Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.7 Pretoria jul. 2008
ORIGINAL ARTICLES
Cardiac disease in pregnancy: A 4-year audit at Pretoria Academic Hospital
P Soma-PillayI; A P MacdonaldII; T M MathivhaIII; J L BakkerIV; M O MackintoshIV
IMB ChB, Dip (Obstet) (SA), FCOG (SA), MMed (O et G), Cert (Maternal and Fetal Medicine) SA; Department of Obstetrics and Gynaecology, University of Pretoria and Pretoria Academic Hospital
IIMB ChB, MMed (O et G), FCOG (SA), FRCOG (UK); Department of Obstetrics and Gynaecology, University of Pretoria and Pretoria Academic Hospital
IIIMB ChB, DA (SA), FCP (SA); Department of Cardiology, University of Pretoria and Pretoria Academic Hospital
IV(medical student); Vrije Universiteit, Amsterdam, Holland
ABSTRACT
BACKGROUND: Pre-existing medical disease constitutes one of the five major causes of maternal death in South Africa. Increasing numbers of women with heart disease reach adulthood as a result of advances in diagnoses and treatment of heart disease in childhood.
OBJECTIVE: To assess the profile of cardiac disease and the maternal and fetal outcome of pregnant patients at Pretoria Academic Hospital (PAH).
METHODS: A retrospective analysis was carried out on 189 pregnant cardiac patients who delivered at PAH between January 2002 and December 2005.
RESULTS: Nearly 1% of all mothers who delivered at PAH had underlying cardiac disease. Most cardiac lesions were valvular disease secondary to childhood rheumatic heart disease. Pulmonary oedema was associated with the greatest morbidity and mortality. The severe morbidity rate was 11.6% and the case fatality rate 3.3%. The mean gestational age at delivery was 35 weeks; 18 (9.7%) babies were born before 34 weeks.
CONCLUSION: Cardiac disease in pregnancy is associated with high morbidity and mortality rates for mothers and their babies. Multidisciplinary evaluation with discussion of risk factors, appropriate family planning and optimising of the cardiac state before conception is advised.
Pre-existing medical disease constitutes one of the five major causes of maternal death in South Africa. Cardiac disease contributed to 40.2% of deaths in this sub-group of patients.1
Increasing numbers of women with acquired and congenital heart disease reach adulthood as a result of advances in diagnosis and treatment of heart disease in childhood and adolescence. The high maternal morbidity and mortality is due to compromised cardiac function and inability to cope with the physiological adaptations of pregnancy, stress of labour and haemodynamic changes of the puerperium. Eighty per cent of cardiac disease in pregnancy in the developed world is congenital in origin.2
Objectives
The objectives of the study were to assess the profile of cardiac disease and the maternal and fetal outcomes of pregnant patients at Pretoria Academic Hospital (PAH), and to identify risk categories and thus improve quality of care.
Patients and methods
PAH is a tertiary referral hospital; pregnant cardiac patients are managed by a high-risk firm. In most cases, the diagnosis of cardiac lesions is made clinically and confirmed by echocardiography. Patients are seen at least twice during their pregnancy at a combined clinic by a cardiologist and an obstetrician - early in pregnancy or soon after booking to confirm the diagnosis and decide on the management plan and, in the third trimester, to discuss a delivery plan. Patients undergoing elective caesarean sections are examined by an anaesthetist before surgery. Most patients are referred to the cardiac-obstetric clinic from local clinics or regional hospitals in the city, and some are referred from the private sector and surrounding provinces.
All patients with cardiac disease (excluding hypertensive cardiac disease) who delivered at PAH from January 2002 to December 2005 were included in our study. A retrospective analysis from the maternity register was conducted, using information from patient records. This study is subject to referral bias because of having been conducted in a tertiary institution.
Results
There were 22 681 deliveries at PAH during the study period. Of these patients, 214 (0.94%) had underlying cardiac disease, and data were available for 189 of them. Twenty-five obstetric records were lost. However, we know that these patients were not classified as a 'near miss' or 'maternal death' as these data are kept separately. Severe morbidity rates and case fatality rates were therefore calculated using 214 as a denominator (the total number of cardiac deliveries), but other data presented were based on 189 as the denominator.
