Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 n.10 Pretoria Oct. 2008
ORIGINAL ARTICLES
Male circumcision and its relationship to HIV infection in South Africa: Results of a national survey in 2002
Catherine ConnollyI; Leickness C SimbayiII; Rebecca ShanmugamIII; Ayanda NqeketoIV
IMPH. Medical Research Council, Durban
IIMSc. Medical Research Council, Durban
IIIDPhil. Human Sciences Research Council, Cape Town
IVBA Hons. Human Sciences Research Council, Cape Town
ABSTRACT
OBJECTIVE: To investigate the nature of male circumcision and its relationship to HIV infection.
METHODS: Analysis of a sub-sample of 3 025 men aged 15 years and older who participated in the first national population-based survey on HIV/AIDS in 2002. Chi-square tests and Wilcoxon rank sum tests were used to identify factors associated with circumcision and HIV status, followed by a logistic regression model.
RESULTS: One-third of the men (35.3%) were circumcised. The factors strongly associated with circumcision were age >50, black living in rural areas and speaking SePedi (71.2%) or IsiXhosa (64.3%). The median age was significantly older for blacks (18 years) compared with other racial groups (3.5 years), p <0.001. Among blacks, circumcisions were mainly conducted outside hospital settings. In 40.5% of subjects, circumcision took place after sexual debut; two-thirds of the men circumcised after their 17th birthday were already sexually active. HIV and circumcision were not associated (12.3% HIV positive in the circumcised group v. 12% HIV positive in the uncircumcised group). HIV was, however, significantly lower in men circumcised before 12 years of age (6.8%) than in those circumcised after 12 years of age (13.5%, p=0.02). When restricted to sexually active men, the difference that remained did not reach statistical significance (8.9% v. 13.6%, p=0.08.). There was no effect when adjusted for possible confounding.
CONCLUSION: Circumcision had no protective effect in the prevention of HIV transmission. This is a concern, and has implications for the possible adoption of the mass male circumcision strategy both as a public health policy and an HIV prevention strategy.
With an estimated 5.6 million people living with HIV/AIDS, South Africa now ranks second-highest in the world after India.1 Although the prevalence rates among both the general public and pregnant women appear to have peaked, incidence rates suggest that a relatively high level of new HIV infections is still taking place, especially among young women.2,3
The notion that male circumcision could be protective against HIV infection was first suggested over two decades ago.4 Since then, numerous ecological, observational and cohort studies have produced mixed findings. A meta-analysis of 27 studies from sub-Saharan Africa showed a reduced risk of HIV in circumcised men compared with uncircumcised men (risk ratio (RR) 0.52, confidence interval (CI) 0.2 - 0.42).5 However, the Cochrane Review found no effect.6 There are currently 3 randomised control intervention trials on male circumcision which offer the strongest evidence available so far that male circumcision can reduce HIV transmission by between 48 and 60%.7-9
Biological data also provide evidence that circumcision could be protective in preventing HIV infection among males. Circumcision is thought to have some protective effect on the spread of diseases such as penile carcinoma, urinary tract infections, and ulcerative sexually transmitted diseases, especially chancroid and syphilis.10 In circumcision, the remaining external foreskin found in most men has very few target cells for HI viruses to attach to, and also greatly increased keratinisation compared with the internal and exterior surfaces of the foreskin in uncircumcised men.11 While removal of the foreskin certainly does not eliminate the risk of HIV infection, it does remove the most susceptible area, thereby reducing the probability of HIV infection. However, there is some recent evidence that the protective claims of circumcision have been overstated.12
Various forms of circumcision have been practised for many generations among several indigenous ethnic groups in sub-Saharan Africa.13 In South Africa, male circumcision is performed mainly on youth as a part of initiatory rites of passage into manhood, primarily among the Xhosa and South Sotho, as well as the Ndebele, Pedi and Venda.10,13,14 Male circumcision at birth is also generally performed on Jewish and Muslim babies.10,13
Subject age and the setting where circumcision was performed may, however, affect the protection it offers in the general male population of South Africa. Firstly, pre-pubertal circumcision has been shown to be associated with reduced HIV and STI risk, unlike circumcision after age 20 years.15
Secondly, most circumcisions among indigenous ethnic groups in South Africa are conducted under unsterile conditions.9,11,12 In addition, other cultural practices may be linked to an increased risk of HIV infection. For example, circumcised males in some ethnic groups are encouraged to engage in unprotected pre-marital sex for sexual exploration, or to prove their virility by impregnating a woman.13 Clearly, the potential benefits of circumcision during late adolescence may be diminished by such factors.
