Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 n.8 Pretoria Aug. 2008
ABSTRACTS
SAGES 2008 - 'Trends in Gastroenterology'
Friday 8 August - Monday 11 August 2008, Cape Town International Convention Centre
Oral Presentations
46th Annual Congress of the South African Gastroenterology Society in association with the South African Society of Endoscopic Surgeons and the South African Gastrointestinal Nurses Society (in order of presentation)
Gastro-oesophageal reflux is not responsible for the majority of recurrent heartburn and new reflux related symptoms post fundoplication
Kruger FC; Botha JEC; Van Heerden N; Amman M
Durbanville Mediclinic, W Cape
BACKGROUND: In a study by Spechler et al. 62% of patients were taking anti-reflux medication post fundoplication (PF). Currently patients with recurrent and new GORD related symptoms PF tend to be treated empirically with PPIs. Data supporting this approach are lacking.
In this study we aim to determine whether gastroesophageal reflux was responsible for recurrent heartburn or new symptoms related to GORD in patients PF.
METHODS AND STUDY POPULATION: We analysed 33 ambulatory MII-pH study results of patients with recurrent and new GORD symptoms PF. These patients were referred to our laboratory between September 2006 and May 2008. A MII pH result was considered positive if there were abnormal esophageal acid exposure in the upright or recumbent position, increased reflux episodes (>73 reflux episodes) or a positive symptom index (SI >50%).
The age of the patients ranged between 21 years and 80 years with a mean age of 43 years. 63.6 % of the patients were female. The time interval for the onset of symptoms PF ranged from 7 months to 18 years with an average of 5.1 years. Thirteen patients (39.3%) had recurrent heartburn and 20 patients (60,6%) had new symptoms related to GORD. The new symptoms were chest pain, dysphagia, odynophagia, abdominal pain, epigastric pain, early satiety, choke, globus, cough, throat clearing and hoarseness. Four patients were on PPI therapy, all 4 in the new symptom group.
RESULTS:
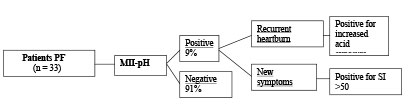
CONCLUSION: In this study we showed that the vast majority of patients with recurrent heartburn or new symptoms related to GORD did not have gastro-oesophageal reflux as the cause of their symptoms. We therefore advise against empiric use of PPI therapy in symptomatic PF patients.
On the basis of our findings we also advise patients to have proof of a positive pH-and or Impedance study before undergoing a Nissen fundoplication.
Self-expanding metal STENTS (SEMS) as a primary modality of treatment for malignant gastric outlet obstruction in cape town
Shaw JM; Panieri E; Van Wyk MEC; Bornman PC
Department of Surgery, University of Cape Town and Groote Schuur Hospital
AIM: To prospectively evaluate the use of SEMS as a primary intervention for relieving malignant gastric outlet obstruction in a resource limited environment in South Africa.
BACKGROUND: Gastro-duodenal obstruction secondary to advanced malignancy is often a difficult symptom to palliate. Surgical bypass is frequently inappropriate or contraindicated due to advanced disease or co-morbidity. Primary stenting aims to rapidly restore enteral intake with minimal morbidity. SEMS enables patients with limited life expectancy to be independent of parenteral fluid administration and facilitates early discharge. SEMS have gained international acceptance as an alternative to surgery and are a useful adjunct to management where expertise, operating time, limited hospital beds and other resource limitations exist. This is the first reported series using SEMS for palliation of malignant gastro-duodenal obstruction in Africa.
METHOD: Patients with clinical and endoscopically proven malignant gastro-duodenal obstruction and a relative contraindication to surgical bypass were eligible. A side-viewing duodenoscope combined with fluoroscopic screening was used to place the SEMS under direct vision. Data were collected prospectively until death from November 2004 to November 2007.
RESULTS: 42 patients, median age 64 years (range 39 - 84) had attempted SEMS placement. The obstruction was due to antral gastric adenocarcinoma (n=17), pancreatic adenocarcinoma (n=17), duodenal adenocarcinoma (n=1), cholangiocarcinoma (n=3), gallbladder carcinoma (n=1) and extrinsic compression from metastatic adenocarcinoma (n=3). Relative contraindications to surgery were locally advanced tumour (n=23), metastatic disease (n=12) and co-morbidity (n=7). The site of obstruction was gastric antrum (n=17), D1D2 (n=11), D2D3 (n=13) and D3D4 (n=1). There were four technical failures (9.5%). In the 38 (90.5%) technically successful placements, 36 (94%) patients resumed oral intake (n=4 liquid, n=15 soft diet, n=17 full diet) and two failed (second obstruction distal to gastro-duodenal obstruction). 14 patients required additional biliary stenting. The median time from stent to discharge was two days (range 1 - 8). Median survival following SEMS was 41 days (range 4 - 321) with 10 patients still alive. Two patients were lost to follow-up. One patient (antral gastric carcinoma) required a three unit blood transfusion following stent placement. There were no other immediate complications.
CONCLUSION: SEMS has a high technical success rate (90.5%) and is able to rapidly restore enteral intake in 94% of patients with malignant gastro-duodenal obstruction who are unsuitable for surgery in a resource-limited environment.
Minimally invasive retroperitoneal pancreatic necrosectomy
Omoshoro-Jones AO; Sparaco A; Klipin M; Smith MD
General and Hepatopancreatobiliary Surgery, Division of Surgery, Chris Hani-Baragwanath Hospital, University of the Witwatersrand, Johannesburg
INTRODUCTION: Infected pancreatic necrosis remains a dreaded complication of acute severe pancreatitis. A minimally invasive retroperitoneal surgical approach has proved useful in improving the associated dismal outcome. This report presents an early experience with this procedure in South Africa.
PATIENTS AND METHODS: Between January 2006 and March 2008, consecutive patients with severe acute pancreatitis and infected necrosis were subjected to a minimally invasive retroperitoneal necrosectomy (MIRP) and establishment of continuous lavage of the cavity through the necrosectomy tract. MIRP is performed following initial resuscitation and stabilization of patients in a high care or intensive care environment and within 48 - 72 hours of a radiologically placed percutaneous catheter. Under image guidance, the tract is dilated to a 34 Fr size, over a guidewire, using graduated urology Amplatz dilators. A piecemeal necrosectomy and/or debridement are then performed through a nephroscope. Thereafter, an irrigation system is established with the placement of an irrigating-draining Fuller Sump catheter. The procedure is repeated in line with the patient's clinical and radiological progress. Operative time, related complications, mortality and hospital stay are analysed.
RESULTS: There were 7 patients, 5 males and 2 females, median age 34 (29 - 63) years. All had one or more organ dysfunction/failure at presentation. Median procedures per patient was 3 (2 - 4). Median operation time and blood loss were 2 (1.2 - 2.48) hours and 150 (100 - 350) ml respectively. Of two patients who developed pancreatic fistula, one resolved spontaneously and the other with endoscopic therapy. There was no mortality in this group. Median ICU/HCU and hospital stays were 16 (6 - 29) days and 46 (40 - 80) days respectively.
CONCLUSION: From this initial experience, MIRP is safe and fairly effective in treating infected pancreatic necrosis with minimal or no adverse outcome.
Outcomes of hepatic resection for colorectal metastases
Hewat M; Krige JEJ; Shaw JM; Bornman PC
Department of Surgery, University of Cape Town and Groote Schuur Hospital
AIM: To determine outcomes of hepatic resection of single and multiple colorectal liver metastases (CRLM).
PATIENTS AND METHODS: 107 patients (62 men, 45 women; mean age 58 years, range 18 - 79) underwent liver resection for CRLM between December 1987 and April 2006. Data were collected prospectively and 105 patients were followed up until May 2007.
