Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.11 Pretoria Nov. 2008
ORIGINAL ARTICLES
Do knees survive the Comrades Marathon?
Glen J HagemannI; Arie M RijkeII; Peter D CorrIII
IMB ChB, DA, MMed. Department of Radiology, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, and Monitored Healthrisk Managers, Durban
IIMD, PhD. Department of Radiology, Nelson R Mandela School of Medicine, University of Kwa-Zulu-Natal, Durban, and University of Virginia, Charlottesville, Virginia, USA
IIIMD, FFRad (D) SA. Department of Radiology, Faculty of Medicine and Health Sciences, UAE University, Al Ain, UAE
ABSTRACT
OBJECTIVE: To detect by magnetic resonance imaging (MRI) the presence and type of knee injuries in non-professional runners after running an ultra-marathon, and to determine whether ultra-marathon running exacerbates pre-existing knee injuries or results in new permanent injuries.
DESIGN: A prospective MRI study of one knee of 10 randomly selected participants who completed the Comrades Marathon between 1997 and 2002. Their knees were scanned 48 hours before the race, and 48 hours and 1 month after the race.
SETTING: All scans were performed at the Radiology Department, Wentworth Hospital, Durban, and the University of KwaZulu-Natal.
MAIN OUTCOME MEASURES: Scores of all knee injuries detected on MRI scans immediately before the race, compared with the scores after the race.
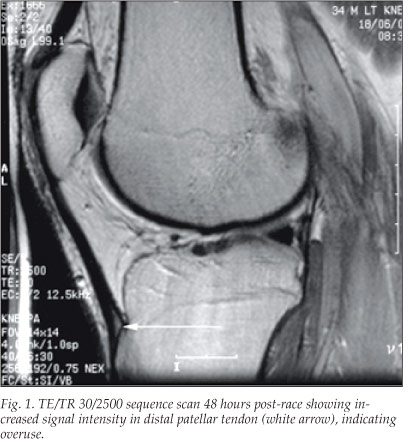
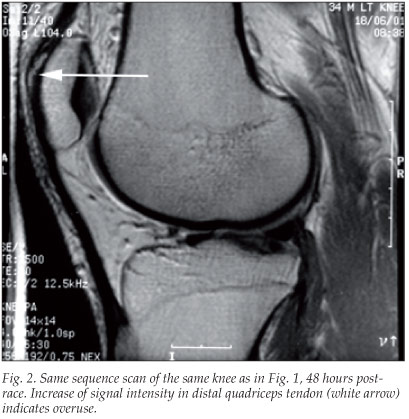
RESULTS: All scanned knees demonstrated an abnormal amount of joint fluid before the race; this increased immediately after the race in 5 runners and remained unchanged in another 5. At 1 month, 5 knees showed decreased joint fluid and 5 remained unchanged, but these were not the same runners as in the post-race groups. There was increased signal intensity in the distal patellar and quadriceps tendons in 4 runners before the race, which increased or remained the same on post-race scans in 6 knees. There was a decrease in signal intensity on scans taken 1 month later in 3 runners, with complete resolution in 2 and no change in 1. Old injuries to ligaments, tendons or other knee structures were unaffected by the race. No bone bruising, cartilage defects or meniscal abnormalities were observed. There was no significant difference in the pre- and post-race or 1-month scan scores.
CONCLUSIONS: The race appears to have had a detrimental effect on runners who started the ultra-marathon with tendinopathy, which worsened post-race by MRI criteria. One month after the race, the scan appearance of the overuse injury had either improved or resolved completely. Bone bruising or meniscal damage did not appear to occur, and the presence of increased joint fluid probably relates to stress or injury.
Knee pain in runners is commonly secondary to overuse, resulting in tendon injuries, bursitis or muscle strain. Runners are most prone to these types of injury, which may often be associated with repetitive drills or a change in the intensity or duration of a workout schedule.1 In marathon and ultramarathon runners, muscle oedema without tears can often be demonstrated in the adductor muscle, quadriceps and hamstring groups. Although the injury can occur anywhere within the muscle, its origin or insertion is most likely to be affected. This tendinopathy and periostitis in the adductors cause the so-called 'pulled groin'. In pulled hamstrings, these are usually found at the site of the ischial tuberosity, and in the quadriceps at the patellar tendon insertion on the anterior tibia.2
Marathon runners, like other athletes participating in extreme sports, are most likely to suffer overuse injury specific to their sport.3 However, other injuries such as ligament tears, cartilage injuries or fractures mostly occur secondarily to accidents such as a fall or collision.4 To what extent such secondary trauma is aggravated by marathon running is not always evident or predictable, but is of prime concern to the treating sports physician and physiotherapist.
