Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.99 n.2 Pretoria Feb. 2009
ORIGINAL ARTICLES
Complications of tube thoracostomy for chest trauma
David MaritzI; Lee WallisII; Timothy HardcastleIII
IMB ChB. Division of Emergency Medicine, University of Cape Town and Stellenbosch University, Tygerberg, W Cape
IIMB ChB, MD, FCEM. Division of Emergency Medicine, University of Cape Town and Stellenbosch University, Tygerberg, W Cape
IIIMB ChB, MMed, FCS (SA) (current affiliation: Trauma Service, Inkosi Albert Luthuli Central Hospital, Durban). Head of Trauma, Tygerberg Hospital and Stellenbosch University, Tygerberg, W Cape
ABSTRACT
OBJECTIVES: To determine the insertional and positional complications encountered by the placement of intercostal chest drains (ICDs) for trauma and whether further training is warranted in operators inserting intercostal chest drains outside level 1 trauma unit settings.
METHODS: Over a period of 3 months, all patients with or without an ICD in situ in the front room trauma bay of Tygerberg Hospital were included in the study. Patients admitted directly via the trauma resuscitation unit were excluded. No long-term infective complications were included. A self-reporting system recorded complications, and additional data were obtained by searching the department's records and monthly statistics.
RESULTS: A total of 3 989 patients with trauma injuries were seen in the front room trauma bay during the study period; 273 (6.8%) patients with an ICD in situ or requiring an ICD were assessed in the trauma unit and admitted to the chest drain ward; 24 patients were identified with 26 complications relating to the insertion and positioning of the ICD; 22 (92%) of these had been referred with an ICD in situ. An overall complication rate of 9.5% was seen. Insertional complications numbered 7 (27%), with 19 (73%) positional complications. The most common errors were insertion at the incorrect anatomical site, and extrathoracic and too shallow placement (side portal of the drain lying outside the chest cavity).
CONCLUSION: Operators at the referral hospitals have received insufficient training in the technique for insertion of ICDs for chest trauma and would benefit from more structured instruction and closer supervision of ICD insertion.
Intercostal chest drains (ICDs) are commonly used in South African emergency centres (ECs), with wide insertion variations among health care practitioners.1,2 Anecdotal evidence suggests that complications relating to the insertion and management of ICDs are frequent. No South African data exist on the morbidity and mortality of ICD insertion. ICD insertion for trauma purposes is an essential skill for doctors working in emergency settings. Incorrect insertion and placement can lead to significant morbidity and even mortality. An audit in the UK revealed that 45% of junior doctors would have placed an ICD outside the safe triangle described by the British Thoracic Society.3 Clear guidelines exist for the correct method of ICD insertion.4
Tygerberg Hospital (TBH) in the Cape Town metropole (and affiliated to Stellenbosch University Medical School) has a level 1 trauma unit which comprises a front room trauma bay and a resuscitation unit for intensive care management of severe trauma. The front room assesses over 15 000 patients annually, while the resuscitation unit receives over 900 patients per year. ICDs inserted in patients with chest trauma at lower levels of care are referred to the TBH front room trauma unit for further management and inpatient care. The unit is staffed by experienced advanced trauma life support (ATLS) operators under the auspices of the Trauma Section of the Division of Surgery. The unit employs an open technique with blunt dissection of the muscles and pleura (without trocar) for inserting ICDs.
Because of increasing concerns over complications relating to ICD insertion at referring institutions, we undertook a 3-month audit at the trauma unit of all patients arriving with, or requiring, an ICD for chest trauma.
Aims
We aimed to determine the complications and errors commonly encountered during the placement of ICDs for trauma and to establish whether further training is warranted for operators inserting ICDs outside level 1 trauma unit settings.
Methods
The audit ran for the 3-month period 1 January to 31 March 2008. We included all patients with chest trauma referred to the TBH trauma unit with an ICD in situ, and patients with chest trauma in whom an ICD had been placed by TBH trauma unit staff. Patients admitted directly to the resuscitation unit were not included.
A self-reporting logbook was kept in the trauma unit; staff were asked to record any complications relating to the insertion or positioning of ICDs which they encountered while on duty. Daily reminders to the trauma staff encouraged this practice. Other data were obtained from the department's admission records and monthly statistics.
Only complications relating to the insertion and position of ICDs were recorded. Late infective complications were not examined. The American College of Surgeons ATLS guidelines for tube thoracostomy were used as the accepted standard of practice.4 We classified complications as insertional (relating to the technique of insertion) or positional (in the wrong place).