RESULTS: 50 patients had a single metastasis resected (Group A); 34 had 2 or 3 metastases (Group B) and 23 had 4 or more (range 4 - 9) metastases resected (Group C). Mean operative time was 254 minutes (range 135 - 435) in Group A, 274 min (range 150 - 525) in Group B, and 319 minutes (range 180 - 510) in Group C (p = 0.005). There were no significant differences in inflow occlusion time (p = 0.30), intra-operative blood loss (p = 0.13), blood transfusion (p = 0.20) or hospital stay (p = 0.92). 6 patients died in hospital; 3 in Group A, 2 in Group B, and 1 in Group C (peri-operative mortality 5.6%). 14 patients in Group A had postoperative complications (9 major, 5 minor) as opposed to 12 in Group B (5 major; 7 minor) and 7 in Group C (5 major, 2 minor). Survival did not differ significantly between the three groups (p = 0.66). Actual 3-year survival was 22% in Group A (10 alive out of 46 patients 3 years post surgery), 22% (7/32) in Group B and 14% (3/22) in Group C. 5-year survival was 18% in Group A, 13% in Group B, and 15% in Group C. 10-year survival was 12% in Group A, 14% in Group B, and 8% in Group C.
CONCLUSION: The outcome of liver resection for multiple colorectal metastases is comparable to resection for single lesions.
PEPTIC ULCER DISEASE AND GASTRIC CANCER IN THE BOLAND
Smits CAG; Duvenage R; Lee E; Voss M
Worcester Provincial Hospital, Government of Health of the Western Cape, Worcester
BACKGROUND: Studies from the Northern hemisphere have suggested that demographics of ulcerating lesions in the stomach and duodenum are changing; with gastric cancers showing a proximal migration and a dramatic decrease in the ratio of gastric to duodenal ulcers. Anecdotally, the Western Cape of South Africa is said to be a high-incidence region for peptic ulcer disease and gastric cancer, although in recent years very few studies have been published of the demographics of peptic ulceration and gastric cancer in Southern Africa.
AIMS: To compare the local demographics of peptic ulceration and gastric cancer with published trends.
METHODS: The study took place in a regional hospital in the Boland, a region in the Western Cape, which serves a largely agricultural community of 500 000 people. Epidemiological data were gathered prospectively from patients with an endoscopically significant mucosal break in the stomach or duodenum over a period of 10 months.
RESULTS: 118 peptic ulcerations were diagnosed. Eighty-eight patients (75%) had gastric ulceration, and 27% of these were malignant. Analysis of location of the gastric ulcer showed the commonest sites were: incisura (26 cases, 1 malignant); prepyloric (26 cases, 5 malignant); gastric body (16 cases, 10 malignant); elsewhere in the antrum (11 cases, 5 malignant). Only 6 patients had ulceration at the cardia, of which 3 were malignant. Of patients being followed up for gastric ulcer, 33% defaulted from treatment.
CONCLUSIONS: The ratio of gastric to duodenal ulcerations and proximal to distal cancers in our region differs from contemporary reports from the Northern hemisphere, but resembles distribution reported 40 years ago. Although prepyloric ulcers are said to share the same pathogenesis as duodenal ulcers, they may be malignant and therefore should be biopsied and followed up. Compliance with follow-up was unsatisfactory. An ongoing study will determine whether this is improved by endoscopy outreach.
PREVALENCE OF HELICOBACTER PYLORI VIRULENCE GENOTYPES IN SOUTH AFRICA: A NEW PERSPECTIVE
Fritz E LI; van der Merwe S WI; Steyn CII; Jansen van Rensburg EIII
IDepartment of Immunology, University of Pretoria;
IINETCARE, Pretoria East Hospital;
IIIDepartment of Genetics, University of Pretoria
The human pathogen Helicobacter pylori has been classified as a carcinogen by the International Agency for Research on Cancer (IARC). Infection usually results in chronic gastritis and in some cases atrophic gastritis. Less than 2% of infected individuals may develop gastric cancer. Infection with H. pylori strains that have specific variants of different pathogenic genes is associated with an increased risk of atrophic gastritis and gastric cancer.
In South Africa the reported incidence of gastric cancer in Caucasians is four times higher than in black Africans, even though H. pylori infection is twice as high in black individuals compared to Caucasians. To study the discrepancy between infection and disease in South Africa, gastric biopsies were obtained from 104 individuals (47 Caucasian, 37 black African and 20 Khoisan). Histopathology and H. pylori genotype investigations were conducted.
Overall, 61.5% of biopsies were infected with H. pylori, with 34% of Caucasian, 76% of black African and 100% of Khoisan being infected. Results obtained for the cytotoxin-associated (cagA) gene and the vacuolating cytotoxin (vacA) genes of H. pylori showed a significant association of cagA with atrophic gastritis in all patient groups, as was expected. The occurrence of cagA in the different ethnic groups was also significantly different (p=0.001); Caucasians 44%, black African 64%, and Khoisan 55%. In addition, cagA was strongly (p=0.000) associated with the vacA, m1/s1 and m2/s1 genotypes in all groups. Thus the vacA s1 allele in association with cagA appears to be the significant determinant of pathogenicity. The previously reported rare vacA m1/s2 genotype was detected in one Caucasian and two black Africans, thus confirming its paucity. Phylogenetic analysis of the H. pylori strains in the Khoisan show that the cagA gene is not present in the HpAfrica2 strain.
In this first-ever characterization of H. pylori virulence genes by global strains, the results appear to indicate that the most evolutionarily ancient H. pylori strain (HpAfrica2) is non-virulent.
EXPERIENCE WITH ENDOSCOPIC DRAINAGE OF PANCREATIC PSEUDOCYST IN A SINGLE UNIT
Ferndale L; Anderson F; Thomson SR
Department of General Surgery, Addington Hospital and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
INTRODUCTION: Endoscopic drainage of pseudocysts is feasible and has been found to be comparable to open surgical drainage. We performed an audit of our experience with this technique.
PATIENTS AND METHODS: Patients undergoing pseudocyst drainge in a single unit were reviewed in the period 1999 - 2008. Demographic data were noted, presenting symptoms and mode of cyst drainage, complications following intervention and outcomes. Enteric cyst drainage was performed using ERCP needle knife entry and pigtail stenting without the aid of endosonar.
RESULTS: In the period 1999 - 2008, 40 patients underwent drainage procedures for pancreatic peudocysts. There were 10 female and 30 male patients with an age range of 4 - 68 years. The aetiology of the pseudocysts was acute pancreatitis in 26 patients, chronic pancreatitis in 1 and trauma in 13. Pain was the presenting complaint in 17 patients, gastric outlet obstruction in 4 and obstructive jaundice in 1. The methods of cyst drainage are illustrated in the table. Endoscopic drainage was performed in 37 patients and was successful in 34. In 3 patients this was complicated by perforation, infection and haemorhage. Two (5%) of this group died.

There was no follow-up in 6 patients, and foloow-up ranged from 1 month to 3.5 years in the others.
CONCLUSIONS: Endoscopic cyst drainage is the method of choice in our hands. Introduction of endosonar may limit complications. Follow-up remains inadequate.
Accuracy of mrcp compared to the gold standard ERCP in the diagnosis of bile duct disorders
Botha FJH*; Potgieter PH*; De Vries C*; Loggenberg E*; Hurter D*; Barry R*; Fichardt JB*; Joubert G*
Departments of Radiology*, Surgeryt and Biostatisticsf, Faculty of Health Sciences, University of the Free State, Bloemfontein
AIM: To determine the accuracy of magnetic resonance cholangiopancreotography compared with the gold standard endoscopic retrograde cholangiopancreatography in the diagnosis of bile duct disorders at our institution.
PATIENTS AND METHODS: 52 patients with suspected biliopancreatic pathology were included into this prospective observational study. MRCP was performed within a 24-hour period prior to the ERCP.
RESULTS: MRCP had sensitivity, specificity and positive and negative predictive values of 87%, 80%, 83.3% and 84.2% respectively for choledocholitiasis, which correlates well with results obtained in other parts of the world.
