Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.6 Pretoria jun. 2008
ORIGINAL ARTICLES
The evolving impact of HIV/AIDS on outpatient health services in KwaZulu-Natal, South Africa
Anokhi ParikhI; Nina VeenstraII
IMSc. Health Economics and HIV/AIDS Research Division, University of KwaZulu-Natal, Durban
IIMPH. Health Economics and HIV/AIDS Research Division, University of KwaZulu-Natal, Durban
ABSTRACT
BACKGROUND AND OBJECTIVE: The high HIV prevalence in KwaZulu-Natal (KZN) places immense pressure on the health system. The burden of HIV/AIDS on health services is evolving as the epidemic progresses and as antiretroviral treatment becomes more widely available. For health policy makers and managers, timely and appropriate information is needed to facilitate adaptive management of health services. Through longitudinal research covering outpatient health services in KZN we examined the dynamics of the evolving HIV/AIDS burden and the resource implications of this burden, necessary for resource allocation decisions.
METHODS: Data were collected between 2004 and 2005 in outpatient services across six health facilities in the province. The burden of HIV/AIDS was measured by assessing the proportion of outpatients presenting as HIV positive, determined by a clinical diagnosis (and test result where available). The burden was also measured by looking at the types of diseases presenting at outpatient facilities. Moreover, the study assessed the burden experienced by health care workers and financial implications for health facilities.
RESULTS AND CONCLUSIONS: The study demonstrates that the burden on outpatient services is significant but has not been increasing over time, suggesting that people are not accessing care if and when they need it. However, in terms of resources, this burden has been increasing and shifting from tertiary services to more primary services. In order to accommodate the demands of HIV/AIDS, our focus therefore needs to turn towards outpatient services, in particular at the primary care level.
At 39.1% KwaZulu-Natal (KZN) has the highest antenatal clinic prevalence of any South African province,1 which has enormous implications in terms of a high burden for health services. We should be prepared for increases in the demand for health care for a decade or more even once HIV prevalence rates decline, since many people are in the earlier stages of infection and asymptomatic.
Several studies have looked at the burden of HIV on health services all over sub-Saharan Africa2-5 and have elicited one particularly startling insight: a steep rise in the HIV/AIDS burden on health care facilities in the late 1980s, with apparent stabilisation of burden in later years. This finding contrasts with epidemiological trends, which predict that the burden should have increased markedly owing to the time lag between HIV infection and the stage at which opportunistic infections are experienced.6 Some of this burden on inpatient services will be alleviated as antiretroviral therapy (ART) coverage improves. These papers have focused almost entirely on inpatient services and tertiary hospitals, with little data available on district health services or outpatient services. Only two studies looked at outpatient services. An HIV prevalence of 25.7% was found among patients visiting primary health care (PHC) facilities across four South African provinces.7 Patients attending two PHC clinics in Gauteng were all tested and the HIV prevalences found to be 34% and 36%.8 Although illuminating, data from one point in time do not capture the dynamics of the burden and do not assess how the prevalence translates to a resource burden, which is crucial for planning.
We set out to investigate how the burden of HIV/AIDS on outpatient health services is changing over time using data from KZN. We attempted to capture the pressures that HIV is placing on the health services by assessing the proportion of patients accessing HIV-related care and the consequent resource implications. Understanding this is essential for the system to plan and respond appropriately to changes. Although the fieldwork was undertaken as the ART programme commenced in many health facilities, there were signs of trends that might be experienced as it expands.
Methodology
Sampling
This study was conducted in Ugu district of KZN, from which sample facilities were selected and a referral pattern was tracked. The district was chosen because it has a regional hospital, which ensures urban and rural representation, avoids problems of a dispersed referral system and has an ARV rollout site. This ensured that the district was representative of health districts in the province in terms of its disease profile and complement of health facilities, and also that it has similar demographic and economic profiles to those of the province as a whole.
Three phases of data collection occurred at 6-month intervals and spanned an 18-month period between July 2004 and December 2005. Six facilities participated in all three phases of the study - 1 regional hospital, 1 district hospital, and 4 PHC clinics - allowing analyses of trends in these facilities. Data were collected at inpatient and outpatient facilities to capture the interaction of various levels of care, though this paper focuses on the latter.
Sampling of health facilities for data collection was done by identifying the most representative district, regional and tertiary level hospitals. Clinics were stratified according to their supervising hospital and then randomly sampled, to include 2 clinics under the regional hospital and 2 clinics under the district hospital.
For each phase of the research, the research team visited each facility in the sample for a 2-day period. Since general outpatient services in South Africa function with no special clinics on specific days, it made little difference which days the team chose to visit. Out of consideration for the over-worked health workers, Mondays and other days when facilities were short-staffed or undergoing any change were avoided.