The Nelson Mandela/HSRC Survey reported that 35% of all adult and young males were circumcised at a mean age of circumcision of 15 years (median 17 years).2 Preliminary analysis of these data showed that male circumcision was more protective among other population groups, such as whites, Indians and coloureds, than among blacks, but confounding by variables such as age of circumcision or risky sexual behaviour was not taken into account (cf. poster by Connolly, Shisana, Simbayi and Colvin as part of their presentation 'HIV and circumcision in South Africa' at the XV International AIDS Conference, held in Bangkok, Thailand, in 2004). Our study looks firstly at demographic and behavioural factors associated with male circumcision in South Africa, and secondly at whether or not there is an association between circumcision and HIV infection.
Methods
A cross-sectional, national household-based, community survey was conducted in 2002. A complex multi-stage probability sampling technique was used to create a master sample of 1 000 census enumerator areas (EAs) from 86 000 EAs available from the 2001 census in South Africa. Of a total of 13 528 possible respondents, 9 963 (73.7%) persons >2 years of age agreed to be interviewed (via proxy for children <11 years), and 8 428 were tested for HIV. HIV testing was done using the Orasure HIV-1 Oral Specimen Collection Device. The Vironostika HIV UNI-Form II plus O Elisa test was used to determine HIV status. No confirmatory test was done on HIV-positive results. A more detailed account of the methodology used is presented elsewhere.16 Ethical approval was obtained from the Human Sciences Research Council's Interim Research Ethics Committee.
Statistical analysis
Demographic and behavioural factors associated with circumcision were analysed using chi-square tests and Wilcoxon sign rank tests. Stepwise logistic regression analysis was then used to identify independent factors associated with circumcision. Similar techniques were used to examine the association between circumcision and HIV infection. STATA (Stata Corp., 2002, College Station, Texas, USA) was used for the analysis.
Results
Description of the sample
A subgroup of 3 025 men aged 15 years and older who participated in the study were included in the analysis (Table I). The majority of them were black (58.5%), aged <25 years (58.7%), and in formal urban areas (59.5%). Over 50% of them were Christian; there were only 3 Jewish (0.1%) and 125 Moslem (4.1%) subjects. Response rates were low among residents in urban formal areas (61.4%) and more specifically 48.9% among whites and 56.1% among Indians. Therefore, these subgroups may not be representative of the general population. The most common home language was Afrikaans (which was spoken by 23.2% of the sample), followed by English (spoken by 19.3%). Slightly more than a third of the men (35.3%; N=1 067) were circumcised.
Determinants of male circumcision
Table II shows a summary of the associations between the various socio-demographic characteristics and circumcision status. Circumcision rates were highest in men aged >50 years, and lowest in the age group 15 - 24 years; more blacks were circumcised than in other racial groups; and circumcision varied widely by province, from a low of 13.1% in Northern Cape to 69.4% in Limpopo. In Eastern Cape, a province where the practice of traditional circumcision is common, only 56% were circumcised (see Fig. 1). The table also shows that rural respondents were more likely to be circumcised than those in urban areas, as were sexually active men.