Patients referred from surrounding hospitals or clinics comprised 53%, while 47% were either self-referred or known to the unit. Of the referred patients, 63% were from primary or secondary level hospitals, 6% from local clinics, and the rest from the private sector. The majority of patients were from Gauteng (67.4%) and Mpumalanga (26.2%).
Baseline characteristics
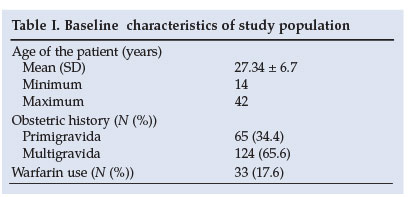
The baseline characteristics of the study population are shown in Table I.
Pathology
The distribution of cardiac lesions is shown in Table II. Organic valve lesions complicated 63.5% of pregnancies, and prosthetic valves were seen in 20.1%. Organic lesions combined with prosthetic valves were seen in 7.9%, and congenital heart disease occurred in 9.0% of pregnancies.
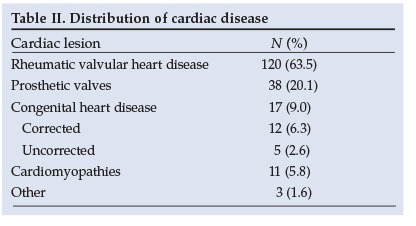
In patients with valve lesions, organic mitral regurgitation and mitral stenosis represented the most common pathologies - 27.5% and 20.8%, respectively. In patients with prosthetic valves, mechanical replacement of the mitral valve was most commonly observed (55.3%). Atrial septal defect and ventricular septal defects were the most common congenital lesions seen.
Maternal outcome
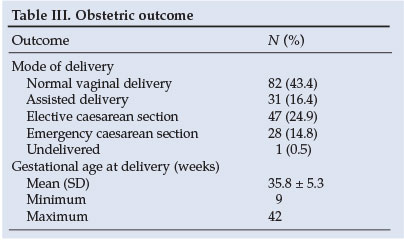
Table III summarises the obstetric outcomes. There were 113 vaginal deliveries, of which 31 (27%) were assisted. We prefer reducing the length of the second stage by an assisted delivery to limit the strain on the heart. The undelivered patient refers to a mother who died prior to delivery.
Near misses
We used the near-miss system as a marker of morbidity in our patients. A near miss describes a patient with an acute organ system dysfunction which could result in death if not treated appropriately3 and has been shown to be a surrogate for maternal death. It occurs about 8 times more often than a maternal death and therefore provides more information on the disease profile of a population.4
There were 48 near misses. In analysing the data, we excluded patients admitted routinely to the intensive care unit for observation following delivery Therefore, there were 25 patients with an organ system dysfunction that resulted in a severe morbidity rate of 11.6%. The average age of patients classified as near misses was 28, and the average parity was 2.
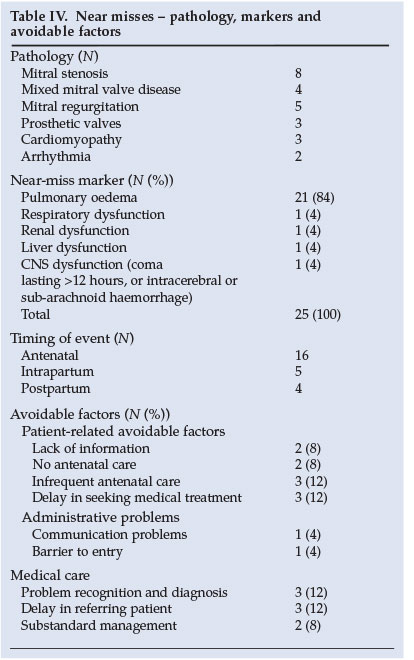
The pathology, near-miss markers and avoidable factors for the patients classified as near misses are shown in Table IV. The avoidable factor analyses were the same as those used in the Confidential Enquiry into Maternal Deaths in South Africa (CEMD).1
Maternal deaths
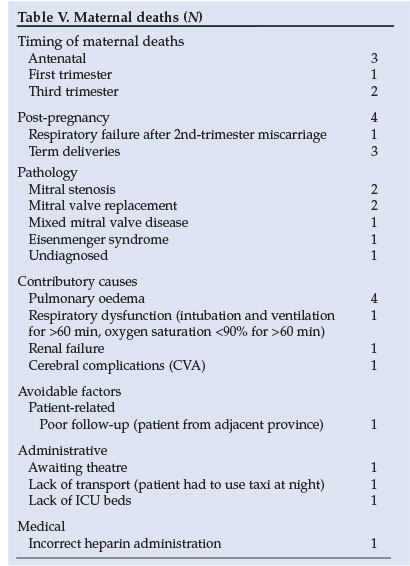
There were 7 maternal deaths among the 214 pregnant cardiac patients. The mortality index, which is described as the subset case fatality rate of critically ill women, was 21%. The case fatality rate was 3.3%. Most of the deaths occurred in the third trimester and the postpartum period. The majority of deaths occurred in women with mitral valve disease; in 57% of cases, the mechanism of death was pulmonary oedema. The pathology, causes of death and avoidable factors are shown in Table V.
