Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 n.11 Pretoria Nov. 2008
SCIENTIFIC LETTERS
Accuracy of patients' self-reporting of pregnancy and awareness of risks to the fetus from X-ray radiation
Yousuf VadachiaI; Hein ElsII; Savvas AndronikouIII
IMB ChB, MMedRad (D). Private practice, Cape Town
IIMB ChB, MFamMed, CCFP. Department of Radiology, Tygerberg Hospital and Stellenbosch University, Tygerberg, W Cape
IIIMB BCh, FCRad, FRCR, PhD. Department of Radiology, Tygerberg Hospital and Stellenbosch University, Tygerberg, W Cape
To the Editor: Radiological investigations expose patients to ionising radiation, which may be harmful to a fetus that is inadvertently exposed. To prevent this female patients are asked whether they think they are pregnant. We attempted to determine the accuracy of patients' self-reporting of pregnancy and their awareness regarding the possible dangers of ionising radiation to the fetus. Patients need information and education regarding the risks of exposing a fetus to ionising radiation.
For adults the risk of cell damage from ionising radiation is low, and the benefits of diagnostic imaging should far outweigh the risk. Immature fetal cells are much more vulnerable to the harmful effects of ionising radiation,1,2 which may include early termination of pregnancy, teratogenic effects and a small increase in the risk of childhood cancers.2 These risks are small, as radiation doses used in diagnostic radiography are low.3,4 However, devices such as computed tomography (CT) scanners deliver much higher levels of X-ray radiation than conventional radiography, with a much higher dose to the patient and to the fetus if a female patient is pregnant.5,6
Preventing exposure of the fetus to X-ray radiation relies on patients reporting their pregnancy, or suspicion thereof. Radiographers also apply the '10-day rule' that restricts X-ray examinations to the first 10 days of the menstrual cycle when conception is considered least likely.1,7
Methods
A voluntary prospective questionnaire- and interview-based study was conducted of 125 female outpatients aged 18 - 42 years, referred to a tertiary imaging department for investigations. Participants' self-reporting of pregnancy was compared with the results of a urine pregnancy test. Participants were questioned about awareness of risks to the fetus from X-ray radiation and provided data regarding age, previous pregnancies, certainty of the date of their last menstrual period and contraception.
Using a precision of 8.8% for a 95% confidence interval in estimating a proportion from a population of N>500, a sample size of N=125 was calculated. This sample size was collected during the period of the study.
Data were analysed using Statistica 7. The negative predictive value, accuracy and sensitivity/specificity of the patients' answers regarding their pregnancy status compared with the pregnancy test (the 'gold standard' for the study) were determined and also analysed with a McNemar test. Comparing 2 variables a chi-square test was used to determine the p-value.
Results
All imaging modalities were included to give a cross-section of all patients presenting to the department. Most participants (77%) were referred for investigations using ionising radiation.
The mean age of the patients was 30.58 years and the median 31 years; 24 (19.2%) were nulliparous and 65 (52%) were not using contraception. Of 60 patients using contraception, 39 (65.0%) used injectable contraceptives, 19 (31.7%) oral contraceptives and 2 (3.3%) intrauterine devices. Of the 125 participants, 81 (64.8%) remembered the date of their last menstrual period with certainty. Of those who could not remember the date, 14 (31.8%) were not using a contraceptive. The 14 (11.2%) participants who were unsure of the date of their last menstrual period and not on contraception could be considered at high risk of being pregnant at the time of the survey. There was a significant statistical association (p=0.0001) between respondents using injectable contraceptives and being unable to recall the date of the previous menstrual period with certainty.
Of the 125 participants, 119 (95.2%) were certain they were not pregnant and had a negative pregnancy test, 4 (3.2%) were certain they were pregnant and had a positive pregnancy test, and 2 (1.6%) thought they were not pregnant but had pregnancy detected by a urine pregnancy test and subsequently confirmed by an ultrasound scan. Testing all the respondents yielded 6 positive results (4.8%), and of the 6 pregnant respondents 2 (1.6%) were unaware of their pregnant state. Patient self-reporting of pregnancy therefore had a negative predictive value of 98.3%, an accuracy of 98.4%, a specificity of 100% and a sensitivity of 66.7%.
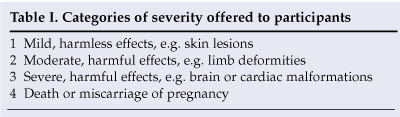
Of the 125 respondents, 71 (56.8%) thought that X-ray radiation was harmful to the fetus (of these 71.8% selected the first trimester as the most radiosensitive period of the pregnancy) and 54 (43.2%) thought it was not harmful. When asked to grade the severity of radiation exposure to the fetus (Table I), 40 (56.3%) of the 71 women who thought it was harmful chose severity category 3 and 16 (22.5%) severity category 4.
Discussion
Diagnosis of pregnancy on clinical grounds only is unreliable, especially in the early stages.7 Confounding patients' awareness of pregnancy and the menstrual cycle are factors such as previous pregnancies, irregular cycles and certain medications, especially injectable contraceptives. Taking injectable contraceptives correlates strongly with an inability to recall the date of the last menstrual period with certainty (p=0.0001). The number of our pregnant participants was insufficient to draw deductions regarding the impact of these factors on awareness of pregnancy. Two participants (1.6%) referred for brain CT scans, a high-dose investigation, were unaware that they were pregnant. The sensitivity and specificity of self-reporting of pregnancy were 66.7% and 100%, respectively; however, this must be qualified by the overall low prevalence of pregnancy in the sample population (4.8%).