CONCLUSION: At our institution, MRCP has high diagnostic accuracy for bile duct calculi. Owing to a small study population, incomparable results were obtained for other bile pathology.
Impact of the use of band ligation on morbidity and mortality at Maputo Central Hospital, Mozambique
Modcoicar P; Cunha L; Arteaga J
Maputo Central Hospital, Mozambique
OBJECTIVES: To evaluate the outcomes of endoscopic treatment of esophageal varices with band ligations and its impact on morbidity and mortality among patients affected by esophageal varices at Maputo Central Hospital between November 2003 and November 2007.
MATERIAL AND METHODS: During the study period, 235 patients affected by esophageal varices bleeding were consecutively submitted to upper digestive endoscopy and treated with band ligations. Oral propanolol was also given. Socio-demographic, clinical and associated pathology data were gathered from clinical and other hospital files retrospectively.
RESULTS: The mean age of the patients was 39 years (range 6 to 77 years; median age 38 years; standard deviation 14 years). About 55% (128/235) were males. Sixty-six per cent (156/235) of patients were submitted to only one session of band ligation. Only 6% (15/235) experienced re-bleeding during the follow-up period which varied between 1 and 48 months, with loss-of-follow-up of about 6% (13/235). During the study period, the mortality rate due to this nosological entity was 3% (7/235) in the Intensive Care Unit (ICU) in Maputo Central Hospital.
CONCLUSIONS: This study confirms the utility of band ligation in the treatment of variceal esophageal bleeding, translating into prevention of re-bleeding episodes and significant reduction of morbidity and mortality at the ICU in Maputo Central Hospital.
Seroprevalence of hepatitis c in diabetic patients in an urban South African setting
Seabi ME; Song E; Mahomed AD; Barrow PH
Johannesburg Hospital, Gauteng
BACKGROUND AND AIMS: Epidemiological and animal studies(1, 2) have suggested a link between diabetes and hepatitis C.The aim of our study was to compare the prevalence of hepatitis C in type 2 diabetics to the general population and to type 1 diabetics.
METHODS: We recruited 516 patients from the diabetes clinic at Johannesburg Hospital and compared them with a control group of 35 211 blood donors who were race and sex matched.The participants were also matched according to recognised risk factors for acquiring hepatitis C.The test kits used to detect the presence of hepatitis C antibodies were the HCV Rapid test device, which is a rapid chromatographic immunoassay for the qualitative detection of antibody to hepatitis C in whole blood, serum or plasma.
RESULTS: The prevalence of hepatitis C was higher in our diabetic group than in the blood donors (1.54% vs 0.02%; p=0.0001). The prevalence of hepatitis C was also higher in type 2 diabetics than in type 1, but this difference was not statistically significant (7/443 vs 1/73; p>0.05). Previous exposure to risk factors for hepatitis C infection did not appear to be related to HCV positivity.
CONCLUSIONS: There appears to be a higher prevalence of hepatitis C in diabetic patients than in the general population. Whether hepatitis C has a direct aetiopathogenic role in the development of diabetes remains to be proven, but there appears to be a link.
References
1. Viserda Chamoro I et al. Hepatitis C as a risk factor for diabetes mellitus type 2. Rev Clin Esp 2006; 206(4): 167-171. [ Links ]
2. Y Shintani et al. Hepatitis C virus infection and diabetes: Direct involvement of the virus in the development of insulin resistance. Gastroenterology 2004; 126: 840-848. [ Links ]
Sages academic gastrointestinal UNIT SURVEY 2007
Levin DI; Watermeyer G; Thompson SR; Fenton KM
IGastrointestinal Clinic, Groote Schuur Hospital and University of Cape Town
AIM: A qualitative assessment of the state of academic gastroenterology (GI) units in South Africa (SA), with emphasis on human resources, equipment and procedures undertaken.
METHODS: Data was supplied by 8 academic centres under the following categories: staff, equipment, and number of procedures for the financial year 2007. A qualitative analysis of trends was undertaken, comparing data from the years 2003 and 2005. Staffing included consultants, trainees, technologists and nurses. Equipment included type and age of all GI equipment, as well newer modalities such as double balloon and other endoscopy.
RESULTS: Medical units are staffed on average by 2 fulltime consultants. There are currently 6 medical and 6 surgical GI trainees. 2 units do not have a medical GI trainee. Since 2002, 22 trainees have achieved the certificate in medical or surgical GI. 18 (82%) are still practising in SA, 11(61%) in academic positions. There are only 2 fulltime medical technologists and great variation in the nursing complement across units. All units have video gastroscopy (range 3 - 5 years), video colonoscopy (range new to 15 years) and manometric equipment. 2 units have endoscopic ultrasound. In addition 1 of these units has confocal and double balloon endoscopy. There has been an increase in colonoscopic procedures of 6 - 44% in 6 units and 14 - 32% in gastroscopies in 3 units. 2 units do more than 400 ERCPs per year.
CONCLUSION: There has been an improvement in basic endoscopic equipment and retention of 61% of qualified trainees within academic units. There are currently 12 trainees, an improvement from 2004. However, 2 units do not have a medical trainee and most units do not have a medical technologist. There is also an absence of advanced GI technology. The challenge therefore will be to create an environment in which academic staff can be retained and GI skills advanced.
Surveillance colonoscopy improves survival in a cohort of patients carrying a single HMLH1 mutation
Stupart DA; Goldberg PA; Algar UF; *Ramesar RS
Department of Surgery and *Division of Human Genetics, University of Cape Town
AIM: To assess the utility of screening colonoscopy in a cohort of patients carrying a single hMLH1 germline mutation (one of the causative mutations for hereditary non-polyposis colon cancer).
PATIENTS AND METHODS: This is a prospective study of 200 subjects with a germline mutation of the hMLH1 gene who were offered surveillance colonoscopy between 1988 and 2007. 611 members of 30 families with pedigrees that were suspicious for inherited colorectal cancer underwent predictive genetic testing. Of these, 200 asymptomatic members of 17 families were found to carry the exon 13 (C1528T) hMLH1 germline mutation. They were offered surveillance colonoscopy. 145 presented for colonoscopic surveillance, while 45 did not.
RESULTS: After a median follow up of 5 years (range 0 - 18), fewer subjects in the surveillance group developed colorectal cancer (12% vs. 25%; p=0.04). Among those patients who developed colorectal cancer, the surveillance group had earlier stage disease at diagnosis than the non- surveillance group (p=0.002). Fewer subjects in the surveillance group died of colon cancer (3.4% vs. 19%; p=0.04), and fewer died overall (11% vs. 29%; p=0.004).
Using Kaplan-Meyer estimates, the surveillance group had a higher life expectancy than the non-surveillance group (median age at death 78 vs. 61 years; p=0.05).
CONCLUSION: Surveillance colonoscopy improves overall and disease-specific survival in subjects carrying a germline hMLHl mutation.
HIV ENTEROPATHY: SYSTEMATIC EVALUATION OF THE GUT BY DOUBLE BALLOON ENTEROSCOPY AND FLOW CYTOMETRY
Rossouw TI; Cassol EI; Malfeld SI, II; Mahasha PI; Fritz ELI, II; Mwantembe OIII; Nieuwoudt MI, II; Bond RI, II; van der Merwe SWI, II; Cassol SII; Anderson RII
IDepartment of Immunology, Hepatology and GI Research Laboratory
IIDepartment of Gastroenterology
IIIUniversity of Pretoria
Human immunodeficiency virus infection in humans may be associated with protracted diarrhoea and weight loss. This has been termed slim disease. HIV-associated enteropathy defines a specific clinical entity where no secondary cause such as opportunistic infections or drug-induced diarrhoea can be shown. Recent developments in double balloon enteroscopy techniques have allowed endoscopic evaluation of the distal gut.