Results
A total of 3 989 patients with trauma injuries (Table I) were seen in the front room of the trauma unit over the 3-month period; 273 (6.8%) arrived with an ICD in situ or required an ICD in the trauma unit. All were admitted to the chest drain ward.

Within the group of 273 patients, we identified 24 with a total of 26 complications or errors relating to the insertion or position of the ICD. No deaths resulting from insertion of an ICD were recorded. Of the patients with complications, 22 (92%) arrived at the trauma unit with an ICD in situ. Seven (27%) of the complications were insertion-related (Table II).

In the patients with an ICD in situ, 4 ICDs were placed elsewhere than the chest, 10 were not inserted deeply enough (last side portal situated outside the chest cavity) and 5 were in the incorrect anatomical site. Three of the latter 5 drains were placed outside the safe triangle recommended by the British Thoracic Society5 (a triangle marked by the anterior border of the latissimus dorsi, lateral border of the pectoralis major and a line horizontal to the nipple) (Fig. 1); the other 2 drains had been inserted into the original stab wound.
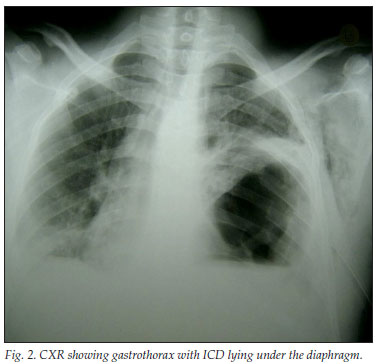
Three ICDs were incorrectly sutured. One fell out of the chest during transport. In another patient, the ICD had been attempted on the wrong side (without a confirmatory chest Xray (CXR)) at the referral hospital, but this was halted after the skin incision when the patient pointed this out. Subsequently, the patient arrived without an ICD, and review of the CXR revealed no indication for ICD placement. In another case, the ICD was inserted below the left diaphragm, the acute gastrothorax following blunt chest trauma having being misdiagnosed as a tension pneumothorax (Table III) (Figs 2 and 3).

The ICD was not placed under water in one of the patients requiring an ICD within the trauma unit. This was discovered during a ward round and might have been a nursing error that occurred while changing the bottle. The other case was an extrathoracic placement of the ICD in a polytrauma patient.
Discussion
The insertion of an ICD for chest trauma is a common procedure in South African ECs. No data exist on South African morbidity and mortality relating to ICD insertion and management. Despite the existence of established international guidelines, there is wide variation in the level of experience and training among operators as well as a lack of standardised guidelines and supervision. No data are available on how many doctors in these referral hospitals are ATLS-certified. Knowledge of the basic principles of the ICD appears to be poor.
All doctors working in emergency settings in South Africa will at some stage need to insert an ICD, which requires thorough understanding of the anatomy and physiology of the pleural space and correct teaching of the insertion technique. With correct training and supervision, it is a simple procedure to perform and should have low morbidity and mortality.6,7 Improving the current inadequate situation is eminently feasible.
Complications with ICDs have traditionally been classified as insertional, positional or infective8,9 (Table IV).
Complication rates vary from 7.6% to 30%, depending on the definition of the complications.8-13 Category-specific complications in the literature also vary widely, some reporting no insertional complications and others an insertional complication rate of 7.9%.8,12,13 Positional complication rates vary from 5.2% to 16%.8,12,13 Our results are similar to these figures. However, the definition of complications varies widely in the literature. If only severe complications with serious morbidity are used, the complication rates in the literature would fall significantly.8
The most common errors that we encountered were insertion at the incorrect anatomical site, extrathoracic placement, and placement that was too shallow (side portal of the ICD lying outside the chest cavity). Many practitioners may not classify these as complications, and the long-term morbidity (if any) related to them is not known. However, incorrect placement places heavy strain on an already overstretched health care system. Many ICDs need to be re-sited or adjusted, which wastes manpower and resources and is uncomfortable and traumatic for the patient.
Most complications (92%) recorded in this audit involved ICDs placed by doctors outside the specialised trauma unit, which suggests that operators at the referral hospitals received insufficient training in the technique. Many doctors working in these hospitals are employed as locums and may not be in fulltime clinical practice in the emergency setting. Supervision and guidance for newly qualified interns and community service medical officers is also lacking.