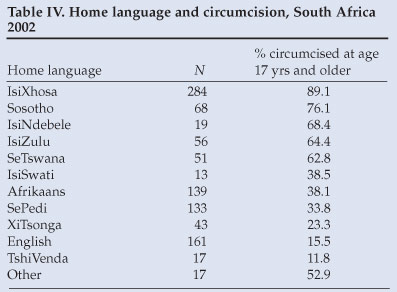
As expected, Islamic and Jewish religions were strongly associated with circumcision while other religions showed little variation. There were also strong associations between circumcision and the language spoken at home, with respondents who spoke IsiNdebele, IsiXhosa, SePedi and TshiVenda and XiTsonga all having higher rates of circumcision, followed by those who spoke English, Sesotho, SaBorwa and other, while IsiZulu speakers had the fewest circumcised men. Ethnic groups with high rates of circumcision were among those known to practise traditional forms of circumcision, namely the AmaNdebele, BaPedi, BaVenda and BaTsonga people (who are primarily in the northern provinces of Limpopo, Mpumalanga and Gauteng) and the AmaXhosa who mainly reside in Eastern Cape.
Following a stepwise logistic regression model, age over 25 years, religion (Islam/Jewish), population group (Indian) and home language remained significantly associated with circumcision. Because of the correlation between province and home language, province was excluded from the model.
Age of circumcision and place, race and language group
Of the 1 067 men >15 years of age who were circumcised, the majority (57.2%) were circumcised in the mountains or the bush, at initiation school or at home, while the remainder (42.8%) were circumcised in hospital. The vast majority of circumcised whites (97.8%), Indians (92.8%) and coloureds (87.4%) had been circumcised in hospital, compared with 21.8% of blacks.
The age of circumcision varied both by race and setting of circumcision. The median age of circumcision of blacks was 18 years, compared with 10 years for coloureds, 2 years for whites, and 1 year for Indians. Over 75% of whites and Indians were circumcised before the age of 12, compared with only 17% of blacks and 57% of coloureds (see Table III). The median age of those circumcised outside of hospital was significantly greater than those in hospital for blacks (18.3 years v. 16 years, p<0.001) and coloureds (18 years v. 10 years, p=0.001). The numbers of whites and Indians circumcised outside of hospital were too small for comparisons.
The practice of post-pubertal circumcision varied by home language. Among IsiXhosa speakers, 64% were circumcised, and >89% of those had been circumcised after their 17th birthday. The TshiVenda-speaking people, a relatively small ethnic group mainly in the northern part of the Limpopo Province, had an overwhelming majority (90.5%) of men who were circumcised, mostly before the age of 17 years (see Tables II and IV).
Circumcision and sexual debut
The median age of sexual debut among all the men was estimated as 18.9 years. Circumcision took place after the start of sexual activity among 40.5% of all the men. Of those circumcised after their 17th birthday, two-thirds (66.5%) had started sexual activity prior to circumcision.
Association between circumcision and HIV infection
Of the 3 025 men in the study, 2 585 had a valid HIV result. HIV prevalence was equal among circumcised and uncircumcised men (11.1% v. 11.0%). When the analysis was restricted to sexually active men, circumcision still showed no protective effect (12.3% v. 12.0%). Age of circumcision was available for 866 of the 961 sexually active circumcised men (95%). Men circumcised before the age of 12 had a lower HIV prevalence (6.8%) than men circumcised after the age of 12 (13.5%) (odds ratio (OR) 0.5, CI 0.3 - 0.8, p<0.01), but not when compared with uncircumcised men (OR 0.8, CI 0.6 - 1.1, p=0.1). Among sexually active men, the prevalence remained lower among men who had been circumcised before the age of 12 (8.9%) compared with those circumcised after the age of 12 (13.6%), but the difference did not reach statistical significance (OR 0.6, CI 0.4 - 1.1, p=0.08). When blacks were examined separately, HIV prevalence was 16.7% for men circumcised before the age of 12, compared with 15.2% for those circumcised after the age of 12 (OR 0.9, CI 0.5 - 1.7, p=0.7), and 17.9% for those uncircumcised (OR1.1, CI 0.6 - 2.0, p=0.8) (Table V). The effect of circumcision remained unchanged when adjusted for condom use, marital status, age and educational level for men circumcised before the age of 12 ( OR 0.9, CI 0.5 - 1.7, p=0.7) and for men circumcised after the age of 12 (OR 0.8, CI 0.6 - 1.1, p=0.2), compared with uncircumcised men. The differences among the coloured population were not significant, and remained so when adjusted for possible confounders. Whites and Indians were excluded because only a few were circumcised after 12 years of age.