MATERIALS AND METHODS: Double balloon enteroscopy was performed in 26 treatment naïve HIV patients after informed consent was obtained. Biopsies were taken of the duodenum, jejunum, ileum and R and L colon at baseline. Patients were then placed on HAART therapy and duodenal biopsies were taken at 3 months. At 6 months biopsies were taken of the duodenum and L colon. Patients were followed up monthly at the HIV clinic where serum was taken for viral load and other parameters. The bowel biopsies were processed for the following: T-lymphocyte and macrophage isolation by flow cytometry, histology, electron microscopy, tissue viral load
RESULTS: The mean CD4+ count was 77.65 x 10^6/l at baseline. Double balloon enteroscopy was successful in 26/26 (100%) of the patients. The mean endoscopy time was 154 minutes +/- 36 min. Flow cytometry showed the mean CD4+% from duodenum, jejunum, ileum and R colon to be 3.5, 3.7, 12.5 and 6.9 respectively.
At 3 months and 6 months the peripheral CD4+ count increased to 155.6 x 10^6/l and 240 x 10^6/l. At 3 months and 6 months CD4+ count in the duodenum increased by 5.0% and 4.2% respectively. There was a decrease in naïve CD4+ and CD8+ T-cells and an increase in CD4+ and CD8+ effector cells, central memory and effector memory T-cells in the duodenum at 3 and 6 months.
The mean percentage weight gain after 6 months follow-up was 8.12%.
Clinical improvement correlated strongly with a decrease in CD8+ cells in the duodenum.
CONCLUSIONS: HIV enteropathy is associated with low CD4+ T-cells in all gut compartments.
Peripheral blood CD4+ cells promptly increased on HAART therapy, while the gut CD4+ cell count remained low. Improvement in diarrhoea and weight gain occurred in all patients and correlated with a decrease in CD8+ T-cells.
The gut was repopulated by effector and memory T-cells. The naive T-cell populations remained low.
Clinical, radiological and laboratory predictors of outcome in patients admitted to Groote Schuur Hospital with acute severe ulcerative colitis
George DI; Epstein D*; Stupart DII; Goldberg PAII; Watermeyer GI
IDivision of Gastroenterology of the Departments of Medicine Surgery
IIGroote Schuur Hospital and University of Cape Town
INTRODUCTION: 60% of patients with acute severe ulcerative colitis (ASUC) fail to respond adequately to IVI corticosteroids. It is important to identify non-responders early in order to initiate salvage medical therapies or alternatively offer timely colectomy with counselling/stoma education. Numerous clinical, radiological and laboratory predictors of outcome in ASUC have been described previously and are widely adopted, particularly CRP >45mg/l or stool frequency >8/day on day 3 of IVI steroids. At our institution, however, we manage a unique cohort of UC and it is unclear whether these indices are meaningful in our setting. We therefore sought to determine which factors are of value in our patient population.
METHODS: A retrospective review of all ASUC admitted to Groote Schuur Hospital (2000 - 2007). Cases fulfilling Truelove and Witt's criteria were identified from the UC database, surgical records and inpatient summaries. Data extracted included demographics, details of UC course/management, laboratory indices and radiographic features.
RESULTS: Sixty-six cases were identified. In 49 (74%) it was the first attack. All received IVI hydrocortisone. Fifty five (83%) responded completely and remained colectomy-free at 90 days, while 11 (17%) failed therapy and required colectomy during that admission. No deaths were reported at 3 months. On admission the colectomy group were significantly more likely to have colonic dilatation (p<0.0001) and significantly lower ESR values than steroid-responders (p=0.014). On day 3 the colectomy group were significantly more likely to have a pulse rate above 90 (p=0.0001), serum albumin below 30 (p=0.02) and stool frequency >4/day (p=0.0041). No patients had stool frequency >8/day on day 3. There was no difference in CRP> 25, CRP> 45 or mean CRP levels on day 3.
CONCLUSION: Our results support certain clinical, radiographic and biochemical indices in predicting outcomes in ASUC. On admission the finding of colonic dilatation and on day 3 a low serum albumin, an elevated pulse rate and stool frequency >4/day appear most valuable in our patient population.
RETROSPECTIVE ANALYSIS OF RESECTED PRIMARY COLORECTAL cancer REVEALED NO correlation BETWEEN NODE HARVEST AND NODE INVOLVEMENT
Rathore MAI; Bhatti MII; Hand LI; Allen DII; Ismail MI; Loughlin VI
IDepartment of Surgery, Lagan Valley Hospital, Lisburn, N/Ireland UK
IIDepartment of Pathology, Belfast City Hospital, Belfast, N/Ireland UK
INTRODUCTION: The aim of this study was to analyse lymph nodes harvest (LNH) to lymph nodes involvement (LNI) correlation in resected primary colorectal cancer.
PATIENTS AND METHODS: The study period was Jan 2002 - Dec 2006 inclusive (5 years). The data were obtained from medical records, pathology and radiology. The patient inclusion criteria were resection of primary colorectal cancer (CRC) (curative or palliative intent) including synchronous or metachronous cancer. Exclusion criteria were recurrent CRC, cancer not operated, cancer not resected (stoma-only; open-close) and endomucosal resection. LNH and LNI were obtained. The data were analysed and also compared with the literature and the national audit.
RESULTS: There were 142 resections in 141 patients (mean 28 per annum). The M:F ratio was 0.97:1 and the median age 71 years. There were 86 colonic (60.5%) and 56 (39.5%) rectal cancers. There were 70 (49.3%) anterior resections and 11 APRs (from a total of 83 rectal resections; the remaining 2 were pan-proctocolectomy). Eighty-eight per cent of resections were elective (OR=2.2, p=0.003 compared with the UK national audit). 17.6% had metastasis at presentation. Adenocarcinoma NOS constituted 94% of all histology results. Median node harvest was 12 (mean 13, p=0.08). There was no significant LNH-LNI correlation (r=0.16, p=0.06). Survival figures for stages I - III CRC revealed 3-year disease-free survival of 82% (all-stage=67%).
CONCLUSION: LNI as a function of tumour and host behaviour is of prognostic significance whereas LNH may be a quality assurance (QA) tool to be used to compare inter-institutional Multi Disciplinary Team Meeting (MDTM) standard.
THE RELATIONSHIP BETWEEN HIV STAGE, HAART, nutritional status AND OUTCOME
Loots E; Redman L; Anderson F; Thomson SR
Department of Surgery, Addington Hospital, and Nelson R Mandela School of Medicine, UKZN
INTRODUCTION: The interrelationship between HIV stage, nutritional status, HAART and outcome in a high-prevalence South African cohort is poorly defined. Assessment of this relationship was undertaken.
MATERIALS AND METHODS: An observational cohort study over a 16-month period on ART-naïve patients over 18 years of age was performed. Consenting patients attending the HIV/HAART clinic had a nutritional assessment performed. This consisted of anthropometric assessment, BMI, mid upper arm circumference (MAC), waist/hip girth ratio and a bio-impedance assessment of body composition. All measurements were performed by the principal investigator. Albumin levels, CD4 count and viral load were measured. Follow-up was performed with an interval from 3 months to 1 year. Antiretroviral therapy was started when the CD4 count was <220 cells/mm3.
RESULTS: Of 125 recruited patients 90 were female and 35 male. Median age 35 years (range 20 - 58). 119 were African, 4 were Coloured and 2 were Asian. The mean CD4 count was 205 cells/ mm3 with a median of a 145 cells/mm3. 63% had a CD4 count of less than 220 cells/mm3. The mean albumin level was 32 g/dl. In the group of CD4 < 220 albumin was 30.3 g/dl and the group above 220 was 34.7 g/dl (p=0.01). The mean BMI was 24.9 (range 13.4 - 50.4).