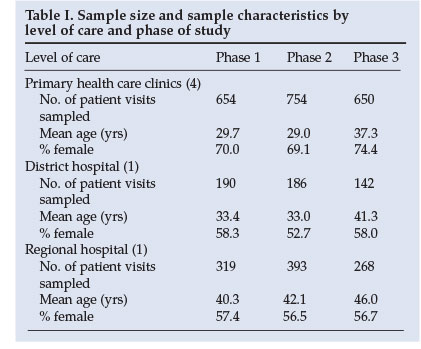
Fieldworkers stationed at key points in the facility (e.g. outpatient clinic, casualty, tuberculosis drop-in centres, medical and paediatric wards) obtained information on each patient passing through the facility. Information collected included demographic details, medical diagnosis, HIV status (according to clinical diagnosis, WHO staging, and HIV test where available), history of treatment and investigations, outcome of illness episode and movement through the health system (Table I).
Measuring burden
The burden of HIV/AIDS was measured by assessing the proportion of outpatients presenting as HIV positive as determined by clinical diagnosis and reference to laboratory tests. The rationale for not attempting to test all patients was because South Africa has reached a stage in the HIV/AIDS epidemic where high prevalence rates are being recorded and HIV testing is conducted for most patients who, from clinical signs and symptoms, are thought to be infected. Testing all patients attending health care facilities for HIV infection has a high risk of overestimating the burden of care, since people may be HIV positive but may not be accessing HIV-related care. It is more reliable to use existing HIV test results supplemented by a clinical diagnosis, because of improving coverage of voluntary counselling and testing (VCT). More than half of patients thought to be HIV positive on clinical signs and symptoms had been confirmed as positive with a test. In contrast, among patients not clinically infected, less than 1% disclosed having been tested to the clinician managing their illness.
To analyse the types of diseases presenting at outpatient facilities, the primary or first recorded diagnosis was considered. Grouping of diagnoses follows that used in Burden of Disease studies, based on the International Classification of Diseases No. 10.9 Patients presenting with an opportunistic infection and HIV positive according to clinical and/or laboratory diagnosis were allocated to the category of 'HIV/ AIDS'.
The concept of the 'burden' of HIV/AIDS becomes more meaningful when considering its resource implications. The study looked at the burden experienced by health care workers and financial implications for health facilities. Focus groups/ interviews with medical staff were conducted to explore how health care workers have adapted and are adapting to changing conditions. Owing to the limited availability of health care workers, inclusion criteria for focus groups and interviews rested largely on individuals' willingness to participate and their time available. These interviews were essential as it cannot be assumed that the proportion of patients seeking care for HIV-related illnesses reflects the workload created by these patients, since HIV-related illness is complicated to manage. Secondly, pressures on health care workers depend on a whole host of factors, many not related to HIV/AIDS.
The analysis of financial resource utilisation was based on assessed HIV prevalence. A limited number of cost categories were examined: personnel costs (in terms of consultation time), drug costs, laboratory costs, and radiological investigation costs. Costing data were obtained through the Provincial Laboratory Services (laboratory investigations), Provincial Medical Supplies (drug costs), and the Kind Edward Radiology Department (radiological investigations).10
The Medical Research Ethics Committee, University of KwaZulu-Natal, gave ethical clearance for this study.
Results and discussion
HIV prevalence in outpatient health facilities based on clinical and laboratory diagnosis
The proportion of patients recorded as HIV positive for each level of care over time indicates that: there is a high proportion of patients recorded as HIV positive for each level of care; the proportion of HIV-positive patients has not increased over time as expected, and the prevalence is the highest in the regional hospital and lowest in PHC clinics (Table II).
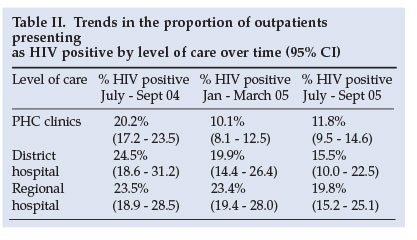
The proportion of outpatients presenting as HIV positive in 2004 is comparable to another study which found the prevalence in PHC clinics in South Africa to be 25.7% in 2002.7 Similarly, inpatient prevalence in this study ranged from 46.9% to 54.5% in 2004 and is consistent with the 46.2% prevalence recorded by Shisana et al.7
While the prevalence of HIV infection in all health care facilities was high, it did not increase during the duration of the research. In inpatient services (data not shown) the percentage was stable over time in both district and regional hospitals. In outpatient services it even appeared to decline, but this decline was not always statistically significant. Ninety-five per cent confidence intervals (CIs) for data obtained at the hospitals (both district and regional) exhibited some degree of overlap over the three phases of the research. Only at the clinic level did the proportion of outpatients presenting as HIV positive register a statistically significant decline between late 2004 and early 2005. This is probably attributable to two contextual factors. During the first round of fieldwork we noted a large number of patients requesting disability grants for their HIV status. Rumour had spread that a positive test result was all that was needed to access this grant, and such misconceptions were only cleared later. Secondly, ART was implemented in two hospitals in the region at this time and it is unclear to what extent this encouraged people to be tested and further managed.
