Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.99 no.2 Pretoria feb. 2009
ORIGINAL ARTICLES
Colorectal cancer in South Africa: a heritable cause suspected in many young black patients
L CronjéI; A C PatersonII; P J BeckerIII
IPhD. Division of Anatomical Pathology, School of Pathology and H E Griffin Cancer Research Group, University of the Witwatersrand, and National Health Laboratory Service, Johannesburg
IIMB BCh, FCPath, PhD. Division of Anatomical Pathology, School of Pathology and H E Griffin Cancer Research Group, University of the Witwatersrand, and National Health Laboratory Service, Johannesburg
IIIPhD. Biostatistics Unit, Medical Research Council of South Africa, Pretoria
ABSTRACT
BACKGROUND: Colorectal carcinoma (CRC) has a low incidence among the black African population. Largely unrecognised in the scientific literature is the fact that a disproportionately large number of young black patients (<50 years old) present with CRC.
OBJECTIVES: To analyse those tumours, which we propose may link them to morphological features associated with known genetic pathways.
METHODS: A retrospective review of South African patients histologically diagnosed as having CRC by the Division of Anatomical Pathology, National Health Laboratory Service (NHLS) and the University of the Witwatersrand (1 732 patients from 1990 to 2003). The histology was fully reviewed in 609 patients (1997 - 2002), and all specimens from patients <50 years of age were subjected to immunohistochemistry tests for mismatch repair proteins, as well as APC and p53 proteins.
RESULTS: Most young patients (<50 years) were black (41% v. 10% white; p<0.001). Blacks had predominantly proximal tumours and significantly more poorly differentiated and/or mucinous tumours (p=0.006), and loss of mismatch repair protein expression was more evident than in whites.
CONCLUSIONS: It seems likely that CRC in young blacks develops through the accumulation of mutations, most probably via mismatch repair deficiency or promoter methylation, which in turn is linked to poor differentiation and a mucinous architecture.
Colorectal carcinoma (CRC) is uncommon in developing countries, typically in Africa and Asia.1 It is generally a disease of older people, and is associated with a Western-style diet and a sedentary lifestyle. However, the age at which patients present with CRC may be a marker for the involvement of hereditary factors which often have specific pathological features.
Over the past decade, the overall incidence of CRC in South Africa has increased markedly. In 1989, CRC was the 10th most common cancer diagnosed in males and females in South Africa but was more recently ranked among the foremost 5 cancers (5th among males and 3rd among females).2 The epidemiology of CRC in white South Africans appears to follow the classic Western trend, although the molecular pathology has not been comprehensively investigated. CRC among black South Africans is far less common, but there is evidence that numbers have been increasing in some centres.3 Furthermore, disproportionately large numbers of young black patients seem to be presenting with CRC,4 a trend which appears to be common among countries throughout the African continent.
Classically, CRC is associated with chromosomal instability and mutations of multiple tumour suppressor genes and oncogenes, including APC, K-ras and p53. Alternatively, the tumour may develop through microsatellite instability (MSI), which may be sporadic (10% of cases) or hereditary, as evident in hereditary non-polyposis colorectal cancer (HNPCC) (in 90% of cases).5 MSI is associated with mutations in the DNA mismatch repair genes hMLH1 and hMSH2, and less frequently hMSH6 and PMS2, leading to the rapid development of neoplasms through the accumulation of mutations.6 Both of these pathways follow the adenomacarcinoma sequence.
Recently, an alternative 'serrated adenoma' pathway was proposed, involving the formation of a tumour from hyperplastic polyps and adenomas through intermediate serrated adenomas.7 These tumours show a low level of MSI (MSI-L) together with a methylation phenotype characterised by the methylation of CpG islands within the promoter regions of genes such as hMLH18 and O-6-methylguanine DNA-methyltransferase (MGMT).9 Serrated neoplasia is less common and could possibly explain the occurrence of CRC among some young patients. This is frequently referred to as the 'methylator pathway'.
This study evaluates the occurrence and morphological features of CRC in South African patients over a 13-year period. Many younger patients (<50 years) were black South Africans and presented with proximal tumours that were often poorly differentiated or mucinous and with significant risk of loss of hMSH2 protein expression. These are features associated with a heritable cause of colon cancer and would aid in its early diagnosis and improved prognosis.