Patients with a CD4 count of <220 cells/mm3 had a mean BMI of 23.4 and those with a CD4 count of >220 cells/mm3 had a mean BMI of 28.2 (p=0.01). Body composition bio-impedance and anthropometric measurements demonstrated similar findings except for lean body mass. Thirty five patients were followed up. Over time the following parameters improved: BMI (p=0.008), CD4 (p=0.051), albumin (p=0.028), waist (p=0.02), hip (p=0.005) and MAC (p=0.008), dry lean mass (p=0.08). Deaths were recorded in 6 patients (4.8%), who had mean BMI, albumin and CD4 of 18 and 25 g/dl and 74 cells/mm3 compared with 24 and 32 g/dl and 212 cells/mm3 for survivors.
CONCLUSION: The CD4 count correlates best with albumin and BMI. HAART produces improvement in overall markers of nutritional status but not lean body mass. Deaths occurred in those both severely malnourished and with profoundly low CD4 counts.
CLOSTRIDIUM DIFFICILE INFECTION AND inflammatory BOWEL disease AT GROOTE SCHUUR HOSPITAL: A RETROSPECTIVE REVIEW (2004 - 2007)
Scholz B; Watermeyer G
Division of Gastroenterology, Department of Medicine, Groote Schuur Hospital and University of Cape Town
INTRODUCTION: C. difficile-associated diarrhoea (CDAD) is a major cause of morbidity and death in hospitalised patients. The incidence of this disorder has increased dramatically in the West over the past decade and the emergence of virulent, highly toxogenic strains, inducing severe disease, have been reported. As in the general population the incidence of C. difficile infection in patients with the inflammatory bowel diseases (IBD), Crohn's disease (CD) and ulcerative colitis (UC) has increased and appears to negatively impact on clinical outcome. In this study we sought to determine the extent and severity of C. difficile infection in IBD patients receiving treatment at Groote Schuur Hospital over the past 4 years.
METHODS: A retrospective cohort study was performed. All patients evaluated for C. difficile toxin between 1 January 2004 and 31 December 2007 were identified from the National Health Laboratory Service database. The following information was subsequently retrieved from patient records: demographics, antibiotic usage, details of hospitalisation, immunosuppression, particulars pertaining to IBD diagnosis and management and outcome of C. difficile infection.
RESULTS: 80 of the 1721 patients tested were found to be positive for C. difficile toxin, 27 were patients with known IBD (16 CD, 11 UC). We noted a steady overall increase in the incidence of CDAD at Groote Schuur Hospital during the study period. In all individuals evaluated, the annual rate of C. difficile positivity increased from 3.5% in 2004 to 6% in 2007. A similar non-significant trend was noted in the IBD cohort and strikingly two thirds of those positive were receiving azathioprine or 6-mercaptopurine at the time.14 of 16 patients with CD had extensive Crohn's colitis documented in the past (only 2 had CD limited to the ileum). No IBD patients with CDAD underwent colectomy during the observational period.
CONCLUSION: Preliminary data show an increase in rates of C. difficile infection at our referral teaching hospital over a 4-year period. A similar trend is noted in our patients with IBD, in particular those with extensive colonic disease. In light of these findings prospective evaluation is necessary to determine the responsible strains, and above all the indiscriminate use of antibiotics in our patients must be avoided.
Poster Presentations (5-minute mini-presentations)
(in alphabetical order according to presenting author)
Changing patterns of incidence, aetiology and mortality from acute pancreatitis at Kalafong Hospital, Pretoria, 1988 - 2007
Chamisa I; Mokoena T; Luvhengo TE
Kalafong Hospital. Department of General Surgery, University of Pretoria
BACKGROUND: Literature reports from Western countries have suggested an increasing incidence of acute pancreatitis (AP) and changing patterns over the past two decades. The aim of this study was to document the incidence, aetiology and mortality from AP in a single instituition over two decades (1988 - 2007) and to examine any emerging trends.
METHODS: A retrospective study of all confirmed cases of AP admitted to the surgical department over a 20-year period was performed. Discharge letters and summaries of all AP patients were retrieved from a computer database. Patient demographics, year of admission, number of attacks, aetiology, management, number of days in hospital, outcome and readmission were entered on a special study proforma.
RESULTS: In all 707 attacks of AP (602 males and 105 females) were recorded. The absolute number of AP admissions between the two decades (n=417, n=290) decreased in proportion to the total number of surgical admissions (34 128 and 26 723), the percentages being 1.2% and 1.1% respectively. There was an increase in gallstone AP (3.1% and 12.8%) attributed to changing demographics but also an absolute increase in blacks. In both decades, alcohol was the main aetiological factor for AP. Drug and endoscope-related AP increased and more whites with AP were admitted in the second decade (n=5, n=57). The in-hospital mortality rate during the respective decades was 6.5% and 3.1%. Mortality for alcohol-induced AP decreased from 6.9% to 2.0% but that for gallstone AP decreased less, from 7.7% to 5.4%.
CONCLUSION: The overall incidence rate for AP decreased proportionately to the total number of surgical admissions over the two decades. Gallstone-related AP increased, and alcohol-related AP decreased. There was a downward trend in mortality from AP, probably attributed to better management.
Keywords: Acute pancreatitis; epidemiology; incidence; mortality.
Early experience with laparoscopic splenectomy for haematological conditions
Ferndale L; Naidoo M; Bhaila SH; Thomson SR; Bassa F
Departments of Surgery1 and Medicine1, IALCH and Nelson R Mandela School of Medicine, UKZN
INTRODUCTION: Laparoscopic splenectomy has become the preferred method for removing the spleen in haematological conditions. We present the early experience from this unit.
PATIENTS: Between January 2007 and March 2008 16 patients underwent splenectomy at the Specialised General Surgery Unit at Inkosi Albert Luthuli Central Hospital. The indications were idiopathic thrombocytopenic purpura (11 patients); Hodgkin's disease (1); auto-immune haemolytic anaemia (1); systemic lupus erythematosus (1) and portal hypertension (1). The average age was 26 years and the female to male ratio was 7:1.
METHOD: Patients were placed in the supine position with a sandbag placed under the left subcostal area. Four ports were used, a 15 ml port supraumbilically; a 10 ml camera port parallel to first port in midclavicular line; a 5 ml epigastric port to left of midline and a 5 ml port in anterior axillary line parallel to supraumbilical port. The spleen is mobilised using an energy device and removed using an endopouch. All spleens were morcelated except where histology was needed.
RESULTS: The rate of conversion to an open procedure was 25%. All conversions were due to bleeding from the hilar region. Two patients required a cholecystectomy in addition to a splenectomy. One patient required a liver and lymph node biopsy in addition to a splenectomy. There were no mortalities and the only serious morbidity was portal vein thrombosis. The average hospital stay was 5 days. The average follow up time was 3.8 months. During follow up, one patient with ITP had a relapse of thrombocytopenia. All other patients were well at follow up.
CONCLUSION: Early experience with laparoscopic splenectomy is safe and encouraging despite a conversion rate of 25% largely for haemorrhage control. These conversions may be part of the learning curve as they occurred early in the experience.
A prospective audit of diagnostic laparoscopy in the diagnosis of abdominal tuberculosis
Islam J; Clarke DL; Ghimenton F; Wilson D; Thomson SR
Departments of Surgery and Internal Medicine, Edendale Hospital and University of Kwa-Zulu Natal
INTRODUCTION: HIV/AIDS has resulted in a resurgence of abdominal tuberculosis in South Africa. Confirming the diagnosis can be difficult. The role of laparoscopy in making the diagnosis is undefined. This prospective audit looks at the role of laparoscopy in establishing the diagnosis of abdominal TB.
METHOD: All patients with clinically suspected but histologically or microbiologically unconfirmed abdominal tuberculosis are jointly assessed by an infectious diseases physician and a general surgeon. If a histological diagnosis of TB cannot be made by any alternative route then the patient will be offered a formal diagnostic laparoscopy under general anaesthetic.
