Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 n.12 Pretoria Dec. 2008
SAMJ FORUM
CLINICAL PRACTICE
Penetrating the acoustic shadows: Emergency ultrasound in South African emergency departments
S R BruijnsI; D EngelbrechtII; W LubingaIII; M WellsIV; L A WallisV
IConsultant and an honorary lecturer at the Division of Emergency Medicine at Stellenbosch University and the University of Cape Town
IIHead of the Division of Emergency Medicine, University of Pretoria
IIIHead of the Division of Emergency Medicine, University of Limpopo
IVWorks in the Division of Emergency Medicine, University of the Witwatersrand
VHead of the Division of Emergency Medicine at Stellenbosch University and the University of Cape Town
With an increasing evidence base, emergency ultrasound (EMUS) is soon to be introduced into South African emergency departments. As with any diagnostic apparatus, there are areas where its use is particularly helpful and areas where it is not. Successful EMUS depends on binary (yes/no) decisions in life-or-death emergency medicine situations (e.g. trauma, abdominal aortic aneurysm (AAA) and cardiac arrest). As its introduction will change established treatment options, discussions have arisen about safety, alternatives and who should perform it; given the large number of generalists employed in the emergency medicine sector, the practitioners are unlikely to be radiologists. We evaluate the evidence from sites where the practice of EMUS by non-radiologists is considered to be established.
Background
EMUS provoked consternation and confrontation in every country where it was introduced, including several European countries, Japan, Israel, the UK and USA, and Australasia. Despite initial resistance, the provision of EMUS is currently accepted as a standard of care in all these places.1-5
EMUS was initiated about 20 years ago in Germany, spreading to North America in the 1990s.6,7 The original indication was to detect haemoperitoneum in the emergency department (ED), thereby offering a non-invasive alternative to diagnostic peritoneal lavage (DPL) and also expediting time-critical surgical management for trauma patients.8-11 Known in the UK, Australasia and the USA by the mnemonic FAST (focused assessment by sonography for trauma), and in Europe as PREP (polytrauma rapid echo-evaluation programme), trauma ultrasound (US) has strong evidence supporting its use and is recommended by the Advanced Trauma Life Support (ATLS) course which is widely taught in South Africa.8-22
EMUS encompasses far more than trauma US. The emergency medicine colleges of several countries also promote a policy on the use of US for early pregnancy, detection of AAA, emergency echocardiography, biliary and renal US.1-3
What is EMUS?
EMUS practised by emergency physicians differs from the US practice of other specialties. It provides information through rapid, non-invasive definition of critical anatomical structures. Performed at the bedside, it forms part of the clinical examination comparable with bedside tests such as the ECG. Its aim is to answer a goal-directed question with a binary (yes or no) answer, rather than a spectrum of queries. It does not replace computed tomography (CT) imaging, magnetic resonance imaging (MRI) or formal US, as it is not as sensitive or specific. It does, however, provide time-critical and clinically important information at the point of care - without interrupting the resuscitation - that can only be matched by including radiology expertise in the trauma team. Given the vast incidence of major trauma in South Africa, the unavailability of after-hours radiology at most public sector emergency departments and the distance between facilities, radiology-led US is unlikely to become the norm. Emergency physicians appropriately trained in the use of EMUS would then provide the best practice.
Goal-directed questions
1. Is free fluid present in the peritoneum or pericardium or pleural space?
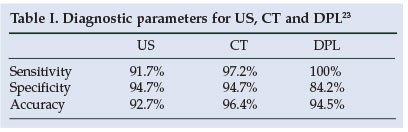
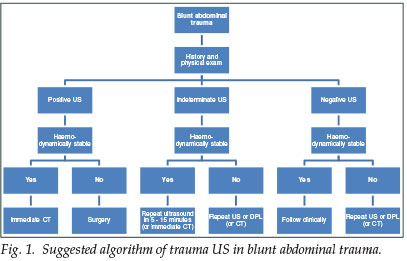
Used in blunt or penetrating torso trauma to detect free peritoneal fluid, the four-view approach is used, namely: hepato-renal space (Morrison's pouch), perisplenic area, retro-vesical/uterine space (Douglas' pouch) and subcostal pericardial view. Table I gives the diagnostic parameters of EMUS along with those for CT and DPL.23 We suggest an algorithm for trauma US to assess patients with blunt abdominal trauma adapted from the Canadian model (Fig. 1).23 The US diagnosis of pericardial fluid (with or without tamponade) provides a quick, non-invasive alternative to the nonspecific Beck's triad and also aids with the pericardiocentesis.24