Methods
Patients/tumour specimens
The data were retrospective, comprising all biopsy and resection specimens that fulfilled the histological criteria for adenocarcinoma of the colon or rectum from 1990 to 2003 from the records of the Division of Anatomical Pathology, NHLS and the University of the Witwatersrand, which comprised cases seen at academic and public sector hospitals in the Gauteng, Mpumalanga and North-West provinces of South Africa. All cases were stratified by age (<50 years of age or >50 years of age at diagnosis), gender, ethnicity and tumour location (identified from histology reports). The study was approved by the Ethics Committee of the University of the Witwatersrand (clearance number 9/11/88).
From 1990 to 2003, 1 732 black and white South African patients (961 and 771 respectively) with colorectal cancer were identified. Because the study was retrospective, family histories were not obtainable. The reports of all cases were examined, and formal pathological review of cases was limited to 609 cases reported between 1998 and 2002. The original histological details were reviewed in consultation with a single pathologist (ACP), without knowledge of patient demographics and tumour sites. Each site was recorded as distal (descending colon, sigmoid, rectum) or proximal (caecum, ascending colon, transverse colon to the splenic flexure). Tumours were graded as well, moderately (low grade) or poorly differentiated (high grade) according to accepted morphological features.1 Mucinous and signet-ring tumours were considered to be of high grade.1 A subset of more recently diagnosed cases (1998 - 2002) identified in patients <50 years, regardless of race, and an equivalent number of patients >50 years, were then subjected to immunohistochemical analysis.
Immunohistochemistry
Table I summarises the antibody specifications. Immunohistochemical staining was performed on formalinfixed, paraffin-embedded tissue sections by means of routine techniques using a DakoCytomation Autostainer (DakoCytomation, Denmark). Briefly, heat-induced antigen retrieval was performed using a combination of microwaving and pressure cooking, endogenous peroxidase was blocked in 3% H2O2 in dH2O for 15 minutes, and nonspecific antigen activity was blocked by immersion of sections in 5% normal goat sera. Sections were then exposed to the monoclonal antibodies in a humidified atmosphere, rinsed and treated with a peroxidase-conjugated polymer, and secondary antibody directed against rabbit and mouse immunoglobulin (ChemMate Dako EnVision Detection kit, DakoCytomation, Denmark). Slides were again washed and incubated with 3,3'-diaminobenzidine (DAB) chromogen, washed with H2O2 and counterstained with haematoxylin, dehydrated and mounted. Appropriate positive and negative controls were used for each run. Slides were considered unsuitable for analysis when there was complete absence of signal in both mucosa and tissue lymphocytes. In some cases, there was insufficient tissue for full immunohistochemical analysis.

Statistical analysis
Statistical comparisons between groups were completed using the two-sided Fisher's exact test. Patients were analysed on the basis of ethnicity (black v. white), age (<50 years v. >50 years), gender (male v. female) and tumour site. Multinomial logistical regression analysis was performed to calculate odds ratios. All statistical analyses were compiled by Stata Intercooled 7.0 (Stata, College Station, Tex. USA). At p<0.05 the differences were considered statistically significant.
Results
Patient demographics
A total of 1 732 patients (961 blacks and 771 whites) with histologically diagnosed CRC were identified; 73% (1 259/ 1 731) were >50 years of age and 27% (472/1 731) were <50 years (age range 14 - 100 years, mean 59). Distinct differences were noted between black and white cohorts. Black patients diagnosed with CRC were predominantly male (55%), while 53% of white patients were female (p=0.001). Similarly, 83% of black patients were <50 years of age compared with only 10% of younger whites (p<0.001). Tumour location showed no correlation with race (p=1.000; 95% confidence interval (CI)).
Pathological characteristics
All young patients (<50 years, N=69) presented predominantly with low-grade tumours (65%; 109/169), with 19% (32/169) being poorly differentiated; of these, 9% (16/169) were mucinous (p<0.001). In contrast, 82% (372/452) of tumours in older patients (>50 years, N=452) were of low grade, while 10% (44/452) were poorly differentiated and, of these, 4% were mucinous (18/452) (p<0.001). Young patients also presented more commonly with high-grade tumours showing a signet ring cell morphology (11%; 14/125) compared with older patients (3%; 12/382) (p<0.001).