RESULTS: Since January 2008 24 patients with suspected abdominal tuberculosis have been referred for assessment (12 males, 12 females, mean age 34.7 (14 - 73)). Nine patients died before any procedures (2 males and 7 females, mean age 32 (14 - 39)). All 9 of them were HIV positive. Five patients required emergency laparotomy (3 for bowel obstruction and 2 for peritonitis; 4 were males and 1 female, mean age 34.2 (23 - 41); 3 patients were HIV positive and 2 were unknown and refused to test). All 5 of these patients had positive histology for TB. Ten patients went for diagnostic laparoscopy (6 males and 4 females, mean age 37.4 (23 - 73); 2 patients were HIV negative, 2 were unknown and 6 were positive). All patients underwent U/S abdomen and 9 patients had a CT abdomen. One patient was found to have appendicitis. In all others there was macroscopic evidence of chronic inflammation. Only 3 patients had positive histology for TB. Four patients had evidence of chronic inflammation on histology. The histology in the remaining 2 was normal. There were no major complications post procedure. One patient died nine days after the laparoscopy.
CONCLUSION: Laparotomy remains an effective way of definitively diagnosing TB abdomen. Our experience with laparoscopy is small. Laparoscopy is useful to diagnose alternative surgical pathologies that need treatment. Histology confirmed the presence of TB in a third of cases. The presence of chronic inflammation without evidence of TB bacilli is confusing.
OUTCOME IN 39 PATIENTS FOLLOWING PERCUTANEOUS TRANSHEPATIC BILIARY DRAINAGE PERFORMED OVER ONE YEAR AT CH BARAGWANATH HOSPITAL
Klipin MJ; Sparaco A; Omoshoro Jones J; Nagdee IA*; Smith MD
Department of Surgery and Radiology*, Chris Hani Baragwanath Hospital, University of the Witwatersrand, Johannesburg
AIM: To determine outcome in patients following percutaneous transhepatic biliary drainage (PTC) at CH Baragwanath Hospital.
METHODS: Retrospective analysis of prospectively collected data. All patients undergoing PTC at CH Baragwanath from 1 May 2006 to 30 April 2007.
RESULTS: Forty nine patients had a PTC from 1 May 2006 to 30 April 2007. Complete records were available for 39; 27 females and 12 males. Average age 57.6 years (23 - 96). The aetiology of biliary obstruction was malignancy in 22, suspected malignancy in 9, benign in 5 and indeterminate in 4. Ten had a PTC as the first biliary drainage. Twenty nine had prior attempts at endoscopic biliary drainage. Twenty-five patients died before discharge. Of these, 18 had the PTC in situ at time of death. Five had their PTC internalized, 2 endoscopically and 3 percutaneously. One patient's PTC became displaced and one patient had an open bypass. In patients who died the average duration from admission to insertion of PTC was 6 (0 - 27) days. Survival following PTC insertion was on average 13 (0 - 42) days. Average hospital stay was 20 (2 - 49) days. Fourteen patients were discharged, 3 with their PTC in situ. Eight had successful internalisation, 5 endoscopically and 3 percutaneously. Two required open bypass. A single patient with a previous hepaticojejunostomy was deemed to have adequate drainage and the PTC was removed. Duration from admission to PTC insertion was 13 (4 - 27) days. Time from PTC insertion to discharge was 17 (3 - 44) days. Average hospital stay of survivors was 37 (13 - 72) days.
CONCLUSION: Percutaneous biliary drainage has a 65% in hospital mortality. The majority of patients (75%) had failed attempts at endoscopic drainage (29 of 39). Prolonged hospitalisation is common (average 24 days). There is a need to identify factors that predict poor outcome.
ARPI, A NON-INVASIVE MARKER FOR ADVANCED FIBROSIS IN NASH, AND A NEW PROPOSED ALGORITHM FOR THE DETECTION OF ADVANCED FIBROSIS
Kruger FCI, II; Daniels CII; Kidd MIII; Swart GIV, V; Brundyn KIV, V; van Rensburg CI; Kotze MJIV
IDivision of Gastroenterology and Hepatology, Department of Medicine, Faculty of Health Sciences, Stellenbosch University (US)
IIDurbanville Medi-Clinic, Durbanville
IIICentre for Statistical Consultation, US
IVDepartment of Anatomical Pathology, Faculty of Health Sciences, US
VNational Health Laboratory Services, Anatomical Pathology, Tygerberg Hospital, Tygerberg
BACKGROUND: Non-alcoholic steatohepatitis (NASH), the non-benign form of non-alcoholic fatty liver disease (NAFLD), can lead to cirrhosis and even hepatocellular carcinoma. The NASH fibrosis score (NFS) has proven to be a reliable, useful, non-invasive marker for the prediction of advanced fibrosis, but a recent study showed that the addition of the ELF panel improves sensitivity. The aspartate aminotransferase-to-platelet ratio index (APRI) is a simpler calculation than NFS, but has never been studied in patients with NAFLD.
AIM: To validate APRI as a non-invasive marker of liver fibrosis in subjects with NAFLD to be used in clinical practice. Furthermore, the sensitivity and specificity of APRI will be compared to NFS and aspartate aminotransferase-to-alanine aminotransferase ratio (AST/ ALT) in an attempt to develop a reliable, user-friendly algorithm for the prediction of advanced fibrosis and thereby avoiding unnecessary liver biopsies.
SUBJECTS AND METHODS: The cohort consisted of 111 patients with a histological diagnosis of NAFLD. The biopsy samples were staged and graded according to the NASH CRN criteria. These were grouped into fatty liver disease (FLD) and NASH as well as no/mild fibrosis (grade 0, 1, 2) and advanced fibrosis (grade 3 and 4). For each group APRI, NFS, AST/ALT ratio was calculated and compared to ALT.
RESULTS: The APRI was significantly higher in the advanced fibrosis group. The area under the receiver operating characteristic (ROC) curve for APRI was 0.85 with an optimal cut-off of 0.98 giving a sensitivity of 75% and a specificity of 86%. The NFS was significantly lower in the advanced fibrosis group. The ROC for NFS gave an AUC of 0.77 and a cut-off value of -1.3 with a sensitivity of 76% and specificity of 69%. The positive predictive value for APRI was 54% as opposed to 34% for NFS. The negative predictive value was 93% for APRI and 94% for NFS.
CONCLUSION: APRI compared favourably to the NFS and was superior to AST/ALT with regard to reliability for the prediction of advanced fibrosis. It is, however, less expensive and easier to calculate than APRI. We therefore propose the use of APRI in a new algorithm for the detection of advanced fibrosis.

THE SPECTRUM OF ADULT INTUSSUSCEPTION
Naidoo M; Steer D; Clarke DL; Thomson SR
Department of General Surgery, Addington Hospital and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban
INTRODUCTION: Intussusception is uncommon in adults and is usually of a more sinister nature than in the paediatric population. This review looks at the spectrum of presentation and pathology in adult intussusception.
METHODS: We approached both the private and public sectors in both Durban and Pietermaritzburg and requested information regarding any patients they had seen with intussusception. This is both a retrospective (from 2004) and prospective (from 2006) survey.
RESULTS: Twenty-two patients with 23 intussusceptions were identified; 1 patient presented with two sites of intussusception. There were 16 males and 6 females. The average age of presentation was 53. A pre-operative diagnosis was made in 8 of the 22, CT scan diagnosed 6, and the remaining 2 were diagnosed at colonoscopy and ultrasound respectively. The rest were diagnosed intraoperatively. The lead points were adenocarcinoma (4), amoebic colitis (2), gastro-intestinal stromal tumour (2), lymphoma (1), lipoma (1), Peutz Jeghers (1), inflammatory myofibroblastic tumour (1). No lead point could be identified in 2 cases and the lead points in the remaining 6 could not be determined due to necrosis. The anatomical descriptions of the intussusceptions were jejuno-jejunal (3), ileo-ileal (10), and ileocolic (9) and colo-colic (1). Resection was performed in 20, 2 early postoperative intussusceptions with no palpable lead point being reduced intra operatively. The Peutz Jeghers patient had resection of the lead point via an enterotomy.