Previous studies on the effect of long-distance running on the structures of the knee have used serial magnetic resonance (MR) images to follow the appearance and resolution of joint effusions, abnormal signal intensity in the menisci, and marrow changes with conflicting interpretations. Joint effusions and increased signal intensity in the menisci were found on scans taken within a 10-minute period after a 30-minute jog,5 but another study showed no alteration in joint fluid and meniscal signal in trained runners 24 hours before and after the completion of a long-distance race (28 - 80 km).6 Mosher et al. reported changes in knee cartilage 10 minutes after a 30-minute jog in non-athletic males,7 while Scheuller-Weidekamm et al. confirmed, using MRI, that running marathon races does not cause severe acute lesions of cartilage, ligaments or bone marrow in non-professional marathon runners.8
The Comrades Marathon (run annually on 16 June) is over a distance of 90 km between Pietermaritzburg and Durban.
There are no available documented records of the presence of old injuries in Comrades runners, and no accessible records of the follow-up of injuries sustained during the race. We aimed to determine the effect of ultra-marathon running on the structures of the normal knee and any pre-existing abnormalities of the knee using MRI. Our hypothesis was that the race aggravates the overuse injuries specific to marathon running but does not affect the MRI appearance of pre-existing or healed knee injuries.
Methods
We prospectively performed MRI studies on the knees of 10 runners who completed the Comrades Marathon between 1997 and 2002. They volunteered to have one knee scanned 48 hours before, and 48 hours and 4 - 6 weeks after, the Marathon. The scanned knee was randomly selected. Runners with previous operations or documented injuries were excluded. No runners had a known history of injury to the knee to be scanned. The age of the runners averaged 37.3 years (range 32 - 44). Three runners were women. They provided informed consent in compliance with the regulations of the Ethics Board of the University of KwaZulu-Natal, who approved this study.
MRI scans were performed on a 1.5 T whole-body scanner (GE Signa, GE Medical Systems, Milwaukee, Wisconsin) with a dedicated phased array knee coil. Knees were examined in a standard position with 20 degrees of external rotation. Examinations took 30 minutes per patient. Fast spin echo (FSE) T1 and T2 weighted sequences of the knee in the sagittal and coronal planes were performed using fat saturation (TE/TR 30/250 and 90/2 500 msec, field of view 14x14 cm, slice thickness 4.0 mm and gap 1.0 mm, and pixel size 0.75 mm2).
The MRI studies were presented in a random order to, and read independently by, two experienced musculoskeletal radiologists (AMR, PDC), who were blinded to the subjects' information, and their inter-observer agreement was measured. Information recorded from each scan was: the presence of injury of the anterior and posterior cruciate ligaments, the menisci, medial and lateral collateral ligaments, patellar and quadriceps tendons, the presence of joint fluid, and the presence of bone marrow bruising (contusion) and cartilage injury. We scored lesions in the menisci and cartilage on a 5-point scale, while the presence of focal injuries to ligaments was scored on a 3-point scale, as used by Scheuller-Weidekamm et al.8 Meniscal lesions were scored 0 - 4. A grade 1 meniscal lesion was considered to be punctate focal hyperintensity not contiguous with an articular surface; grade 2 was defined as a linear intra-meniscal hyperintensity with articular surface extension; grade 3 was a tear that reached one articular surface; and grade 4 was defined as a complex meniscal tear involving the upper or lower articular surface.8 Cartilage lesions were score from 0 to 4. A grade 1 lesion was defined as a focal hyperintense matrix signal with an intact surface; grade 2 as an ulcer or fissure <50% of the cartilage depth; and a grade 3 lesion involved >50% of the depth of the articular cartilage.