Significant variations between levels of care, with the prevalence rate being lowest among PHC clinics, is not a surprising result as patients with higher levels of morbidity tend to access hospital level care.
Proportion of patients presenting with HIV using the burden of disease methodology
Analysis of different diseases for which patients accessed outpatient services shows that HIV places a moderate burden on outpatient services, with 8 - 22% of patients accessing HIV-related care. Although the types of patients seen at different visits varied, there was no appreciable increase in the burden of HIV/AIDS across all levels of care. There was a statistically significant decline of burden observed in PHC clinics between the end of 2004 and early 2005, which are consistent with the findings in Table II (Fig. 1).
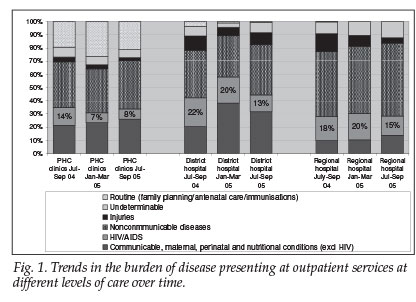
The proportion of patients presenting with HIV was generally higher at the hospitals than at the clinics, but was lower than in previous studies7,8 and indeed lower than the burden measured by prevalence in Table II, something that would be expected in a high-prevalence context. The lack of increase over time concur with suspicions of a rising burden of AIDS illness in communities, a finding documented from Kenya, Lesotho and Swaziland.3,11-12
Resource implications of the HIV/AIDS burden
Our assessment of the resource implications of the burden of HIV/AIDS was based on assessed HIV prevalence. Costing data indicated that while care for HIV/AIDS patients was frequently more expensive than care for other types of patients, this was not always the case. Inpatient care in particular had a tendency to be equally resource-intensive for both types of patients, the exception being at lower-level hospitals. Outpatient care, on the other hand, was nearly always more expensive if it was HIV-related (Fig. 2). This trend is readily explained since HIV/AIDS generally manifests itself in more complex ways than other health conditions managed by lower-level hospitals and outpatient care services.
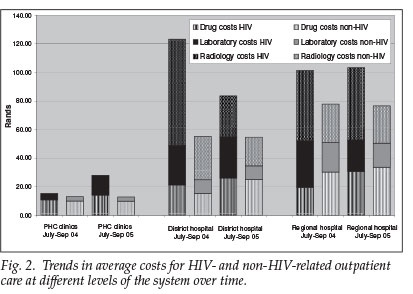
Costing at outpatient facilities identified expected early trends as the ART programme expands, including a shift in the burden from tertiary care to more primary care (Fig. 2). In the first phase, costs of treating HIV /AIDS patients were similar to the costs of treating other types of patients at PHC clinics but were higher in hospitals. Over time, the costs of treating HIV patients increased across all cost categories while the cost of treating non-HIV patients remained unchanged. The high radiology costs at district hospital in the first phase are due to a handful of expensive investigations for a small number of patients.
The services offered at clinics had expanded during this time to offer CD4 testing, pretreatment counselling and dry blood spot polymerase chain reaction (PCR) for infants on the prevention of mother-to-child transmission (PMTCT) programme. This expansion in services resulted in corresponding increases in laboratory costs and human resource implications. Consultation times for HIV/AIDS care became significantly longer, placing more pressure on the clinic sisters (Table III). Meanwhile, consultation times at hospitals became more comparable for HIV/AIDS care and other types of care. The trend of an increasing burden on clinics is likely to continue as HIV/AIDS care becomes more integrated and new interventions are decentralised to lower levels of the system. Other anticipated shifts in the burden of care, such as that from inpatient care to outpatient care, were not evident at this stage.
Making sense of the costing results from this research and those of previous studies has not always been straightforward, simply because the costs of treatment vary according to a whole host of factors, which differ between individual health facilities and levels of care. Importantly, these factors are not only determinants for costs, but also for human resource and infrastructure requirements more generally. According to the findings of this research, they include availability of inputs to care, rationing by health care providers, rationing by users (with suspicions that the more ill individuals were the ones not managing to seek care), clinical staging and nature of treatment (i.e. prophylactic or curative), and level of care.

Conclusion and policy implications
This research demonstrated that the burden on outpatient services in the district was not increasing over time as one would expect, although the resource burden did increase.
As these results come from one district in KZN they may not be generalisable to the whole province or country. Nonetheless, a number of policy-relevant lessons can be learned. First, while the burden has not been increasing, it is still high, in that a large number of patients are seeking HIV-related care. This burden is higher if the resource implications are considered, because HIV patients cost more than non-HIV patients in terms of financial and human resources. In strengthening the health system, outpatient services must therefore not be neglected.