2. Is a pneumothorax present?
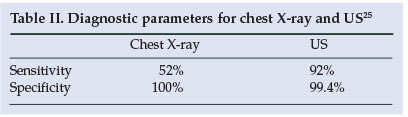
EMUS can include pleural visualisation for the assessment of a pneumothorax. Table II shows the sensitivity and specificity of chest X-ray and chest US compared with CT - the gold standard.25
3. Is an intrauterine pregnancy present?
Indications include a positive β-HCG in either a first trimester pregnant patient with abdominal pain, bleeding, near syncope and shock (suspected ectopic pregnancy or miscarriage)26-28 or a second trimester pregnant patient with abdominal pain, bleeding, near syncope and shock (suspected miscarriage).29 The sensitivity is further increased when free peritoneal fluid is detected in suspected ectopic pregnancy.30
4. Is cardiac activity present?
Demonstrating pulseless electrical activity (PEA) with low flow, as opposed to PEA with no flow, assists in deciding on further resuscitation treatment (or its futility). The former has a better prognosis than the latter (comparable with that of asystole).31-33 This application has been extended to include a search for the commonest causes of PEA:34
• massive pulmonary embolism (engorged right chambers with a flattened left ventricle and close ventricular walls or kissing trabecular muscles)
• hypovolaemia (underfilled right ventricle, hyperkinetic left ventricular wall motion, close ventricular walls and a flat inferior vena cava (IVC)
• tension pneumothorax
• pericardial tamponade.
5. Is an abdominal aortic aneurysm (AAA) present?
Detection of AAA in an unstable patient would confirm a decision to proceed to surgery in patients presenting with an abdominal mass or pain, flank pain or back pain associated with hypotension, shock, syncope or near syncope.35-37 As with early pregnancy US, sensitivity is improved through detection of free peritoneal fluid.
Other indications including biliary and renal US were added to EMUS in the USA and Australasia to reduce the time spent in the ED awaiting special investigations.1,2 Procedural US also has a role in reducing procedure-related complications and waiting times, including cannulation of arterial and central venous sites, foreign body localisation, bladder sizing/ aspiration, abscess localisation/aspiration, thoracocentesis and paracentesis, and US-guided nerve blocks.1,2
Who can practise EMUS?
EMUS is included in the emergency medicine and surgical curricula of countries where it has become standard practice and where it has also been available to practising physicians. Training methods and structure are largely similar1-5 and basically comprise 4 stages:
• introductory course
• pre-credentialing practice (usually through collecting a predefined number of supervised USs in each area)
• credentialing (continued assessment and/or practical exam)
• continuing medical education (CME).
Why the controversy?
Firstly, trauma US does not determine a specific intra-abdominal injury. While this is true, trauma US (like DPL) screens for free peritoneal fluid, thereby expediting referral for surgical intervention in an unstable patient (Fig. 1). CT is second to surgery in determining a specific injury, but the time required for travelling, setting up, performing, interpreting and communicating a result is not ideal for an unstable situation.23
Secondly, a CT scan is a better imaging modality than trauma US as it can reveal a specific injury. However, except for teaching hospitals, CT facilities are in short supply in the South African public sector. EMUS, then, is an alternative to DPL (which is associated with a high rate of negative laparotomies).38
Thirdly, radiologists are better than non-radiologists at AAA assessment and trauma US. While this is true, there is no significant difference in interpretation when the aim is to give a yes/no answer to the goal-directed question of whether free fluid or AAA is present.35,39 Competent AAA assessment can be successfully achieved by non-radiologists for screening purposes (oral communication, 24 July 2008, P Dubbins, Department of Radiology, Derriford Hospital, UK).
The future
Introductory courses were held in 2007 at the Emergency Medicine Society of South Africa's (EMSSA) conference on emergency medicine in the developing world; further courses were held in 2008, and more are planned. The EMSSA and the South African College of Emergency Medicine are working towards a policy on EMUS including the adoption of accepted international practice, which supports the development of emergency medicine as a specialty in a resource-poor country.