When compared with white patients, 15% of black patients (N=367) had poorly differentiated tumours (p=0.001), of which 7% (27/367) were exclusively mucinous. In contrast, whites (N=245) showed fewer poorly differentiated (8%; 21/245) and purely mucinous tumours (3%; 7/245) (p=0.001).
Immunohistochemistry
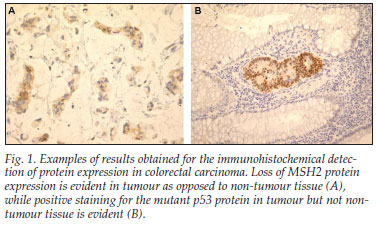
Black patients more frequently showed loss of expression of the mismatch repair gene proteins hMLH1 (23%; 29/128) (p=0.121), hMSH2 (12%; 16/129) (p=0.013) and hMSH6 (43%; 54/126) (p=0.210) (Table II) (Fig. 1, A). In contrast, white patients more frequently showed loss of APC protein expression (15%; 9/62) (p=0.648) and the accumulation of mutant p53 protein within cancer cells (58%; 37/64) (p=0.047) (Fig. 1, B). Loss of MGMT protein expression was observed in similar percentages in both ethnic groups, i.e. 27% blacks (33/123) and 26% whites (16/62) (p=1.000).
In summary, there was a significant risk (odds ratio (OR) 1.9) for young black male patients to present with poorly differentiated tumours with a degree of mucin expression, as calculated through multinomial regression analysis. In addition, young black patients have a further additional risk of developing a tumour with an exclusively mucinous appearance and with a loss of hMSH2 protein expression (OR 6.5) while they were less likely to show accumulation of mutant p53 protein in cancer cells (OR 0.6).
Discussion
We investigated the pathological features of CRC among patients presenting to academic and public sector hospitals in South Africa's most densely populated regions. Among the 961 black patients, 41% were aged <50 years, compared with the equivalent of only 10% among white patients. Of black patients, 29% were <40 years and 11.6% <30 years old, supporting studies that have identified disproportionate numbers of young South African black patients presenting with CRC.3,4
An increased incidence of colon cancer among young black patients has also been identified outside Africa. A higher proportion of African-American and Hispanic patients between 20 and 40 years of age has been reported, compared with older patients (60 - 80 years) of the same ethnicity.10 The tumours in the younger patients were poorly differentiated and/or mucinous, which is similar to the finding of our study.
An association between MSI-H CRC genotype and phenotype in African-American patients has been identified.11 These microsatellite-unstable tumours showed distinct clinical and pathological features including proximal location, highgrade and/or mucinous histology, the presence of tumourinfiltrating lymphocytes and mismatch repair gene deficiency, most frequently in the hMLH1 and hMSH2 genes.12 Young black males in our series presented with a similar morphology as well as a risk of absent hMLH1 protein expression and an increased possibility of loss of hMSH2 protein expression.
Hereditary non-polyposis colorectal cancer (HNPCC) shows similar features, including presentation at average age <50 years.13 However, diagnosis of HNPCC relies on fulfilling the Amsterdam and Bethesda criteria, and this was unavailable in our series. The strict Amsterdam criteria may lead to underdiagnosis of HNPCC, and it is suggested in the 1997 Bethesda guidelines that CRC diagnosed at a young age, even without a family history, may indeed have a genetic element leading to cancer development and that such patients should be tested for HNPCC.14 Early screening for HNPCC15 failed to identify new HNPCC cases and concurred with the revised Bethesda guidelines16 that excluded microsatellite instability testing in all adenomas from patients <40 years of age. However, Velayos and co-workers commented on the possibility of using direct germline testing as an alternative, as this shows increased sensitivity.15 As such, confirming the CRC cases in our young patients as being HNPCC by germline detection of microsatellite instability may be appropriate.