Second, the trends that are being observed are not due to ART as the roll-out had not quite taken off during the study period, the regional hospital having started in August 2004 and having only 112 patients by end of 2005. The district hospital commenced its roll-out in June 2005. Moreover, seeing that South Africa is trying to decentralise the ART roll-out by getting PHC clinics to administer treatment, ART should theoretically decrease the burden on inpatient services and will increase the burden on outpatient services. Again, outpatient services will need to be strengthened.
Third, utilisation of services does not reflect the demand for services, owing to barriers to access. While in accordance with epidemiological trends we expected a greater number of patients to access HIV-related care, utilisation patterns look fairly stable over time. This indicates that people are either facing barriers to accessing care or choosing to not access it. Either way, it implies a high community burden of care. Potential reasons for this situation came out during interviews and have been noted in previous studies, such as costs, stigma and health worker behaviour3 (and A Padarath et al., presented at the 3rd Public Health Conference 2006, Midrand, 15 - 17 May, unpublished). Currently these barriers have implications for ART coverage, since people are required to travel to a health facility frequently to collect their medication.
Finally, there is a real need for information that can enhance adaptive management. Managing resources has become particularly difficult in the context of HIV/AIDS and is often done based on little information. This study looked at the resource implications of managing HIV/AIDS in health facilities and was able to identify some early trends, in particular a shift in the burden from tertiary to primary services. As the ART programme grows we would expect to see further shifts from inpatient services to outpatient services, but this was not yet evident. These shifts require corresponding changes in resource allocation; however, this imperative will never become apparent through isolated studies of only one health facility, which has been the norm until now.
References
1. SA Department of Health. National HIV and Syphilis Prevalence Survey South Africa 2005. Pretoria: South African Department of Health, 2006. [ Links ]
2. Hassig S, Perriens J, Baende E, et al. An analysis of the economic impact of HIV infection among patients at Mama Yemo Hospital, Kinshasa, Zaire. AIDS 1990; 4(9): 883-887. [ Links ]
3. Arthur G, Bhatt S, Muhindi D, Achiya G, Kariuki S, Gilks C. The changing impact of HIV/ AIDS on Kenyatta National Hospital, Nairobi from 1988/89 through 1992 to 1997. AIDS 2000; 14(11): 1625-1631. [ Links ]
4. Gilks C, Floyd K, Otieno L, Adam A, Bhatt S, Warrel D. Some effects of the rising case load of adult HIV-related disease on a hospital in Nairobi. J Acquir Immune Defic Syndr Hum Retrovirol 1998; 18(3): 234-240. [ Links ]
5. Tembo G, Friesan H, Asiimwe-Okiror G, et al. Bed occupancy due to HIV/AIDS in an urban hospital medical ward in Uganda. AIDS 1994; 8(8): 1169-1171. [ Links ]
6. Dorrington R, Bradshaw D, Johnson L, Budlender D. The Demographic Impact of HIV/AIDS in South Africa: National Indicators for 2004. Cape Town: Centre for Acturarial Research and South African Medical Research Council, 2004. [ Links ]
7. Shisana O, Hall E, Maluleke K, et al The impact of HIV/AIDS on the health sector: National survey of health personnel, ambulatory and hosptalised patients and health facilities, 2002. Report prepared for South African Department of Health. Pretoria: Human Sciences Research Council Press, 2003. http://www.hsrcpress.ac.za/product.php?productid=1986 (accessed June 2007). [ Links ]
8. Schneider H, Kellerman R, Oyedele S, Dlamini N. HIV Impact Surveillance System Summary Report: Design and Data Collection. Johannesburg: Wits School of Public Health and Gauteng Department of Health, September 2005. [ Links ]
9. Murray J, Lopez A, Mathers C, Stein C. The Global Burden of Disease 2000 Project: Aims, Methods and Data Sources. Boston: Harvard Burden of Disease Unit, November 2001. [ Links ]
10. Veenstra N, Oyier A. The burden of HIV-related illness on outpatient health services in KwaZulu Natal, South Africa. AIDS Care 2006; 18(3): 262-268. [ Links ]
11. Health and Development Africa (HDA). Study oof the Health Service Burden of HIV and AIDS and Impact of HIV and AIDS on the Health Sector in Swaziland. Johannesburg: Health and Development Africa (Pty) Ltd/JTK Associates, 2005. [ Links ]
12. Mburu F, Naidoo S. Impact of HIV/AIDS on mortality among the inpatients at Motebang Hospital, Lesotho. Southern African Journal of HIV Medicine 2004; 16: 33-37. [ Links ]
 Correspondence:
Correspondence:
A Parikh
(anokhip@gmail.com)














