Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.4 Pretoria Abr. 2008
GUIDELINE
Management of Atopic Dermatitis in Adolescents and Adults in South Africa
Werner SinclairI; Jamila AboobakerII; Francois JordaanIII; Deepak ModiIV; Gail ToddV
IMB ChB, MMed (Derm) (Chair of Working Group). Working Group of the Dermatological Society of South Africa
IIMB ChB, FFDerm, FRCP. Working Group of the Dermatological Society of South Africa
IIIMB ChB, MMed (Derm). Working Group of the Dermatological Society of South Africa
IVMB BCh, DTM&H (RCP Lond), MSc, FFDermWorking Group of the Dermatological Society of South Africa
VBSc Agric, MB ChB, FFDerm, PhDWorking Group of the Dermatological Society of South Africa
ABSTRACT
OBJECTIVE: The guidelines for the management of atopic dermatitis in patients older than 18 years have been developed in an attempt to improve the outcomes of treatment of this condition in South Africa. This condition has a major impact on the quality of life of sufferers and it is expected that these guidelines, if implemented, will play a role in achieving this.
RECOMMENDATIONS. All health care workers involved in the management of atopic dermatitis should take note of these guidelines and try to implement them in clinical practice as far as possible. All treatment methods and procedures not substantiated by evidence from the literature should be discontinued and avoided to decrease the financial burden of dermatitis treatment.
VALIDATION: These guidelines were developed through general consensus by a group of five South African dermatologists, from evidence based on extensive literature review. Draft documents were made available for comment to the dermatology community as a whole, via the official website of the Dermatological Society of South Africa. They were also presented and discussed at the annual congress of the Dermatological Society of South Africa. All input from these sources, where appropriate, were then incorporated into these guidelines.
Guidelines sponsor. Novartis initiated the project and sponsored the meetings of the work group and all costs generated by these meetings.
DISCLAIMER: These guidelines do not represent all the possible methods of management applicable to all patients, do not exclude any other reasonable methods and will not ensure successful treatment in every situation. The unique circumstances of each patient should be taken into account by the responsible physician regarding decisions on any specific therapy.
1. Introduction and methods
Atopic dermatitis (AD) is a very common, chronic, inflammatory eczematous skin disease in children, affecting up to 20% of children in Western Europe and Australia. The morbidity and impact on quality of life of these patients can be very severe.1 Women seem to be more severely affected than men2 and the psychological distress suffered correlates well with the severity of the dermatitis.3
There is considerable confusion about uniform criteria for the diagnosis of AD in adults and management is often arbitrary and empirical, with poor outcomes in general. There is therefore a need for standardised guidelines on diagnosing and managing this condition.
A working group of dermatologists, the current fulltime heads of dermatology departments/divisions of five of the medical schools in South Africa, was convened on instruction from the executive committee of the Dermatological Society of South Africa and tasked with publishing these guidelines.
The working group used an evidence-based module -evidence obtained through a thorough literature search published on the topic over the last 15 years. Evidence was graded according to the SIGN4 grading system and all recommendations and statements in the text are marked according to these levels of evidence to denote the strength of evidence and therefore the validity and weight of recommendation:
1.1 Levels of evidence
1++ High-quality meta-analyses, systematic reviews of randomised controlled trials (RCTs), or RCTs with very low risk of bias.
1+ Well-conducted meta-analyses, systematic reviews of RCTs, or RCTs with low risk of bias.
1- Meta-analyses, systematic reviews of RCTs, or RCTs with a high risk of bias.
2++High-quality systematic reviews of case-control or cohort studies; high-quality case-control or cohort studies with a very low risk of confounding, bias or chance and a high probability that the relationship is causal.
2+ Well-conducted case-control or cohort studies with a low risk of confounding, bias or chance and a moderate probability that the relationship is causal.
2- Case-control or cohort studies with a high risk of confounding, bias or chance and a significant risk that the relationship is not causal.
3 Non-analytical studies, e.g. case reports, case series.
4 Expert opinion.
1.2 Grades of recommendation
A At least one meta-analysis, systematic review of RCTs rated as 1++ and directly applicable to the target population; or A systematic review of RCTs or a body of evidence consisting principally of studies rated as 1+, directly applicable to the target population and demonstrating overall consistency of results.
B A body of evidence including studies rated as 2++, directly applicable to the target population and demonstrating overall consistency of results; or Extrapolated evidence from studies rated as 1++ or 1+.
C A body of evidence including studies rated as 2+, directly applicable to the target population and demonstrating overall consistency of results; or Extrapolated evidence from studies rated as 2++.
D Evidence level 3 or 4; or Extrapolated evidence from studies rated as 2+.
