Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.99 n.4 Pretoria Apr. 2009
SAMJ FORUM
CLINICAL IMAGES
Cutaneous bacillary angiomatosis: a marker of systemic disease in HIV
N Grilo; D Modi; P Barrow
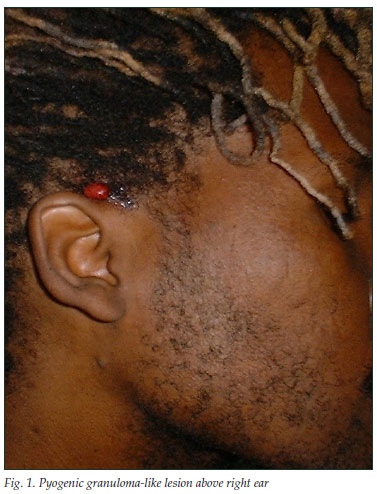
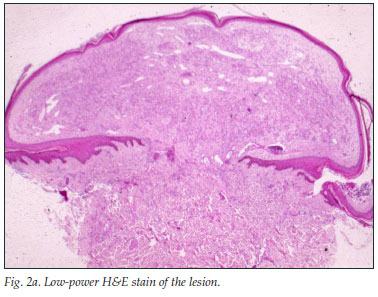
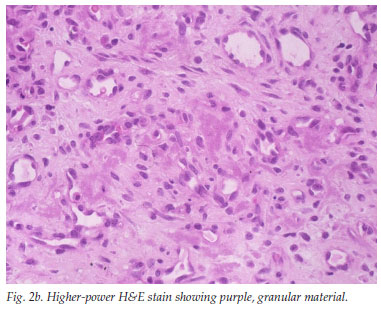
A 33-year-old man presented with a 5-week history of relapsing fever, weight loss and right upper quadrant pain. He was pyrexial, the liver and spleen were enlarged and tender, and he had a few pyogenic granuloma-like tumours on the skin (Fig. 1). He was HIV positive (CD4 cell count 119/µl), and had raised liver enzyme levels (alkaline phosphatase (ALP) 258 IU/l and gamma-glutamyl transpeptidase (GGT) 218 IU/l). Results of hepatitis studies and the alpha-fetoprotein level were normal, blood cultures were negative and a chest radiograph was normal. An abdominal ultrasound scan showed an enlarged and markedly echogenic liver and spleen with multiple hypo-echoic foci in keeping with possible microabscesses. The skin and liver showed similar histological features: clusters of purple, granular material that stained positive for organisms, confirmed on the Warthin-Starry stain (Figs 2a, 2b and 2c).
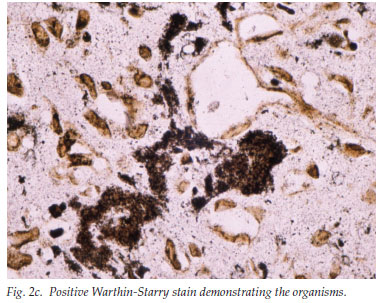
The polymerase chain reaction (PCR) confirmed the presence of Bartonella spp. on both biopsy specimens. The skin lesions had almost completely disappeared after 1 month on erythromycin 500 mg 4 times a day, but the patient was subsequently lost to follow-up.
Discussion
Bacillary angiomatosis (BA) is caused by the Gram-negative bacteria B. henselae and B. quintana. Cutaneous BA was first described in 1983, and the first case in South Africa (where disease prevalence in the host, the domestic cat, is 24%1) was reported in 1993.2 BA is difficult to diagnose, requiring culture for at least 21 days; serological studies are often unreliable, and special staining with the Warthin-Starry stain is used to confirm the tissue diagnosis. The prevalence of Bartonella bacteraemia (nested PCR) was 10% at the Johannesburg HIV outpatient clinics.3 The treatment of choice is erythromycin 500 mg 4 times a day for 3 months; also useful are doxycycline, ceftriaxone and the fluoroquinolones.
Examination of the skin is mandatory because cutaneous lesions may be a marker of systemic BA infection, especially in HIV-positive patients, and skin biopsy is much safer than liver biopsy for tissue diagnosis.
1. Kelly PJ, Matthewman LA, Hayter D, et al. Bartonella (Rochalimaea) henselae in southern Africa - evidence for infections in domestic cats and implications for veterinarians. J S Afr Vet Assoc 1996; 67: 182-187. [ Links ]
2. Levy GR, Nayler S. Bacillary angiomatosis. The first case reported in South Africa. S Afr Med J 1993; 83: 855-856. [ Links ]
3. Frean J, Arndt S, Spence D. High rate of Bartonella henselae infection in HIV-positive outpatients in Johannesburg, South Africa. Trans R Soc Trop Med Hyg 2002; 96: 549-550. [ Links ]
Dr Nella Grilo qualified and did her postgraduate training at the University of the Witwatersrand. She is currently a consultant dermatologist at Chris Hani Baragwanath Hospital, Johannesburg. Professor Deepak Modi also trained at Wits, and is currently academic head of the Division of Dermatology there. Dr Peter Barrow is a gastroenterologist, currently working in Dubai.
Corresponding author: N Grilo (27823189392@vodamail.co.za)