Microsatellite-unstable tumours also occur within 10 - 15% of sporadic CRCs.17 The difference in the development of sporadic versus hereditary CRC is thought to invoke the 'methylator pathway'. Promoter regions are rich in CpG islands, such as those of the hMLH1 and O-6-methylguanine DNAmethyltransferase (MGMT) genes, and hence susceptible to hypermethylation, resulting in their transcriptional silencing.8,9 Microsatellite instability in sporadic CRC has been shown to be due to methylation of the hMLH1 gene18 and is common in proximal tumours.19 After identifying MSI-H in the colon cancers from African-American patients, Ashktorab et al. noted that the MSI-H tumours are likely to be attributable to promoter methylation as 85% (29/34) of them showed hMLH1 promoter methylation.20 Although not statistically significant, compared with older whites, young black patients showed a trend towards an increased risk for absent hMLH1 protein expression. Further studies into the methylation status of this promoter region would provide insight into the CpG island methylator phenotype of these tumours.
Methylation of the MGMT gene is characteristic of CRC with low-level microsatellite instability.21 This has become associated with the 'serrated adenoma pathway'22 that involves the formation of carcinoma from hyperplastic polyps and adenomas through intermediate serrated adenomas. Cancers associated with this pathway have been shown to secrete abundant mucin.23 We report 26% (49/185) of cases showing loss of expression of MGMT, which could imply hypermethylation of this promoter region. Only 3 serrated adenomas were identified, in the later years of our study and in older female white patients. Our low percentage of serrated adenomas may indicate a low detection rate rather than a low incidence, and calls for careful identification of the entity.
Tumours of the serrated adenoma pathway are often found in the sigmoid colon and rectum24 and, through the associated p53 gene mutation, may indicate the involvement of APC gene mutations. Black South African patients were less likely than whites to show an accumulation of mutant p53 in cancer cells in our series. p53 mutations are associated with the well-known adenoma-carcinoma sequence of events that is initiated by mutations in the APC gene. However, proximal tumours developed in a p53-independent manner which may indicate a preference towards the mutator phenotype with the accumulation of mutations owing to mismatch repair deficiency. Our white patients presented more frequently with both loss of expression of the APC protein and accumulation of p53 in cancer cells; it therefore appears that their tumours develop through the suppressor pathway involving mutations of tumour-suppressor genes that are thought to be diet- and/or environmentally related.
Our subjective impression, and that of other units,25 is that the incidence of CRC is increasing, which may be validated by further updates of the Cancer Registry of South Africa.2
Young black patients were more likely to be male, with poorly differentiated and/or mucinous proximal tumours and with loss of hMSH2 protein expression. Therefore, it seems likely that CRC in these patients develops predominantly through a heritable cause linked to a deficiency in mismatch repair caused by promoter methylation. Further analysis of microsatellite instability and methylation status would aid in the additional characterisation of the pathway involved in the development of CRC in young black patients.
The authors thank the Medical Research Council of South Africa and the H E Griffin Trust for funding, and Professor Michèle Ramsay for her comments on the manuscript.
References
1. Hamilton SR, Vogelstein B, Kudo S, Riboli E, Nakamura S, Hainout P. Tumours of the colon and rectum. In: Hamilton SR, Aaltonen LA, eds. Pathology and Genetics of Tumours of the Digestive System. Lyon: IARC Press, 2000: 103-129. [ Links ]
2. Mqoqi N, Kellet P, Sitas F, Jula M. Cancer in South Africa, 1998 - 1999. Johannesburg: National Cancer Registry of South Africa, National Health Laboratory Service, 2004. [ Links ]
3. Angelo N, Dreyer L. Colorectal carcinoma - a new threat to black patients? A retrospective analysis of colorectal carcinoma received by the Institute for Pathology, University of Pretoria. S Afr Med J 2001; 91: 689-693. [ Links ]