0 Not recommendable.
1.3 Scope
These guidelines were developed to address the diagnosis and management of adult patients, from the age of 13 years and above, who suffer from AD.
1. Evers AW, Duller P, van der Valk PG, Kraaimaat FW, van de Kerkhof PC. Common burden of chronic diseases? Contributors to psychological distress in adults with psoriasis and atopic dermatitis. Br J Dermatol 2005; 152: 1275-1281.
2. Holm EA, Esmann S, Jemec GB. Does visible atopic dermatitis affect quality of life more in women than in men? Gend Med; 1: 125-130.
3. Taieb C, Ngyuen C, Myon E. Adults with atopic dermatitis: quality of life impact. J Am Acad Dermatol 2006; 54: AB80.
4. National Institute for Clinical Excellence. SIGN 50. A Guideline Developers Handbook. Edinburgh: National Institute for Clinical Excellence: Guideline Development Methods, 2004: 7.5-7.8.
2. Definitions
The term 'eczema' is derived from the Greek word ekzein which literally means 'to boil out'. In patients with eczema the condition flares up ('boils out') periodically. Flares may be precipitated by irritation of the skin, infection and stress. The term 'dermatitis' refers to inflammation of the skin analogous to 'appendicitis', inflammation of the appendix, 'hepatitis', inflammation of the liver, etc. The terms 'dermatitis' and 'eczema' are nowadays generally regarded as synonymous. Some authors still use the term 'dermatitis' to include all types of cutaneous inflammation, so that all eczema is dermatitis, but not all dermatitis is eczema. The term 'dermatitis', however, should be used with care, as some patients regard it as implying an occupational cause. Unfortunately, there is still no international agreement on the use of these terms. Ackerman1,2 has argued that, as the term eczema cannot be defined in a way that meets with universal approval, it should be dropped from dermatological parlance. There seems to be a consensus that the term still serves a useful purpose for the clinician. Much energy has been needlessly wasted in debating which term should be used. Geographically there is unexplained preference for one or the other.
Acute eczema/dermatitis is characterised by oedema, erythema, vesiculation, exudation, and crusting. Chronic eczema/dermatitis is characterised by lichenification. Lichenification refers to thickening of the skin with exaggeration of the normal markings. Flat-topped, shiny, quadrilateral coalescing papules are enclosed. Subacute eczema/dermatitis shows features overlapping with acute and chronic eczema/dermatitis. Lesions are commonly slightly elevated, red, brownish or purplish in colour with variable scaling. Generally physicians most commonly encounter the subacute presentation of eczema/dermatitis.
The commonest forms of eczema/dermatitis are atopic, seborrhoeic, primary irritant, photoallergic, phototoxic, nummular, asteatotic, stasis and dyshidrotic. Eczema/ dermatitis associated with infection (e.g. dermatophyte) or infestation (e.g. scabies), so-called 'ide' reactions, are additional variants.
The term 'atopy' was first coined in medicine in 1923 by two allergists, Coca and Cook. They defined atopy clinically as a proclivity to develop allergic rhinitis, allergic asthma, and allergic urticaria. Patients whom they considered to be atopic possessed a distinctive antibody, named by them 'reagin' or 'skin-sensitising antibody' because intradermal skin tests to a variety of inhalant allergens, e.g. trees, weeds, grasses, dust, moulds and danders, elicited wheals at sites of some injections. When Sulzberger, in the early 1930s, encountered atopic patients with skin lesions that favoured antecubital and popliteal fossae, he initially called the disorder 'neurodermatitis of atopic type', then 'atopic eczema' and finally 'atopic dermatitis'.
The word 'atopy' is defined as 'a clinical hypersensitivity state that is subject to hereditary influences; included are hay fever, asthma and eczema'. Atopic dermatitis (AD), allergic rhinitis, and asthma are atopic diseases that develop against a complex genetic background, the so-called atopic diathesis. The term atopic eczema or just 'eczema' is frequently used in the UK, whereas 'atopic dermatitis' is used more in the USA. The word atopic in the term atopic eczema is simply an indicator of the frequent association with atopy and the need to separate this clinical phenotype from the other forms of 'eczema' such as irritant or allergic contact eczema, which have other causes and distinct patterns. The terms 'atopic eczema' and 'atopic dermatitis' are synonymous.
