 or co-morbid systemic lupus erythematosus and rheumatoid arthritis.4, 8 In juvenile DM the interpretation of the CK needs to be individualised. Although a normal CK with active DM often has a poorer prognosis,8 DM is a treatable and potentially reversible form of muscle weakness that, unrecognised, may have grave consequences. Our case highlights the importance of not relying solely on CK for diagnosing the condition, and that a trial of steroids should be considered in subjects with inflammatory myopathies, despite low or normal CK levels.
1. Bohan A, Peter JB. Polymyositis and dermatomyositis (parts 1 and 2). N Engl J Med 1975; 292: 344-347, 403-407. [ Links ]
2. Feldman BM, Rider LG, Reed AM, Pachman LM. Juvenile dermatomyositis and other idiopathic inflammatory myopathies of childhood. Lancet 2008; 371: 2201-2212. [ Links ]
3. Bohan A, Peter JB, Bowman RL, Pearson CM. A computer-assisted analysis of 153 patients with polymyositis and dermatomyositis. Medicine (Baltimore) 1977; 56: 255-286. [ Links ]
4. Sanmarti R, Collado A, Gratacos J, et al. Reduced activity of serum creatine kinase in rheumatoid arthriotis: a phenomenon linked to the inflammatory response. Br J Rheum 1994; 33: 231-234. [ Links ]
5. Pachman LM, Hayford JR, Chung A, et al. Juvenile dermatomyositis at diagnosis: clinical characteristics of 79 children. J Rheum 1998; 25: 1198-1204. [ Links ]
6. Targoff IN. Laboratory manifestations of polymyositis/dermatomyositis. Clin Derm 1988; 6: 76-92. [ Links ]
7. Kagen LJ, Aram S. Creatine kinase activity inhibitor in sera from patients with muscle disease. Arthr Rheum 1987; 30: 213-217. [ Links ]
8. Rider LG, Miller FW. Laboratory evaluation of the inflammatory myopathies. Clin Diag Lab Immunol 1995; 2: 1-9. [ Links ]
* Corresponding author: J Heckmann (jeanine.heckmann@uct.ac.za)