CONCLUSION: Adult intussusception is rare and is usually secondary to a lead point. One-third present with subacute symptoms and a CT scan is the preferred diagnostic modality. Resectional surgery is the mainstay of treatment.
Outcome analysis of pancreaticoduo-denectomies at Groote Schuur Hospital -an interim analysis
Troskie C; Bornman PC; Essel H; Krige JEJ
Department of Surgery, University of Cape Town and Groote Schuur Hospital
AIM: To review the outcome of non-trauma-related pancreaticoduodenectomies performed at Groote Schuur Hospital between 1980 and 2007, with a sub analysis of survival between 2000 and 2007.
METHODS: Retrospective analysis was performed. The pathology, postoperative complications and mortality were reviewed. A sub-analysis compared the survival and stages of patients between 2000 and 2007.
RESULTS: The male:female ratio was 135:96 with a median age of 57 years. Of the 221 patients, 159 had a pylorus-preserving pancreaticoduodenectomy and 62 a standard Whipple procedure. Pathology (n=223): adenocarcinoma n=62 (28%), ampullary tumour n=70 (31%), chronic pancreatitis n=28 (13%), cholangiocarcinoma n=18 (8%), cystic neoplasm n=14 (6%), duodenal carcinoma n=5 (2%), other n=15 (7%). The in-hospital mortality was 5.5% (n=12).The causes of death were bleeding (n=4), liver necrosis (n=1), multi-organ failure (n=6), and DVT/PE (n=1). The complications were: pancreatic fistula n=31(14%), bile leak n=20 (9%), delayed gastric emptying n=25 (11%), bleeding n=16 (7%). Re-operation was required in 7% for bleeding. Survival of 11% at 5 years were documented.
CONCLUSION: Pancreaticoduodenectomy remains a major physiological insult with significant morbidity and mortality, and an acceptable survival benefit.
Posters
(in alphabetical order according to presenting author)
CT scan in the assessment of acute pancreatitis in a regional hospital setting
Anderson F; Thomson SR
Department of General Surgery, Addington Hospital and Nelson R Mandela School of Medicine, University of Kwa-Zulu Natal, Durban
PATIENTS AND METHODS: All patients with a diagnosis of acute pancreatitis were prospectively evaluated during the period June 2001 to April 2008. CT scan was used to confirm the diagnosis (20), in evaluation of those with predicted severe (50) disease or in patients who developed complications (81).
RESULTS: In the period June 2001 to April 2008, there were 434 admissions of 381 patients with a diagnosis of acute pancreatitis. CT scan was performed in 151 (35%). In 61 (40%), the CT scan was performed for the assessment of predicted severe disease. Pancreatic necrosis was found in 49 (32%). The extent of necrosis was >30% in 20 (13%). Eight (16%) of the patients with pancreatic necrosis died and 2 (2%) of those without necrosis died.
In 57 patients with predicted severe disease, CT scan assessment was not performed due to clinical improvement or critical illness. Seventeen (30%) of these patients died. Ten (16%) of those with documented pancreatic necrosis had aspiration of the necrotic tissue following clinical deterioration. Infection of pancreatitic necrosis was documented in 5 patients (10%). Two were successfully managed non-operatively, 1 by percutaneous drainage and 2 by open debridement and lavage. Three died.
CONCLUSION: A large proportion of our patients with predicted severe disease are not assessed by CT scan. The finding of infected necrosis is uncommon in our setting. The mortalities are associated with documented pancreatic necrosis.
Symptomatic portal biliopathy
Govender K; Newton KA
Department of Gastroenterology, Inkosi Albert Luthuli Hospital
INTRODUCTION: Cavernous transformation of the portal vein (portal cavernoma) is a rare cause of biliary obstruction. 'Portal biliopathy' refers to these biliary abnormalities. The majority of cases of portal biliopathy are asymptomatic, while 5 - 18% of cases are symptomatic.
CASE PRESENTATION: A 23 year old African male, with a background of portal hypertension of unknown aetiology, presented with jaundice and abdominal discomfort for 3 months. Clinical examination revealed jaundice, splenomegaly and no signs of chronic liver disease. Liver function tests confirmed a mildly elevated bilirubin together with raised cannalicular enzymes and normal albumin. Hepatitis B/C and HIV serology were negative. Rectal snip showed no schistosoma ova. Upper endoscopy revealed small oesophageal varices. Ultrasound and CT abdomen showed cavernous transformation of the portal vein, dilated intra-hepatic ducts, normal liver parenchyma and moderate splenomegaly. MRCP and ERCP confirmed dilated intra-hepatic ducts with a smooth stricture of the common bile duct.
DISCUSSION/CONCLUSION: The pathogenesis of biliary obstruction due to portal cavernoma is poorly understood. Direct compression of the common bile duct as well as ischaemic cholangiopathy have been proposed as possible mechanisms. The management strategies for symptomatic portal biliopathy address the relief of biliary obstruction (endoscopic or surgical) and the decompression of the portal cavernoma via shunt surgery. Our patient has been treated with endoscopic stenting of the common bile duct stricture and he is currently awaiting splenorenal shunt surgery.
Portal biliopathy, although infrequent, needs to be considered in the differential diagnosis of jaundice in patients with portal hypertension.
ERCP IN THE EASTERN CAPE - A SINGLE CENTRE STUDY
Atherstone AK; Stephenson K; Hampton MI; Rogers A
Walter Sisulu University
OBJECTIVE AND BACKGROUND: To evaluate the endoscopic retrograde cholangiopancreatography (ERCP) service at Frere Hospital, East London. The centre enjoys a unique position: a single ERCP endoscopist; a patient base from both public and private sectors covering 2 of the 3 regions of the Eastern Cape; approximately 5 million people.
METHOD: A retrospective analysis of consecutive ERCPs over a 3-year period (2004 - 2006). Case demographics, indication for the procedure (symptoms and ultrasound findings), cannulation rate, sphincterotomy use, outcome and complications were noted.
RESULTS: 277 ERCPs were performed in 263 patients over the 36-month period (male:female ratio 1:3; age range 10 - 92, mean 51.6 years). The most common indication for ERCP was obstructive jaundice (42.6%), and 15% of ERCPs were performed after cholecystectomy. Abdominal ultrasound findings were recorded in 79.8% prior to ERCP. 48% of ERCPs were purely diagnostic whereas 40.8% were classified as either therapeutic or 'both'. A papillotomy or sphincterotomy was performed in 70.7% of cases and cannulation successful in 81.2%. Approximately one third of cases were found to have CBD stones or sludge. Either basket or balloon extraction techniques were employed in 108 cases. A diagnosis of malignancy was confirmed in 16.9% of studies and a further 7.9% suggested such a diagnosis. 83.4% of intended actions (e.g. stone extraction/biopsy/stenting) were successful. Complications noted were significant bleeding in 4 patients, perforation in 1 patient, and pancreatitis in 1 patient. There were no procedure-related deaths.
CONCLUSION: This study again highlights the severe resource limitations present in the Eastern Cape Province; a single endoscopist performs all ERCPs for more than three quarters of the population. Despite the significant challenges that exist in this environment, excellent standards of care are being achieved; the rate of successful cannulation and completion of therapeutic intent are comparable to other reported series.
CLINICAL CASE: AN ASSOCIATION BETWEEN AN ULCERATIVE COLITIS AND VITILIGO IN A YOUNG INDIAN ADULT
Modcoicar P; Manuel R; Carrilho C
Maputo Central Hospital, Mozambique
A clinical case is presented of an association of ulcerative colitis and vitiligo in a 25-year-old patient from an Indian ethnic background. The patient had vitiligo since he was 10 years old and had never been seen and/or treated for it before. He was seen at the one of private clinics in Maputo by a gastroenterologist. His main complaint was diarrhoea with mucus and blood, with only small amounts of stools produced during each defecation. At the time he was referred he had had diarrhoea for the past two weeks. He was submitted to a partial colonoscopy where lesions suggestive of ulcerative colitis were seen and subsequently confirmed by histological biopsies. He was started on oral Mesalasine and topical corticotherapy. His clinical presentation showed improvements in three weeks on treatment. The patient was kept on a maintenance treatment and on a follow-up at nine months he presented no clinical or endoscopic signs of ulcerative colitis. Although there are reported cases of an association between ulcerative colitis and vitiligo this is the first case reported in Mozambique and there are very few cases reported in international biomedical literature.