Most participants (98.4%) were correct about whether or not they were pregnant. In our sample, direct questioning of patients regarding suspicion of pregnancy therefore had a high negative predictive value. However, 80.8% of the participants had been pregnant previously, with 33.6% having had 2 and 18.4% 3 previous pregnancies. Participants with experience of the symptoms of pregnancy would be expected to be more accurate in their awareness of being pregnant. Women in our respondents' age group (mean age 30.58 years) would also be likely to be aware of the symptoms of pregnancy, from their personal experience or from their peers.
Patients, attending physicians and radiologists vary widely in levels of awareness of the risks of radiation to the fetus.8-11 Of emergency room patients, only 7% had been informed of possible radiation risks, 100% were unable to estimate the radiation dose of a CT scan relative to a chest X-ray, and 3% believed that radiation increased the risk of childhood malignancies.9 Of mothers exposed to diagnostic radiation 25.5% considered their fetus to be at high risk for major malformations, a higher figure than in a control group.11 Family physicians perceived risk to be high, with 61% estimating the teratogenic risk following abdominal CT to be 5% or greater and 44% estimating the risk following an abdominal X-ray to be 5% or greater.8 Furthermore, 1% of family physicians would recommend termination of pregnancy following abdominal radiography and 6% following an abdominal CT scan.8 Patients' inadequate awareness and understanding of the effects of radiation has led to numerous medico-legal proceedings against hospitals following births of babies with congenital malformations thought to be due to prenatal diagnostic radiation.12
Our results are similar, with 56.8% of participants considering diagnostic X-rays to be harmful to the fetus, most stating that irradiation will cause severe effects or termination of pregnancy (of these 56.4% selected category 3 of severity and 22.4% category 4). Most participants in this group (71.8%) correctly selected the first trimester as the most radiosensitive period of gestation. Given the consensus that the X-ray dose in routine diagnostic radiation is too low to cause severe teratogenic effects, this is an inappropriately high perception of the risks.
Conclusions
Routine pregnancy testing of all female patients in the childbearing age range before a diagnostic X-ray is generally considered unnecessary, although some feel otherwise.13 It is prudent to have urine pregnancy test kits available and to offer the test to patients undergoing high-dose investigations or considered to have a high possibility of being pregnant.
Most of our patients overestimated the risks posed to the fetus by diagnostic X-ray imaging, and most correctly identified the most radiosensitive period of pregnancy. Some degree of patient awareness is therefore present, but it needs to be refined and ongoing patient education such as posters, brochures and presentations is needed.
References
1. Bushong SC. Radiologic Science for Technologists. St Louis: CV Mosby, 1975; 283-323. [ Links ]
2. International Commission on Radiological Protection Publication 90. Biological effects after prenatal irradiation (embryo and fetus). Annals of the IRCP 2003; 33: 7-9. [ Links ]
3. Lowe SA. Diagnostic radiography in pregnancy: Risks and reality. Aust N Z J Obstet Gynaecol 2004; 44: 191-196. [ Links ]
4. Toppenberg KS, Hill DA, Miller DP. Safety of radiographic imaging during pregnancy. Am Fam Physician 1999; 59(7): 1813-1820. [ Links ]
5. Osei EK, Faulkner K. Fetal doses from radiological examinations. Br J Radiol 1999; 860: 773-780. [ Links ]
6. Hurwitz LM, Yoshizumi T, Reiman RE, et al. Radiation dose to the fetus from body MDCT during early gestation. AJR Am J Roentgenol 2006; 186(3): 871-876. [ Links ]
7. Cunningham FG, Gant NF, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom KD. Williams Obstetrics. 21st ed. New York: McGraw-Hill, 2001: 22-29. [ Links ]
8. Ratnapalan S, Bona N, Chandra K, Koren G. Physicians' perception of teratogenic risk associated with radiography and CT during early pregnancy. AJR Am J Roentgenol 2004; 182(5): 1107-1109. [ Links ]
9. Lee CI, Haims AH, Monico EP, et al. Diagnostic CT scans: Assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 2004; 231(2): 393-398. [ Links ]
10. Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors' knowledge of radiation exposure: questionnaire study. BMJ 2003; 327: 371-372. [ Links ]
11. Bentur Y, Horlatsch N, Koren G. Exposure to ionizing radiation in pregnancy: perception of teratogenic risk and outcome. Teratology 1991; 43(2): 109-112. [ Links ]
12. Berlin L. Radiation exposure and the pregnant patient. AJR Am J Roentgenol 1996; 167(6):1 377-1380. [ Links ]
13. El-Khoury GY, Madsen MT, Blake ME, Yankowitz J. A new pregnancy policy for a new era. AJR Am J Roentgenol 2003; 181(2): 335-340. [ Links ]
 Correspondence:
Correspondence:
H Els
(els.hein@gmail.com)
Accepted 18 February 2008.














