Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 n.11 Pretoria Nov. 2008
SAMJ FORUM
CLINICAL IMAGES
Primary central nervous system lymphoma: An unusual presentation
J M HeckmannI; S O'RyanII; S CandyIII
IConsultant in the Division of Neurology, Department of Medicine
IIDepartment of Radiology, Groote Schuur Hospital and University of Cape Town
IIIPreviously worked in the Division of Neurology
Lymphocytic meningitis can be an unusual presentation of primary central nervous system lymphoma (PCNSL).
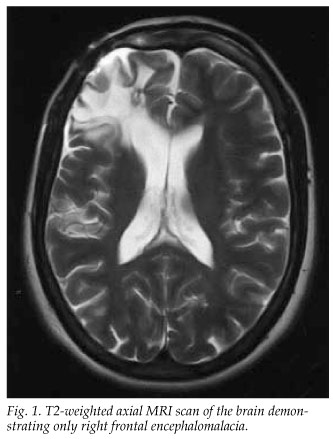
A 42-year-old woman presented with isolated right third nerve palsy and preceding lethargy. A previous head injury had required craniotomy, orbital reconstruction and medication to control the subsequent epilepsy. Apart from the pupillary-sparing third nerve palsy, the general and neurological examinations were normal. Magnetic resonance imaging (MRI) revealed post-traumatic right frontal cortical gliosis consistent with the previous trauma (Fig. 1). The remaining T2-weighted and FLAIR images were normal and did not demonstrate a cause of the third nerve palsy. Cerebrospinal fluid (CSF) investigations demonstrated a lymphocytic meningitic picture with 100 lymphocytes/µL no polymorphs, protein 1.08 g/l (normal <0.45 g/l), glucose 2.7 mmol/l (blood glucose 6.1 mmol/l) and 201 erythrocytes/µl, and were negative for tuberculosis, syphilis and cryptococcus. Three weeks later, she was referred for workup of the isolated right third nerve palsy, the unexplained lymphocytic meningitis and increasing drowsiness. A second CSF examination showed 14 lymphocytes/µl, protein 1.4 g/l, glucose 2.5 mmol/l, and an unhelpful cytological examination. A week later, she developed bilateral third nerve palsies with dilated pupils, and increasing drowsiness. An urgent computed tomography (CT) scan demonstrated extensive enhancing tissue in the periventricular and subependymal brain parenchyma (Fig. 2) extending into the midbrain area. A brain CT angiogram was normal. An endoscopic brain biopsy histological examination confirmed large B-cell lymphoma. High-dose methotrexate was commenced but the patient deteriorated and died 5 weeks after presentation.

Discussion
An unexplained increase in the frequency of PCNSL, which was previously considered to be rare, has been noticed over the last few decades in immunocompetent and older individuals.1 The incidence among AIDS and immunocompromised patients has also increased, and many tumours contain the Epstein-Barr virus genome, suggesting a pathogenetic role for the virus.2
Lymphoma can affect the central nervous system (CNS) as a primary neoplasm or, less frequently, as a metastatic spread of systemic lymphoma.1 PCNSL has a predilection for the brain parenchyma and tends to be periventricular,1 as in this case. Secondary CNS spread of systemic lymphoma occurs more commonly to the leptomeninges, particularly to the spinal cord, presenting with spinal cord compression syndromes.1 Diffuse large B-cell lymphomas comprise the majority of PCNSLs.1 Common presenting symptoms include mental state changes, hemiparesis, seizures and headaches.1 Cranial nerve palsy presentations are rare.3 CT and MRI images of PCNSL usually show one or several periventricular enhancing mass lesions.1
Our patient's initial uncontrasted brain MRI scan was normal. The tumour grew aggressively and, 4 weeks later, the uncontrasted CT brain image (not included) showed subependymal infiltrative tissue that markedly enhanced with contrast (Fig. 2). The point to note is that if an uncontrasted MRI scan does not show a cause of unexplained lymphocytic meningitis, contrasted images must be obtained. Cytological examination of the CSF is normal in up to 50% of cases.4 The dramatic change from the initial normal brain image within 4 weeks highlights that PCNSL can be a highly aggressive neoplasm.1
1. Ropper AH, Brown RH. Intracranial neoplasms and paraneoplastic disorders. In: Adams & Victor's Principles of Neurology. 8th ed. New York: McGraw-Hill, 2005: 560-565. [ Links ]
2. Bashir RM, Harris NL, Hochberg FH, Singer RM. Detection of Epstein-Barr virus in CNS lymphomas by in situ hybridization. Neurology 1989; 39: 813. [ Links ]
3. Jahnke K, Korfel A, O'Neill B, et al. International study on low-grade primary central nervous system lymphoma. Ann Neurol 2006; 59: 755-762. [ Links ]
 Correspondence:
Correspondence:
J M Heckmann
(jeanine.heckmann@.uct.ac.za)