Ligaments and tendons were considered to be intact if the ligament or tendon were detected as a homogeneous low-intensity structure from its origin to its insertion (grade 0). A partial tear was considered to be have focal increased intrasubstance signal with preserved ligament orientation and outline (grade 1) while a complete tear was defined as discontinuity or non-visualisation of the ligament (grade 2). The volume of synovial effusion was scored using a 3-point scale: grade 0 was considered to be a normal joint; grade 1 was fluid collections of <10 mm depth in the retropatellar bursa measured transversely in the midline sagittal T2-weighted image; and grade 2 was fluid collection measuring >10 mm transversely.
Scores were summated for each study and compared to determine if there was a significant difference between studies using ANOVA test from a standard statistical software programme (SPSS version 15 Chicago, IL). A p-value <0.05 was considered significant. Inter-observer variability was measured using Pearson's correlation test with excellent agreement defined as k>0.8, good agreement as k=0.61 - 0.8, and poor agreement as k<0.2.
Results
There were no significant changes in the meniscal lesions between the pre- and post-scan images. Four runners had pre-existing grade 1 meniscal lesions, involving the posterior horn of the medial meniscus in 2 runners and the posterior horn of the lateral meniscus in the other 2. There were no grade 2 - 4 lesions. None had evidence of a symptomatic meniscal lesion. No hyaline cartilage or focal bone marrow bruises were detected on either the pre- or post-scans.
Five runners had positive grade 1 injuries of the patella tendon on their pre-race scans. Following the race, another 2 runners developed grade 1 injuries (Fig. 1); in one of them, the lesions were not visible on the 1-month follow-up scan. Two runners had partial tears in the quadriceps tendon (grade 1) with no new lesions detected following the race (Fig. 2). One runner had a grade 1 partial tear of the anterior cruciate ligament detected before the race. No additional ligament lesions were detected after the race. One runner each had grade 1 partial tears of the medial and lateral collateral ligaments detected before the race, with no additional collateral ligament lesions detected after the race.
Eight runners had grade 1 knee joint effusions before the race, with all 10 runners developing grades 1 and 2 joint effusions after the race. The joint effusions decreased in 8 runners (grade 1) and disappeared completely in 2 at the 1-month follow-up scan. Two runners had pre-existing asymptomatic Baker's cysts, and another 2 had evidence of pre-existing partial soleal muscle tears.
The total score for all knee lesions in each runner on the pre-race scan was a mean of 2.1 (standard deviation (SD) 1.197); the immediate post-race scan score was 3.2 (SD 1.317), and the 1-month follow-up scan score was 2.3 (SD 1.16) (Table I). In 8 runners, the score increased from the pre- to immediate post-race scans, but decreased to the pre-race score levels in all runners on the 1-month follow-up scans. There was, however, no significant difference between the lesions detected on the 3 groups of scans (p=0.121). Inter-observer agreement by the two radiologists on scoring the MR studies was k=0.8, which is defined as good agreement.
Discussion
The knee images of all 10 Comrades runners showed abnormal amounts of joint fluid on the pre-race scans. Such fluid is nonspecific and can be associated with stress or injury to any type of knee structure. All runners but one had evidence of some old or new injury, and the joint fluid could have been a reaction to that injury.
Post-race, the changes in the amount of joint fluid followed the same trend as observed for the patellar and quadriceps tendon injuries: immediately following the race, the joint fluid appeared to have increased in half of the runners and remained unchanged in the other half. A month later, the joint fluid had decreased in half and remained unchanged in the other half.
When comparing the findings of the scans performed immediately after the race with those performed before the race, it is important to appreciate that all runners had participated in very intensive training and workout programmes before the ultra-marathon. Therefore, it was to be expected that old injuries and typical overuse injuries in the patellar and quadriceps tendon insertions would be detected on the pre-race scans. As a result, the number of runners who demonstrated partial tears (grade 1) on their post-race but not pre-race scans is small. However, in runners with evidence of previous partial tendon and ligament tears, their tendon or ligament injuries appear to have either deteriorated or remained unchanged after the race. It appears safe to conclude, therefore, that old tendon and ligament injuries as a result of isolated accidents or trauma do not predispose to overuse injuries precipitated by intensive training programmes or ultra-marathons. From our results, we conclude that overuse injuries in marathon running generally tend to subside or resolve after a rest of about 4 weeks. However, we are unaware of any continued training undertaken by the runners during that period.
