Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.9 Pretoria sep. 2008
ORIGINAL ARTICLES
The quality of operative notes at a general surgery unit
A RogersI; M BuntingII; A AtherstoneIII
IMB ChB; Department of Surgery, Frere Hospital, East London, E Cape
IIMB ChB, FCS (SA); Department of Surgery, Frere Hospital, East London, E Cape
IIIMB ChB, FRCS; Department of Surgery, Frere Hospital, East London, E Cape
ABSTRACT
AIM: With the increasingly litigious nature of medical practice, accurate documentation is critical. This is particularly true for operative procedures, and medical councils have identified this and published guidelines to aid surgeons. However, these remain a frequently cited weakness in their defence in medico-legal cases. This study assessed the accuracy of operative notes in a general surgery unit in order to improve our practice.
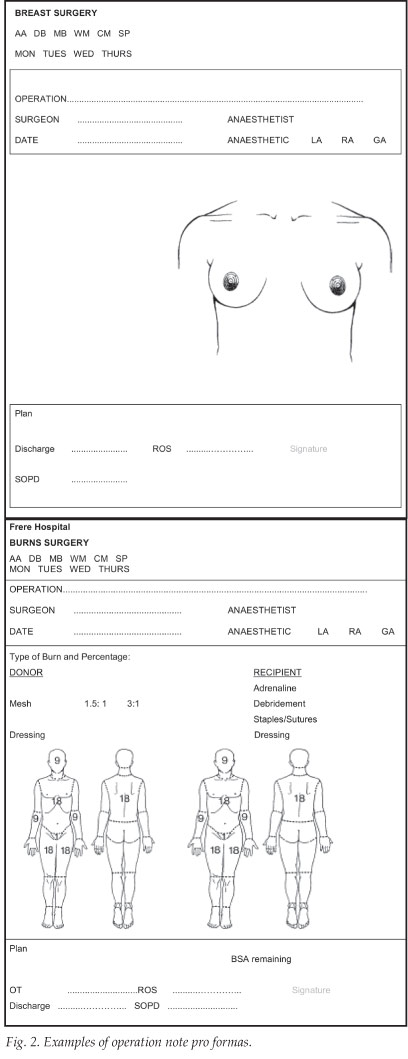
METHOD: An audit of 100 consecutive operative notes was performed, and notes were assessed using the Royal College of Surgeons guidelines. The quality of note-taking of trainees was compared with that of consultant surgeons. A series of operation note pro formas was designed in response to the findings.
RESULTS: Of the notes, 66% were completed by trainees. The vast majority of notes had no diagram to demonstrate the surgical findings or illustrate the actions. Specialist surgeons were more likely to describe the actions accurately, but less likely to describe wound closure methods or dressings used. They were also less likely to complete adequate postoperative orders.
CONCLUSIONS: This study identifies key areas of weakness in our operative note-keeping. Pro formas should be introduced and made available for commonly performed procedures, and diagrams should be used wherever possible.
Medical councils around the world advise doctors to keep accurate, comprehensive, contemporaneous medical notes. These principles apply in all areas of patient care, not least at times when complications and risks are more prevalent, such as during operations.1 The Royal College of Surgeons of England (RCS), for instance, published guidelines encouraging surgeons to:
'Ensure that there are legible operative notes (typed if possible) for every operative procedure. The notes should accompany the patient into recovery and to the ward and should be in sufficient detail to enable continuity of care by another doctor. The notes should include:
- date and time
- elective/emergency procedure
- the names of the operating surgeon and assistant
- the operative procedure carried out
- the incision
- the operative diagnosis
- the operative findings
- any problems or complications
- any extra procedure performed and the reason why it was performed
- details of tissue removed, added or altered
- identification of any prosthesis used, including the serial numbers of prostheses and other implanted materials
- details of closure technique
- postoperative care instructions, and
- a signature.'
In 1992, the UK National Enquiry into Perioperative Deaths noted a considerable variation in the quality of operation notes.2 Previous audits of the quality of operation notes have identified various areas of weakness applicable to all surgical specialties. For instance, postoperative instructions were missing in as many as two-thirds of cases; trainees outscored consultants in almost every criterion in one study; and emergency operation notes scored better than elective. In another audit, more than two-thirds of the consultant's operation notes were illegible to those expected to make decisions about the patient's care.3
To combat some of these problems, several units have introduced specially standardised pro formas, with prescribed headings to act as aides mémoire. Two ENT units have recently demonstrated an improvement in all criteria following such a measure.3-5 A study of caesarean section notes in a London hospital showed that there had been significant improvements in almost all items assessed after the introduction of a dedicated 'operative delivery note'. Prior to its introduction, less than 80% of case notes documented skin incision time and type, surgical findings, type of uterine incision, presenting part, explanation of fetal delivery, uterine cavity check, presence of paediatrician, adnexal check, and complete sutures used.6 A computerised database introduced for the entry of orthopaedic surgery was shown to be flexible and inexpensive.7
Methods
A retrospective audit of 100 sets of consecutive operation notes was conducted at Frere Hospital, the notes being analysed using the RCS Guidelines. A series of A4 page-size operation note pro formas were designed in response to the results obtained, to be used for commonly performed procedures. Appropriate anatomical diagrams were included with clearly headed areas for particular details of the surgery and postoperative planning.