Risk factors for the development of complications after ICD insertion have been identified.10-12 Consistently identified as an independent risk factor for the development of complications was the insertion of an ICD by a non-surgical operator. Other factors were insertion outside of the trauma unit,12 intubated ventilated patients, the presence of shock and admission to an ICU.10,11 One study showed that an ICD procedure prior to transfer to a trauma unit had an overall complication rate of 38%.10 The key issue was that the level of training, experience and technical skill was related to the likelihood of complications. The differences in the complication rate among patients with an ICD placed outside the trauma unit in this audit suggest that these operators would benefit from more structured instruction and closer supervision of chest drain insertion.
By careful application of the recommended technique as described in the ATLS course,4 many complications or errors can be avoided. Prior to insertion, the operator must ensure that the awake patient has adequate analgesia and sedation and that the drain is inserted in the correct side. The insertion site should not be placed lower than the fourth intercostal space, as the diaphragm can rise as high as the fifth intercostal space on expiration. With the correct insertion site, the chance of inserting the chest tube into the liver or spleen is minimised. The operator must ensure that the last portal hole of the chest tube is inside the chest cavity. By using the open technique (an incision on the skin that will admit 2 fingers, and blunt dissection of the muscles and pleura without use of a trocar), a finger sweep of the chest cavity will avoid penetration of any herniated abdominal organs or penetration of lung adherent to the chest wall. The operator must advance the tube superiorly (apically) and posteriorly, and ensure that it is not kinked and that the last portal hole on the tube is not in subcutaneous tissue before suturing. This requires insertion of around 12 - 15 cm of the tube into the chest. The ICD must be securely attached to the chest wall and the drainage system correctly assembled. A CXR must confirm correct placement, that the tube is not kinked and that drainage of the haemothorax/pneumothorax has been successful.14
Training of doctors who work regularly in emergency settings needs to be addressed; this could include an outreach programme to improve the skills of doctors working in resource-poor settings. We are planning to produce a poster detailing the key steps of ICD insertion which, if prominently displayed in the EC, can serve as a reminder of the technique and reduce the complication rate.
Ethical approval. This study was approved by the Committee for Human Research, Division of Research Development and Support, Faculty of Health Sciences, Stellenbosch University.
References
1. Andrews E. A new specifically designed forceps for chest drain insertion. Injury 2003; 34(12): 957-959. [ Links ]
2. Tang A, Hooper T, Hasan R. A regional survey of chest drains: evidence-based practice? Postgrad Med J 1999; 75: 471-474. [ Links ]
3. Griffiths JR, Roberts N. Do junior doctors know where to insert chest drains safely? Postgrad Med J 2005; 81: 456-458. [ Links ]
4. Committee on Trauma. American College of Surgeons, Advanced Trauma Life Support. Chicago: American College of Surgeons, 1997. [ Links ]
5. Laws D, Neville E, Duffy J. BTS guidelines for the insertion of a chest drain. Thorax 2003; 58 (suppl II): ii53-ii59. [ Links ]
6. Hyde J, Sykes T, Graham T. Reducing morbidity from chest drains. BMJ 1997; 314: 914. [ Links ]
7. American College of Surgeons Committee on Trauma. Thoracic trauma. In: Advanced Trauma Life Support Program for Physicians: Instructor Manual. Chicago: American College of Surgeons, 1993. [ Links ]
8. Bailey RC. Complications of tube thoracostomy in trauma. J Accid Emerg Med 2000; 17: 111-114. [ Links ]
9. Collop NA, Kim SK, Sahn SA. Analysis of tube thoracostomy performed by pulmonologists at a teaching hospital. Chest 1997; 112: 709-713. [ Links ]
10. Etoch SW, Bar-Natan MF, Miller FB, Richardson JD. Tube thoracostomy. Factors related to complications. Arch Surg 1995; 130(5): 521-525. [ Links ]
11. Deneuville M. Morbidity of percutaneous tube thoracostomy in trauma patients. Eur J Cardiothoracic Surg 2002; 22(5): 673-678. [ Links ]
12. Ball CG, Lord J, Laupland KB, et al. Chest tube complications: How well are we training our residents? Can J Surg 2007; 50(6): 450-457. [ Links ]
13. Heng K, Bystrzycki A, Fitzgerald M, et al. Complications of intercostal catheter insertion using EMST techniques for chest trauma. Aust N Z J Surg 2004; 74: 420-423. [ Links ]
14. McGillicuddy D, Rosen P. Diagnostic dilemmas and current controversies in blunt chest trauma. Emerg Med Clin N Am 2007; 25: 695-711. [ Links ]
Accepted 14 November 2008.
Corresponding author: D Maritz (david.maritz.emed@gmail.com)