The presence of a knee joint effusion probably relates to stress or injury. Although none of the runners had a known history of injury to the knee to be scanned, 8 had MR evidence of old injury to that knee. This study demonstrates that the presence of old injury does not predispose to acute MRI changes during the Comrades Marathon, with changes occurring regardless of the presence or absence of old injury. Our results are in general agreement with other marathon runner studies.5-11 No change in meniscal signal intensity and no significant increase in joint fluid were observed, but MRI evidence of partial tears was noted in the hamstring muscles and tendons. These findings contrast with results of studies on occasional joggers and non-athletes where there was no evidence of partial tears, but an increased meniscal signal in 50% of subjects, provided that the knee was scanned within minutes of the 30-minute jog.5
The meniscal signal may be a transient finding that has escaped the attention of investigators whose subjects were imaged 24 hours or more after the race.6 However, it is unlikely that joint fluid as a result of the marathon would significantly dissipate within a 24-hour period, which is confirmed by our study.
We believe that MRI evidence from trained marathon runners cannot be compared with that of recreational runners. Possibly the time elapsed between the end of the race and the post-race scan is of importance for detecting increased meniscal signal, but it is consistently absent in trained marathon runners. This also suggests an adaptation to marathon running stresses.6
Our study showed no evidence of bone bruises. Increased signal intensity within bone marrow has, however, been observed in MRI studies of the feet and ankles of marathon runners.9 As such areas are mostly located in regions atypical for stress-related oedema (bone bruise), these findings have been attributed to spots of increased haematopoietic activity as part of bone marrow hyperplasia in asymptomatic marathon runners.11,12 Their absence in our highly trained Comrades runners may suggest yet another adaptation to the stresses of marathon running.
The study confirmed our hypothesis that the Comrades Marathon aggravates the overuse injuries specific to marathon running and does not affect the MRI appearance of healed old injury. We also found no evidence that the presence of old injury contributes to the incidence or the extent of overuse injury. Scans before and after the race of all runners demonstrated normal cartilage and marrow, which confirms the view that damage to cartilage and bone bruising occurs primarily in the setting of traumatic events and is not part of overuse injury.
References
1. Noakes TD. Lore of Running. Cape Town: Oxford University Press Southern Africa, 2001. [ Links ]
2. Blazina ME, Kerlan RK, Jobe FW, et al. Jumpers knee. Orthop Clin North Am 1973; 4: 665. [ Links ]
3. Kaeding C, Tomczak R. Running injuries about the knee. Clin Podiatr Med Surg 2001; 200(18): 307-318. [ Links ]
4. Fadale PD, Hulstyn MJ. Common athletic knee injuries. Clin Sports Med 1997; 16(3): 479-499. [ Links ]
5. Kursunoglu-Brahme S, Schwaighofer B, Gundry C, et al. Jogging causes acute changes in the knee joint: An MRI study in normal volunteers. Am J Roentgenol 1990; 154: 1233-1235. [ Links ]
6. Shellock FG, Mink JH. Knees of trained long-distance runners: MR imaging before and after competition. Radiology 1991; 179: 635-637. [ Links ]
7. Mosher TM, Smith HE, Collins C, et al. Change in knee cartilage T2 at MR imaging after running: a feasibility study. Radiology 2005; 234: 245-249. [ Links ]
8. Scheuller-Weidekamm C, Schueller G, Uffmann M, Bader TR. Does running cause acute lesions of the knee? Evaluation with MR imaging. Eur Radiol 2006; 16: 2179-2185. [ Links ]
9. Lazzarini KM, Troiano RN, Smith RC. Can running cause the appearance of marrow edema on MR images of the foot and ankle? Radiology 1997; 202: 540-542. [ Links ]
10. Hohmann E, Wortler K, Imhoff AB. MR imaging of the hip and knee before and after marathon running. Am J Sports Med 2004; 32(1): 55-59. [ Links ]
11. Krampla W, Mayrhofer R, Malcher J, et al. MR imaging of the knee in marathon runners before and after competition. Skeletal Radiol 2001; 30: 72-76. [ Links ]
12. Shellock FG, Morris E, Deutsch AL, et al. Hematopoietic bone marrow hyperplasia: high prevalence on MR images of the knee in asymptomatic marathon runners. Am J Roentgenol 1992; 158: 335-338. [ Links ]
 Correspondence:
Correspondence:
A Rijke
(amr@virginia.edu)
Accepted 16 September 2008.