No technology can be claimed as the sole property of a specialty. Cardiologists perform cardiac echos, gynaecologists perform antenatal US, and the same principle applies to EMUS. Bruce Campana, from the Department of Emergency Medicine, King Faisal Specialist Hospital & Research Centre, Saudi Arabia, put it best: 'I can't use a stethoscope as well as a cardiologist, nor read plain films as well as a radiologist, nor interpret electrocardiograms as well as a cardiologist; yet somehow we emergency docs are able to make life-and-death decisions every day using these modalities. How about if we just get good enough with ultrasound to use it for emergency applications, like everything else we do?'23
We invite readers' comments on this topic.
1. American College of Emergency Physicians. Policy Statement: Emergency Ultrasound Guidelines. Irving: ACEP, 2001. http://www.acep.org (accessed 2 May 2008). [ Links ]
2. Australasian College for Emergency Medicine. Policy Document - Use of Bedside Ultrasound by Emergency Physicians. West Melbourne: ACEM, 1999. http://www.medeserv.com.au/acem/open/documents/home.htm (accessed 2 May 2008). [ Links ]
3. College of Emergency Medicine Ultrasound Sub-committee. Emergency Medicine Ultrasound Level 1 Training. London: CEM, 2006. www.collemergencymed.ac.uk/CEM/default.asp (accessed 2 May 2008). [ Links ]
4. American Institute of Ultrasound in Medicine. AIUM Practice Guideline for the Performance of the Focused Assessment With Sonography for Trauma (FAST) Examination. Laurel: AIUM, 2007. http://www.aium.org (accessed 2 May 2008). [ Links ]
5. Royal College of Radiologists. Ultrasound Training Recommendations for Medical and Surgical Specialties. London: RCR, 2005. http://www.rcr.ac.uk (accessed 2 May 2008). [ Links ]
6. Brenchley J, Sloan P, Thompson P. Echoes of things to come. Ultrasound in the UK emergency medicine practice. J Accid Emerg Med 2000; 17: 170-175. [ Links ]
7. Nordenholz KE, Rubin MA, Gularte GG, et al. Ultrasound in the evaluation and management of blunt abdominal trauma. Ann Emerg Med 1997; 29: 357-366. [ Links ]
8. Fernandez L, McKenney MG, McKenney KL, et al. Ultrasound in blunt abdominal trauma. J Trauma 1998; 45: 841-848. [ Links ]
9. Jehle D, Guarino J, Karamanoukian H. Emergency department ultrasound in the evaluation of blunt abdominal trauma. Am J Emerg Med 1993; 11: 342-346. [ Links ]
10. Rozycki GS, Ochsner MG, Jaffin JH, et al. Prospective evaluation of surgeons' use of ultrasound in the evaluation of trauma patients. J Trauma 1993; 34: 516-527. [ Links ]
11. Ma OJ, Mateer JR, Ogata M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma 1995; 38: 879-885. [ Links ]
12. McGahan JP, Cronan MS, Richards JR, et al. Comparison of ultrasound utilization and technical costs before and after establishment of 24-hour in-house coverage for ultrasound examinations. Emerg Radiol 2000; 16: 788-791. [ Links ]
13. Melanson SW, Heller M. The emerging role of bedside ultrasonography in trauma care. Emerg Med Clin North Am 1998; 16: 165-189. [ Links ]
14. Scalea TM, Rodriguez A, Chiu WC, et al. Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma 1999; 46: 466-472. [ Links ]
15. Ma OJ, Kefer MP, Mateer JR, et al. Evaluation of hemoperitoneum using a single- versus multiple-view ultrasonographic examination. Acad Emerg Med 1995; 2: 581-586. [ Links ]
16. Abrams BA, Takuma K, Seifert R, et al. Ultrasound for the detection of intraperitoneal fluid: the role of Trendelenburg positioning. Am J Emerg Med 1999; 17: 117-120. [ Links ]
17. Mandavia DP, Mallon WK. Using bedside ultrasonography to evaluate trauma patients. J Crit Illness 2000; 15: 387-394. [ Links ]
18. Committee on Trauma. Advanced Trauma Life Support Provider's Manual. 7th ed. Chicago: American College of Surgeons, 2005. [ Links ]