Among sexually active black men, the circumcision setting was not associated with HIV prevalence (bush/home (15.4%) v. hospital (15.1%), p=0.9).
Discussion
The first key finding from this study was that male circumcision does not appear to be protective against HIV infection among men in South Africa, irrespective of whether they are sexually active or not. This finding is inconsistent with the bulk of findings in the literature.5-8 The recent randomised control trials (RCTs) show that while circumcision is protective, it does not offer complete protection. The further finding that 2 out of 5 men were circumcised after their sexual debut suggests that any possible benefit of male circumcision might have been reduced by sexual contact prior to circumcision with young females, who in South Africa have a very high HIV prevalence. A similar explanation was given by Auvert:17 circumcision was found to be protective in Kisumu, Kenya, compared with Ndola in Zambia where it had no effect.
Although descriptions of circumcision practices appear in anthropological literature,10,13 the strength of this study is that it describes in more detail the determinants of male circumcision in South Africa, and is based on a large cross-section of data of the South African population. From our study, male circumcision was associated with increasing age, black race, religious affiliation, home language and province. Most circumcisions among whites and Indians were performed in childhood in hospital settings, whereas the greater proportion among blacks was performed after the age of 17 and outside a hospital setting. Circumcision was also more common among speakers of IsiNdebele, IsiXhosa, SePedi, TshiVenda and XiTsonga and residents of Limpopo, Mpumalanga, Gauteng and Eastern Cape provinces, correspondingly.13,14 A surprising finding was that more BaVenda men were circumcised than AmaXhosa men. In Xhosa culture, a man is not accepted as a man unless or until he is circumcised. Indeed, it is not uncommon for uncircumcised men to be ostracised by other men during discussions about manhood. In turn, some old or even elderly men have to undergo circumcision later in life to finally gain acceptance of their masculinity by other Xhosa men.14
The last key finding is the high proportion of post-pubertal circumcisions done outside of a hospital setting. This is a major source of concern as, in the past, most traditional circumcisions were performed in the bush by traditional practitioners without adequate infection control measures, possibly increasing the risk of HIV infection.3,10,13,14 Steps have already been taken in this area, and joint initiatives already exist between Western and traditional health systems which have successfully resulted in fewer botched circumcisions and the saving of lives of young initiates, compared with the past.10,13,14
The above findings must be seen within the various limitations of the present study. Firstly, the study is based on a cross-sectional study design, which cannot show a temporal relationship. Secondly, information on circumcision was self-reported and might have been influenced by imperfect recall and influences of social desirability as to when and where circumcision had taken place. Also, the interviews were conducted by Western-trained nurses, and some men might have been reluctant to discuss circumcision with them.
More research, especially of the operational type, is clearly needed on the feasibility of implementing a policy of mass male circumcision in communities where traditional circumcision may be done too late to offer the maximum protection, and the long-term protection of circumcision may be eroded by risky sexual behaviour.
This study was based on the database obtained from the Nelson Mandela/HSRC Study of HIV/AIDS in South Africa2 which was conducted in 2002 as a collaborative effort between the following institutions: The Human Sciences Research Council (HSRC), Medical Research Council (MRC) of South Africa, the Centre for AIDS Development, Research and Evaluation (CADRE), the Joint United Nations Programme on HIV/AIDS Regional Support Team for Eastern and Southern Africa (UNAIDS-RST ESA), the Agence Nationale de Recherches sur le Sida (ANRS) and Geospace International. The authors thank the Nelson Mandela Foundation, the Nelson Mandela Children's Fund, The Swiss Agency for Development and Cooperation, and the HSRC for financial support for the original study.