A medical officer or registrar wrote 66% of the operation notes; a specialist completed 34%. Cases were divided into categories according to the degree of urgency:
- Elective (e.g. laparoscopic cholecystectomy, lipoma excision, incisional hernia, closure of colostomy, etc.) - 26%
- Urgent (e.g. mastectomy, amputation for gangrene) - 36%
- Emergency (e.g. appendicectomy, laparotomy for penetrating abdominal trauma) - 26%
- Burns - 12%.
Results
Every note had the surgeon's name and signature and the assistant's name clearly written. On only 2 notes out of 100 was the date absent or incorrect. Information regarding the diagnosis and indication for the operation was included in 68% of cases. The surgical approach or incisions made was outlined accurately in only 74% of cases. The operation findings and actions were clearly described in 74% and 84% of cases, respectively. Only 60% included adequate details about the nature of prostheses used; 69% had comprehensive details about specimens taken, marked for or sent to the pathology service; abbreviations were used in 20%; and only 72% included complete information about the form of suture or wound closure method. Most cases had no diagram included, and 70% had no information about the type of dressing used.
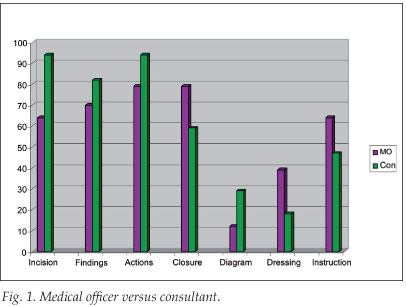
Only 58% of the operation notes had postoperative instructions clearly written on the note (Fig. 1).
Discussion
Specialists were more likely to accurately describe the incision, findings and actions of the procedure, but less likely to include accurate information about the suture used for closure, the dressing used, or the postoperative instructions. Specialists included diagrams of the procedure in their operation notes more frequently. Medical officers perform the vast majority of emergency surgery in our setting. This type of surgery, as well as the urgent surgery category (more often performed by specialists), was shown to include the best operation notes. Elective and burns surgery (more often completed by specialists and medical officers, respectively) were the types worst described and with the notes least accurate.
With the increasingly litigous nature of modern medical practice, doctors have been forced to practise defensive medicine. Potential areas of weakness in our practice need to be identified and rectified timeously. Operation notes could be easier to interpret if, wherever possible, there were diagrams; this reduces the reliance on doctors' descriptive abilities to portray the necessary information. The addition of prescribed headings to act as aides mémoire would reduce the likelihood of the operative surgeon not including detailed information about wound closure, suture type and postoperative instructions (Fig. 2).
References
1. Good Medical Practice. London: General Medical Council, 1998. [ Links ]
2. Campling EA, Devlin HH, Hoile RW, Lunn JN. The Report oof the National Confidential Enquiry into Perioperative Deaths 1992/1993. London: National Confidential Enquiry into Perioperative Deaths, 1995. [ Links ]
3. Baigrie RJ, Dowling BL, Birch D, Dehn TC. An audit of the quality of operation notes in two district general hospitals. Are we following the Royal College guidelines? Ann R Coll Surg Engl 1994; 76(1): suppl, 8-10. [ Links ]
4. Bateman ND, Carney AS, Gibbin KP. An audit of the quality of operation notes in an otolaryngology unit. J R Coll Surg Edinb 1999; 44(2): 94-95. [ Links ]
5. Shayah A, Agada FO, Gunasekaran S, Jassar P, Egland RJ. The quality of operative note taking: An audit using the Royal College of Surgeons Guidelines as the gold standard. Int J Clin Pract 2007; 61(4): 677-679. [ Links ]
6. Nicopoullos JD, Karrar S, Gour A, Panter K. Significant improvement in quality of caesarean section documentation with dedicated operative proforma - completion of the audit cycle. J Obstet Gynaecol 2003; 23(4): 381-386. [ Links ]
7. Barlow JW, Flynn NA, Britton JM. The Basingstoke Orthopaedic Database: A high quality accurate information system for audit. Ann R Coll Surg Engl 1994; 76: Suppl 6, 285-287. Accepted 11 January 2008. [ Links ]
 Correspondence:
Correspondence:
A Rogers
(rogersadr@gmail.com)
Accepted 11 January 2008