Neonatal outcome
The mean gestational age at delivery was 35 weeks, and the average birth weight was 2 500 g. There were 167 (88.4%) babies born alive, of whom 18 (9.7%) were delivered before 34 weeks and 10 (5.3%) were admitted to the neonatal intensive care unit. There were 22 pregnancy loses (11.6%). A possible association between warfarin and pregnancy loss was noted. Of patients not using warfarin, 95% gave birth to a live baby, compared with only 60% of patients who used warfarin.
Discussion
Almost 1% of all patients delivered at PAH presented with underlying cardiac disease. Our patient profile resembles that of a developing country with the predominant lesions being valvular lesions secondary to childhood rheumatic heart disease. Organic mitral regurgitation was the most common pathology, while stenosis of the mitral valve was associated with the greatest morbidity and mortality.
Rheumatic fever is uncommon in developed countries, which since the 1980s have had a prevalence of under 0.5/100 000 children of schoolgoing age. In contrast, the annual incidence in developing countries is 100 - 200 times greater.5 African studies have shown a prevalence of 2.7/1 000 schoolgoing children in Nairobi and 14.3/1 000 children in Kinshasa.6 In Soweto in 1975, a prevalence of 6.9/1 000 was found, with a maximum of 20/1 000 in 7th and 8th grade children - the highest reported prevalence of the disease at the time.7 The investigators of this study concluded that '... a comprehensive prevention campaign is urgently needed'.
Although the Department of Health reported a decline in the incidence of rheumatic heart disease from the years 2000 to 2004 in South Africa, there is evidence of gross underreporting of the disease.8,9 Rheumatic heart disease is the major cause of cardiovascular disease in children, and this study confirms that this burden of disease continues in adulthood.10
Pulmonary oedema was the greatest cause of morbidity and mortality in this study (associated with 4 (57%) maternal deaths and 21 (84%) near misses). Patients presented with pulmonary oedema in both the antepartum and postpartum periods. It is therefore crucial that underlying cardiac disease is timeously diagnosed so that physicians are able to prevent decompensation during pregnancy and intensively treat those who decompensate. Intensive care access, especially in the postpartum period, should be facilitated to ensure stricter control of fluid balance in cardiac patients after delivery.
Near-miss data show that there were patient-related avoidable factors (CEMD criteria) in 32% of cases - patients were unbooked, booked late or did not have regular antenatal visits. There needs to be greater awareness and education among our communities regarding rheumatic heart disease and its complications. Patients with valvular disease need to be diagnosed early, and ideally they should conclude having children before becoming symptomatic. Unfortunately, the majority of our patients with prosthetic valves had their surgery before or during their reproductive period, and a large proportion of them present to us in pregnancy. Women who are contemplating pregnancy should be educated about their disease and the potential morbidity and mortality that pregnancy holds.