References
1. Statement on Kenyan and Ugandan trial findings regarding circumcision and HIV: Male circumcision reduces the risk of becoming infected with HIV, but does not provide complete protection (13 December 2006). Geneva: WHO/UNFPA/UNICEF/World Bank/UNAIDS. http://www.who.int/mediacentre/news/statements/2006/s18/en/index.html (accessed 18 June 2007) [ Links ]
2. Shisana O, Simbayi L. Nelson Mandela/HSRC Study of HIV/AIDS: South African National HIV Prevalence, Behavioural Risks and Mass Media Household Survey 2002. Cape Town: Human Sciences Research Council Press, 2002. [ Links ]
3. Shisana O, Simbayi LC, Parker W, et al. Nelson Mandela/HSRC Study of HIV/AIDS: South African National HIV Prevalence, HIV Incidence, Behaviour and Communication, 2005. Cape Town: Human Sciences Research Council Press, 2005. [ Links ]
4. Fink AJ. A possible explanation for heterosexual male infection with AIDS. N Engl J Med 2005; 315: 1167. [ Links ]
5. Weiss HA, Quigley MA, Hayes R. Male circumcision and risk of HIV infection in sub-Saharan Africa: A systematic review and meta-analysis. AIDS 2000: 14; 2361-2370. [ Links ]
6. Siegfried N, Muller M, Volmink J, et al. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane Library, Issue 3, 2003. Oxford: Update Software. [ Links ]
7. Auvert B, Taljaard D, Lagarde E, et al. A randomised, controlled intervention trial of male circumcision for reduction of HIV infection risk: The ANRS 1265 trial. PLoS Medicine 2005: 2(11) e298; 1112-1122. [ Links ]
8. Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised trial. Lancet 2007; 369: 643-656. [ Links ]
9. Grey RJ, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007; 369: 657-666. [ Links ]
10. Mayatula V, Mavundla TR. A review of male circumcision procedures among South African Blacks. Curationis 1997; 20 (3): 16-20. [ Links ]
11. Male Circumcision: Current Epidemiological and Field Evidence; Program and Policy Implications for HIV Prevention and Reproductive Health. Conference Report 2003. Washington, DC: USAID, 2003. [ Links ]
12. Myers A, Myers J. Male circumcision - A new hope? S Afr Med J 2007; 97: 338-341. [ Links ]
13. Simbayi L. Psychosocial and cultural determinants of HIV/AIDS in the SADC region (Chapter 3). HIV/AIDS in Southern Africa: A review paper. Prepared for the WK Kellogg Foundation by the HSRC's Social Aspects of HIV/AIDS and Health Programme. Cape Town: Human Sciences Research Council Press, 2002. [ Links ]
14. Meissner O, Buso DL. Traditional male circumcision in the Eastern Cape - scourge or blessing? S Afr Med J 2007; 97: 371-373. [ Links ]
15. Kelly R, Kiwanuka N, Wawer MJ, et al. Age of male circumcision and risk of prevalent HIV infection in rural Uganda. AIDS 1999; 13: 399-405. [ Links ]
16. Shisana O, Stoker DJ, Simbayi LC, et al. South African National Household Survey of HIV/ AIDS Prevalence, Behavioural Risks and Mass Media Impact: Methodology & Prevalence. S Afr Med J 2004: 94; 283-288. [ Links ]
17. Auvert B, Buve A, Lagarde E, et al. (For the Study Group on the Heterogeneity of HIV Epidemics in African cities (2001)). Male circumcision and HIV infection in four cities in Sub-Saharan Africa. AIDS 2001; 15 (Suppl. 4): S31-S40 [ Links ]
 Correspondence:
Correspondence:
C Connolly
(cconnolly@mrc.ac.za)
Accepted 6 December 2007.














