Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.11 Pretoria Nov. 2008
SAMJ FORUM
CLINICAL IMAGES
M R H Bayat; J Maharaj; F Vawda
The authors all have postgraduate radiology qualifications and worked in the Department of Radiology of the Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, at the time of writing
The clinical features of acute abdominal pain are often nonspecific, and surgery may be required to elucidate the correct diagnosis. Imaging modalities such as computed tomography (CT) scanning have proved invaluable in making diagnoses with relative accuracy and preventing unnecessary operative procedures.
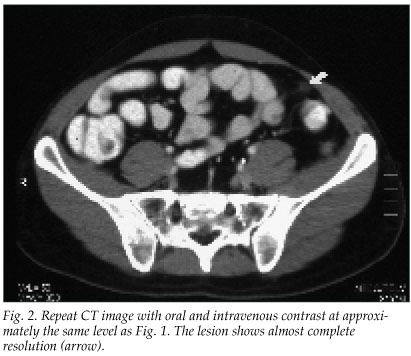
We describe the case of a 57-year-old man who presented with abdominal pain of subacute onset but worsening over the previous week. He had poor appetite, fever, rigors and constipation. He was pyrexial and had a tachycardia, localised tenderness over the left iliac fossa and a mild leucocytosis. A well-defined 1x1.5 cm oval ring of soft-tissue attenuation surrounding a central area of fatty attenuation was noted on CT scan (Fig. 1). Its posterior aspect was closely related to the adjacent distal sigmoid colon and it appeared anteriorly adherent to the parietal peritoneum. A diagnosis of primary epiploic appendagitis (EA) was made on the CT findings. The patient was discharged with analgesia. A repeat CT scan was done 2 weeks later (Fig. 2).

Discussion
The epiploic appendices are small pedunculated protuberances of fat located on the antimesenteric serosal surface of the colon along the teniae coli, predominantly along the caecal and sigmoid colon.1 These are not normally seen on CT scans unless ascites is present or there is peritoneal contrast.1,2
Many clinicians have not heard of EA. In a series of 33 cases, all patients presented with abdominal pain, 45% had localised tenderness, and 53% had mild leucocytosis.3 Prior to its identification on imaging, EA was considered quite rare. The diagnosis was only made retrospectively in those patients who had surgical intervention.4 Depending on the EA site, the clinical features commonly mimic acute appendicitis or diverticulitis. EA has been reported to have an incidence of 2.3 - 7.1% in patients clinically suspected of having diverticulitis.2 It is characterised pathologically by inflammatory changes within the epiploica secondary to infarction, which may be the result of spontaneous thrombosis or torsion of the draining vein.2,5
The thin hyperdense enhancing rim measuring 1 - 2 mm seen on post-intravenous contrast CT images is pathognomonic.1-3,5-7
The central area enclosed by the hyperattenuating ring is always of fatty density.5,6 Follow-up CT scan after treatment characteristically demonstrates complete resolution in EA.
Based on the imaging features, the differential diagnosis includes segmental omental infarction, secondary EA and peritoneal metastasis. Segmental omental infarction and primary EA have similar clinical features and the same treatment.1,7 The 'hyperattenuating ring sign' is seen in both primary and secondary EA. Secondary EA is caused by contiguous inflammatory changes of the appendices epiploicae as a result of pathology within an adjacent organ. Depending of the location of the EA, associated diverticulitis, appendicitis or cholecystitis must be excluded. The treatment of secondary EA should be directed at the underlying cause. Peritoneal metastasis is another possible imaging mimic, usually with involvement of multiple rather than single epiploica.
The treatment for primary EA is simple analgesia followed by a repeat CT scan to confirm response to therapy, which differs considerably from the other clinical differentials and reduces costs.6
1. van Breda Vriesman AC. The hyperattenuating ring sign. Radiology 2003; 226: 556-557. [ Links ]
2. Sandrasegaran K, Maglinte DD, Rajesh A, Akisik FM. Primary epiploic appendagitis: CT diagnosis. Emerg Radiol 2004; 11: 9-14. [ Links ]
3. Zissin R, Hertz M, Osadchy A, Kots E, Shapiro-Feinberg M, Paran H. Acute epiploic appendagitis: CT findings in 33 cases. Emerg Radiol 2002; 9: 262-265. [ Links ]
4. Shamblin JR, Payne CL, Soileau MK Infarction of an epiploic appendix. S Afr Med J 1986; 79: 374-375. [ Links ]
5. Mollà E, Ripollés T, Martinez MJ, Morote V, Roselló-Sasre E. Primary epiploic appendagitis: US and CT findings. Eur Radiol 1998; 8: 435-438. [ Links ]
6. Rao PM, Rhea JT, Wittenberg J, Warshaw AL. Misdiagnosis of primary epiploic appendagitis. Am J Surg 1998; 176: 81-85. [ Links ]
7. Mcclure MJ, Khalili K, Sarrazin J, Hanbridge A. Radiological features of epiploic appendagitis and segmental omental infarction. Clin Rad 2001; 56: 819-827. [ Links ]
 Correspondence:
Correspondence:
M R H Bayat
(mrbayat@mailbox.co.za)