4. Oettlé AG. Primary neoplasms of the alimentary canal in whites and Bantu of the Transvaal, 1949-1953. A histological series. Nat Cancer Inst Monogr 1967; 25: 97-109. [ Links ]
5. Liang JT, Huang KC, Cheng AL, Jeng YM, Wu MS, Wang SM. Clinicopathological and molecular biological features of colorectal cancer in patients less than 40 years of age. Br J Surg 2003; 90: 205-214. [ Links ]
6. Lynch HT, de la Chapelle A. Hereditary colorectal cancer. N Engl J Med 2003; 348: 919-932. [ Links ]
7. Freeman HJ. Heterogeneity of colorectal adenomas, the serrated adenoma, and implications for screening and surveillance. World J Gastroenterol 2008; 14: 3461-3463. [ Links ]
8. Park S-J, Rashid A, Lee J-H, Kim SG, Hamilton SR, Wu T-T. Frequent CpG island methylation in serrated adenomas of the colorectum. Am J Pathol 2003; 162(3): 815-822. [ Links ]
9. Jass JR. Serrated adenoma of the colorectum and the DNA-methylator phenotype. Nat Cli n Pract Oncol 2005; 2: 398-405. [ Links ]
10. O'Connell JB, Maggard MA, Liu JH, Etzioni DA, Livingston EH, Ko CY. The rates of colon and rectal cancers are significantly increasing in young adults. Am Surg 2003; 69: 866-872. [ Links ]
11. Ashktorab H, Smoot DT, Farzanmehr H, et al. Clinicopathological features and microsatellite instability (MSI) in colorectal cancers from African Americans. Int J Can 2005; 116: 914-919. [ Links ]
12. Jass JR, Do K-A, Simms LA, et al. Morphology of sporadic colorectal cancer with DNA replication errors. Gut 1998; 42: 673-679. [ Links ]
13. Rowley PT. Inherited susceptibility to colorectal cancer. Annu Rev Med 2005; 56: 539-554. [ Links ]
14. Rodriquez-Bigas M, Boland CR, Hamilton SR, et al. A National Cancer Institute Workshop on Hereditary Nonpolyposis Colorectal Cancer Syndrome: Meeting highlights and Bethesda guidelines. J Natl Cancer Inst 1997; 89: 1758-1762. [ Links ]
15. Velayos FS, Allen BA, Conrad PG, et al. Low rate of microsatellite instability in young patients with adenomas: Reassessing the Bethesda guidelines. Am J Gastroenterol 2005; 100: 1143-1149. [ Links ]
16. Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 2004; 96: 261-268. [ Links ]
17. Young J, Simms LA, Biden KG, et al. Features of colorectal cancers with high-level microsatellite instability occurring in familial and sporadic settings. Parallel pathways of tumorigenesis. Am J Pathol 2001; 159: 2107-2116. [ Links ]
18. Derks S, Postma C, Carvalho B, et al. Integrated analysis of chromosomal, microsatellite and epigenetic instability in colorectal cancer identifies specific associations between promoter methylation of pivotal tumor suppressor and DNA repair genes and specific chromosomal alterations. Carcinogenesis 2008; 29: 434-439. [ Links ]
19. Miyakura Y, Sugano K, Konishi F, et al. Extensive methylation of hMLH1 promoter region predominates in proximal colon cancer with microsatellite instability. Gastroenterology 2001; 121: 1300-1309. [ Links ]
20. Ashktorab H, Smoot DT, Farzanmehr H, et al. Clinicopathological features and microsatellite instability (MSI) in colorectal cancers from African-Americans. Int J Cancer 2005; 116: 914-919. [ Links ]
21. Whitehall VL, Walsh MD, Young J, Legget BA, Jass JR. Methylation of O-6-methylguanine DNA methyltransferase characterizes a subset of colorectal cancer with low-level microsatellite instability. Cancer Res 2001; 61: 827-830. [ Links ]
22. Jass JR, Whitehall VL, Young J, Leggett BA. Emerging concepts in colorectal neoplasia. Gastroenterology 2002; 123: 862-876. [ Links ]
23. Mäkinen MJ, George SMC, Jernvall P, Mäkelä J, Vihko P, Karttunen TJ. Colorectal carcinoma associated with serrated adenoma - prevalence, histological features, and prognosis. J Pathol 2001; 193: 286-294. [ Links ]
24. Paluszkiewicz P, Berbec H, Pawlowska-Wakowicz B, Cybulski M, Paszkowska A. p53 protein accumulation in colorectal cancer tissue has prognostic value only in left-sided colon tumours. Cancer Detect Prev 2004; 28: 252-259. [ Links ]
25. Degiannis E, Sliwa K, Levy R, Hale MJ, Saadia R. Clinicopathological trends in colorectal carcinoma in a Black South African population. Trop Gastroenterol 1995; 16: 55-61. [ Links ]
Accepted 27 October 2008.
Corresponding author: L Cronjé (leandracronje@webmail.co.za)