Medically related avoidable factors were present in 32% of the near misses. A maternal death occurred as a result of poor medical care. The patient had a prosthetic valve, was erroneously given an increased amount of heparin, and subsequently died from a cerebrovascular bleed. Our protocol used for heparin administration is a partial thromboplastin time (PTT) value of 2.5 times the normal level. Specialised training is required for medical personnel so that pregnant cardiac patients are effectively managed.
Important administrative factors such as delayed referrals and difficult access to the intensive care unit were identified and will be addressed to prevent further morbidity and mortality.
An association between warfarin use and fetal loss was noted. Unfortunately, postmortems or detailed examinations of these fetuses were not performed. Three of these fetuses had abnormal brain findings on antenatal ultrasound, and the maternal International Normalised Ratio (INR) was uncontrolled in each case. Frequently, patients with prosthetic valves present for antenatal care when pregnancy is advanced and the fetus has already been exposed to warfarin in the first trimester. Pre-pregnancy counselling is of great importance in reducing maternal and fetal risk.
This study had a number of limitations as it was retrospective and patients were identified from the birth register. It is possible that some cases were missed; more accurate data will be obtained from a prospective study currently under way.
Conclusion
Cardiac disease in pregnancy is associated with high morbidity and mortality rates for mothers and their babies. Close haemodynamic monitoring during labour, delivery and the early postpartum period is crucial in patients with cardiac disease. Pulmonary oedema is the most important mechanism of maternal morbidity and mortality. This information should be part of pre-pregnancy counselling. Contraception should be discussed with all patients, and pregnancy should only be contemplated after the maternal condition is optimised. The association between warfarin use and adverse pregnancy outcome confirms other reports.11,12
References
1. NCCEMD, Maternal, Child and Women's Health Directorate. Saving Mothers: Third Report on Confidential Enquiries into Maternal Deaths in South Africa. 2002-2004. Pretoria: Department of Health, 2006. [ Links ]
2. Gelson E, Johnson M, Gatzoulis M. Review: Cardiac disease in pregnancy. Part 1: Congenital heart disease. Obstet Gynecol 2007; 9: 15-20. [ Links ]
3. Mantel GD, Buchmann EJ, Rees H, Pattinson RC. Severe acute maternal morbidity: a pilot study of a definition for a near miss. Br J Obstet Gynaecol 1998; 105: 985-990. [ Links ]
4. Pattinson RC, Macdonald AP, Backer F, Kleynhans M. Effect of audit on critically ill pregnant women. Clin Govern Int J 2006; 11: 278-288. [ Links ]
5. Olivier C. Rheumatic fever - is it still a problem? J Antimicrob Chemother 2000; 45: 13-21. [ Links ]
6. Rheumatic Fever and Rheumatic Heart Disease: Report of a WHO Expert Consultation, 29 October - 1 November 2001. World Health Organ Tech Rep Ser 2001; No. 923. [ Links ]
7. McLaren MJ, Hawkins DM, Koornhof HJ, et al. Epidemiology of rheumatic heart disease in black school children of Soweto, Johannesburg. BMJ 1975; 3: 474-478. [ Links ]
8. Statistical Notes, February 2005. Rheumatic Fever. Pretoria: Department of Health, 2005. http://www.doh.gov.za/facts/stat-notes-f.html (accessed 15 June 2007). [ Links ]
9. Nkgudi B, Robertson KA, Volmink J, Mayosi BM. Notification of rheumatic fever in South Africa - evidence for underreporting by health care professionals and administrators. S Afr Med J 2005; 95: 206-208. [ Links ]
10. Mayosi B, Robertson K, Volmink J, et al. The Drakensburg Declaration on the control of rheumatic fever and rheumatic heart disease in Africa. S Afr Med J 2006; 96: 246. [ Links ]
11. Hanania G. Management of anti-coagulation during pregnancy. Heart 2001; 86: 125-126. [ Links ]
12. Van Mook, Walther NKA, Peeters L. Severe cardiac disease in pregnancy, part II: impact of congenital and acquired cardiac diseases during pregnancy. Curr Opin Crit Care 2005; 11(5): 435-448. [ Links ]
 Correspondence:
Correspondence:
P Soma-Pillay
(priya.somapillay@up.ac.za)
Accepted 8 November 2007