19. Rose J. Ultrasonography and Outcomes Research: One Small Step for Mankind or Another Drop in the Bucket? Ann Emerg Med 2006; 48: 237-239. [ Links ]
20. Brooks AJ, Price V, Simms M. FAST on operational military deployment. Emerg Med J 2005; 22: 263-265. [ Links ]
21. Vance S. The FAST scan: Are we improving care of the trauma patient? Ann Emerg Med 2007; 49: 364-366. [ Links ]
22. Melniker LA, Leibner E, Mckenney MG, et al. Randomized Controlled Clinical Trial of Point-of-Care, Limited Ultrasonography for Trauma in the Emergency Department: The First Sonography Outcomes Assessment Program Trial. Ann Emerg Med 2006; 48: 227-235. [ Links ]
23. Ross J. Emergency department ultrasound for the assessment of abdominal trauma: an overview. CJEM 1(2): 117-119. [ Links ]
24. Plummer D, Brunnette D, Asinger R, et al. Emergency department echocardiography improves outcome in penetrating cardiac injury. Ann Emerg Med 1992; 21: 709-712. [ Links ]
25. Soldati G, Testa A, Sher S, et al. Occult traumatic pneumothorax: Diagnostic accuracy of lung ultrasonography in the emergency department. Chest 2008; 133: 204-211. [ Links ]
26. Shih CHY. Effect of emergency physician-performed pelvic sonography on length of stay in the emergency department. Ann Emerg Med 1997; 29: 348-352. [ Links ]
27. Mateer JR, Aiman EJ, Brown MH, et al. Ultrasonographic examination by emergency physicians of patients at risk for ectopic pregnancy. Acad Emerg Med 1995; 2: 867-873. [ Links ]
28. Durham B, Lane B, Burbridge L, et al. Pelvic ultrasound performed by emergency physicians for the detection of ectopic pregnancy in complicated first-trimester pregnancies. Ann Emerg Med 1997; 29: 338-347. [ Links ]
29. Ma OJ, Mateer JR, DeBehnke DJ. Use of ultrasonography for the evaluation of pregnant trauma patients. J Trauma 1996; 40: 665-668. [ Links ]
30. Rodgerson JD, Heegaard WG, Plummer D, et al. Emergency department right upper quadrant ultrasound is associated with a reduced time to diagnosis and treatment of ruptured ectopic pregnancies. Acad Emerg Med 2001; 8: 331-336. [ Links ]
31. Salen P, O'Connor R, Sierzenski P, et al. Can cardiac sonography and capnography be used independently and in combination to predict resuscitation outcomes? Acad Emerg Med 2001; 8: 610-615. [ Links ]
32. Blaivas M, Fox J. Outcome in cardiac arrest patients found to have cardiac standstill on the bedside emergency department echocardiogram. Acad Emerg Med 2001; 8: 616-621. [ Links ]
33. Breitkreutz R, Walcher F, Seeger, FH. Focused echocardiographic evaluation in resuscitation management: Concept of an advanced life support-conformed algorithm. Crit Care Med 2007; 35(Supp 5): S150-61. [ Links ]
34. Bocka JJ, Overton DT, Hauser A. Electromechanical dissociation in human beings: an echocardiography evaluation. Ann Emerg Med 1988; 17: 450-452. [ Links ]
35. Shuman WP, Hastrup W, Kohler TR, et al. Suspected leaking abdominal aortic aneurysm: use of sonography in the emergency room. Radiology 1988; 168: 117-119. [ Links ]
36. Knaut AL, Kendall JL, Patten R, et al. Ultrasonographic measurement of aortic diameter by emergency physicians approximates results obtained by computed tomography. J Emerg Med 2005; 28: 119-126. [ Links ]
37. Kuhn M, Bonnin RL, Davey MJ, et al. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med 2000; 36: 219-223. [ Links ]
38. Henneman PL, Marx JA, Moore EE, et al. Diagnostic peritoneal lavage: accuracy in predicting necessary laparotomy following blunt and penetrating trauma. J Trauma 1990; 30(11): 1345-1355. [ Links ]
39. Brooks A, Davies B, Smethhurst M, et al. Prospective evaluation of non- radiologist performed emergency abdominal ultrasound for haemoperitoneum. Emerg Med J 2004; 21: 580-581. [ Links ]
 Correspondence:
Correspondence:
S R Bruijns
(scbruijns@googlemail.com
Accepted 30 September 2008.