EPIGASTRIC PAIN WITH SMALL GALLSTONES: A DIAGNOSTIC challenge
Mtshali, Z
Medforum Clinic
These young patients (mostly under 40 years) with small multiple gallstones presented with short episodes of recurrent severe epigastric pain (often radiating to the back). There was a delay in the diagnosis of the gallstones, as the patients were treated by their family doctors or out-patients hospital staff empirically as peptic ulcer cases.
PATIENTS AND METHODS: 30 patients with the above symptoms were seen between 2002 and 2007 in a solo private surgical practice. The following features set these patients apart from peptic ulcer, gallstones pancreatitis, obstructive jaundice from gallstones and cholecystites: 1. Pain - severe, short duration, recurrence. 2. Absence of tenderness when pain has subsided. 3. Gastroscopy - all had no duodenal or gastrical ulcer. 4. Serum amylase, urinary amylase and serum lipase were normal, excluding gallstone pancreatitis. 5. Liver function test - alkaline phosphatase and serum bilirubin were normal, excluding onstructive jaundice. 6. Sonar of gall bladder - multiple small stones, normal gallbladder wall and no pericholecystic fluid. Cholecystectomy was done and confirmed the sonographic features.
CONCLUSION: The severe epigastric pain is supposedly caused by small stones transiently impacting in the ampulla of Vater, stimulating spasm in sphincter of Odi. Small stones supposedly cause both gallstones pancreatitis and biliary colic as separate entities. Recognition of this would prevent diagnostic delays.
GLOMUS TUMOUR OF THE STOMACH: ENDOSCOPIC ULTRASOUND FINDINGS OF A SINGLE CASE
Naidoo VG
Department of Gastroenterology, University of KZN
INTRODUCTION: Glomus tumours of the stomach are rare. Endoscopically the appearance is that of a submucosal lesion which has a broad differential diagnosis. Endoscopic ultrasound (EUS) has the ability to determine the layer of origin and sonar character of submucosal lesions. There is a paucity of literature documenting the EUS characteristics of glomus tumours of the stomach.
CASE PRESENTATION: A 45-year-old man presented with a major upper gastro-intestinal bleed. Gastroscopy showed a large antral submucosal mass with overlying clot on the distal aspect. EUS confirmed a hyperechoic mass arising from the muscularis propria. A distal gastrectomy and Billroth 1 anastomosis was performed. The resected specimen consisted of an ulcerated polypoidal tumour measuring 4x3x3 cm. Histology confirmed a glomus tumour. The patient made an uneventful postoperative recovery.
DISCUSSION: Glomus tumours of the stomach have been described as hypoechoic masses arising from the third or fourth layer with internal heterogenous echo mixed with high echoic spots. This description is based on small patient numbers probably due to the rarity of this tumour.
CONCLUSION: The EUS appearance of the glomus tumour in our patient is unusual in that the mass was fairly uniformly hyperechoic. This suggests that the EUS appearance of glomus tumours may be variable.
Procalcitonin as a marker of sepsis at Groote Schuur Hospital
Rogers AD; Miller M; Piercy J; Joubert IA; Michell WL
Surgical Intensive Care Unit, Groote Schuur Hospital, Cape Town
OBJECTIVE AND BACKGROUND: Procalcitonin, a precursor of the hormone calcitonin and a sensitive marker of systemic sepsis, has been the focus of significant attention in the recent critical care literature. This study evaluates the use of procalcitonin measurements in the management of critically ill surgical patients at Groote Schuur Hospital.
METHOD: Recent literature is reviewed describing the benefits of procalcitonin as a biomarker of severe sepsis in a variety of clinical scenarios. A retrospective review of its use at Groote Schuur Hospital during 2007 was performed. Guidelines are proposed to optimise the effective use of this investigation in our setting.
RESULTS: Procalcitonin is in widespread use at Red Cross Children's Hospital (200 per month average), where the assay is performed. Its effective use at Groote Schuur Hospital is hampered by delays in result availability and concerns over its cost. 535 tests were requested during the fifteen months from January 2007 to March 2008 (35 tests per month; mean 3 per patient; range 1 - 13 tests per patient). The vast majority was sent from the surgical ICUs. Experience during this period has demonstrated that procalcitonin is more specific than leukocyte counts in the presence of significant infection and correlates more closely to mortality in ICU. Most promising though has been its role as a tool to evaluate expensive antibiotic choices after initiation of therapy.
CONCLUSION: Procalcitonin has proved to be a useful adjunct to our special investigation armamentarium. This study has identified that, when used in a focused manner, it gives clinicians confidence when implementing targeted therapies for critically ill surgical patients. Despite its expense (R300), its superiority over traditional markers of sepsis is demonstrated by its earlier increase in infection and its response to antibiotic choice. This study motivates for its greater availability in managing septic surgical patients in tertiary centres.
The '3g ghimenton gastropexy' - a case report of a South African approach to gastric volvulus
Rogers A; Atherstone A
Department of Surgery, Frere Hospital, East London
We present a case of a subacute gastric volvulus in the presence of congenital eventration of the left hemidiaphragm. Our patient, who had experienced bouts of severe epigastric pain over the preceding months, underwent open surgery a month following the initial presentation, and a Greys Ghimenton Gastropexy 1 was performed with a good postoperative course. The technique had recently been described in a poster at the 2007 ASSA meeting. Preoperative contrast studies, plain X-rays and endoscopy demonstrated the pathology, and a postoperative contrast study confirmed the success of the technique.
An audit of provincial gastroenterology services in the western cape
Watermeyer G; Van Wyk M; Goldberg PA
Division of Gastroenterology of the Departments of Medicine and Surgery, Groote Schuur Hospital and University of Cape Town
BACKGROUND: While disorders such as gastro-oesophageal reflux disease, gastrointestinal (GI) cancers and inflammatory bowel disease are prevalent amongst all racial groups within the Western Cape, there is little knowledge of local GI service provision. The state of equipment, facilities and staffing is largely unrecorded and to date unknown. The aim of this study was to audit the availability of GI facilities within the provincial sector, which provides care for the majority of people within the Western Cape.
METHOD: All hospitals in the Western Cape providing endoscopy were evaluated by means of a hands-on audit, to identify available organisational infrastructure. Data was collected including staffing, details and utilisation of existing equipment, maintenance and disinfection techniques and delays in service provision.
RESULTS: Over a period of 12 months 17 Western Cape hospitals were visited: 3 tertiary, 5 regional and 9 district level institutions. There are currently 89 gastrointestinal endoscopes in state service; the average age is 6.1 years (range 1 to 23 years). While most institutions utilise video endoscopy, in many instances equipment is towards the end of its economic life. A total of 26 434 endoscopic procedures were performed over a 12 month period. Overall at least 60% of all adult endoscopy was undertaken at tertiary institutions. The mean delay from consultation until gastroscopy or colonoscopy was 9.25 weeks (range 0.5 - 28) and 8 weeks (range 1 - 20) respectively. Only 1 tertiary and 1 regional hospital employed fully trained, registered GI-specialised nurses and the majority of institutions did not conform to internationally accepted standards for the maintenance and disinfection of endoscopic equipment.
CONCLUSION: While endoscopy equipment is widely distributed throughout the province, it is evident from this undertaking that services in the Western Cape fall short of international standards; with delays in endoscopic provision, lack of adequate equipment, inadequate scope maintenance and disinfection and a shortage of trained staff. As such much of the population reliant on state facilities has poor access to gastrointestinal health care. These deficiencies need to be addressed.