The morphology, distribution and evolution of eczema/ dermatitis in atopic eczema/dermatitis are highly characteristic. During the infant phase (birth to 2 years) red scaly lesions develop typically on the cheeks, usually sparing the perioral and perinasal areas. The chin is typically involved and cheilitis is common. A small but significant number of infants develop a generalised eruption. Involvement of the scalp is not uncommon. The diaper area is often spared. Sometimes the cubital/popliteal fossae or other parts of the limbs are involved. During the childhood phase (2 - 12 years) eczema/dermatitis involves the flexural areas (i.e. the antecubital fossae and popliteal fossae) but also the neck, wrist and ankles. During the adult phase (12 years to adult) lesions involve similar areas to those affected during the childhood phase. Additionally hand eczema/dermatitis, periocular eczema/dermatitis and anogenital eczema/dermatitis are common. Morphologically, lesions may be acute, subacute or chronic.
Importantly, for the clinician, the diagnosis of atopic eczema/dermatitis is based on the aforementioned criteria, namely age of the patient, distribution of the rash and morphology of the rash.
Atopic eczema is a difficult disease to define, as the clinical features are highly variable in morphology, body site and time. There is no specific diagnostic test that encompasses all people with typical eczema that can serve as a reference standard. Diagnosis is, therefore, essentially a clinical one.3-5
According to the position paper from the European Academy of Allergology and Clinical Immunology nomenclature task force,6 the term 'Atopic eczema/dermatitis syndrome' (AEDS) should be used as the 'umbrella' term to cover the different subtypes of AD. The new nomenclature (AEDS) underlines the fact that AD is not one, single disease, but rather an aggregation of several diseases with certain clinical characteristics in common. Intrinsic AD (non-allergic AEDS = NAAEDS) fulfils the most commonly used diagnostic criteria for AD (20%). These patients have no associated respiratory diseases, such as bronchial asthma or allergic rhinitis, show normal total serum IgE levels, no specific IgE, and negative skin-prick tests to aeroallergens or foods. Extrinsic AD (allergic AEDS = AAEDS) is commonly associated with respiratory allergies such as rhinitis and asthma, a high level of serum IgE, specific IgE and positive skin-prick tests to aeroallergens or foods (80%). Immunological differences between the IgE-associated type of AD and the non-allergic type can be found in the cell and cytokine pattern in peripheral blood and in the affected skin, and also by phenotyping characterisation of epidermal dendritic cells. The current explanation of this distinction is based on differences in genetics and/or environmental conditions. The classification into AAEDS and NAAEDS at each stage of life, i.e. infancy, childhood, teenage and adult, is essential for the allergological management of patients in respect of allergen avoidance, secondary allergy prevention, and immunotherapy. The risk of an 'atopy march' is significantly lower in children with the NAAEDS. The subdivision of allergic versus non-allergic AD is currently controversial. Cases may transform from one type to the other. This division may not be applicable to adults.
It is quite possible that there are distinct subsets of atopic eczema, e.g. those cases associated with atopy and those who have severe disease with recurrent infections. Until the exact genetic and causative agents are known, it is wiser to consider the clinical disease as one condition. Perhaps sensitivity analyses should be done within clinical trials, or among those who are thought to represent distinct subsets, e.g. those who are definitely atopic with raised circulating IgE to allergens, and those with severe disease and associated asthma.3,4,7-15
Definitions
- Atopy - clinically defined atopy is a proclivity to develop allergic rhinitis, allergic asthma, and allergic urticaria. Patients possess a distinctive skin-sensitising antibody ('reagin'). Intradermal skin tests to a variety of inhalant allergens, e.g. trees, weeds, grasses, dust, moulds and danders, are positive.
- Dermatitis - inflammation of the skin.
- Eczema - inflammation of the skin. Dermatitis and eczema are synonyms and the terms are used interchangeably.
- Intrinsic atopic dermatitis - NAAEDS fulfils the most commonly used diagnostic criteria for AD. These patients have no associated respiratory diseases, such as bronchial asthma or allergic rhinitis, show normal total serum IgE levels, no specific IgE, and negative skin-prick tests to aeroallergens or foods. NAAEDS comprises 20% of cases.
- Extrinsic atopic dermatitis - AAEDS is commonly associated with respiratory allergies such as rhinitis and asthma, a high level of serum IgE, specific IgE and positive skin-prick tests to aeroallergens or foods. AAEDS comprises 80% of cases.
1. Ackerman AB. 'Eczema' revisited. A status report based upon current textbooks of dermatology. Am J Dermatopathol 1994; 16: 517-522; discussion 523-531.
2. Ackerman AB. A plea to expunge the word 'eczema' from the lexicon of dermatology and dermatopathology. Arch Dermatol Res 1982; 272: 407-420.
3. Friedmann PS, Holden CA. Atopic dermatitis. In: Burns DA, Breathnach SM, Cox NH, Griffiths CEM, eds. Rook's Textbook of Dermatology, Vol 1, 7th ed. Oxford: Blackwell Publishing, 2004: 18.1-18.31.
4. Habif TB. Atopic dermatitis: In: Clinical Dermatology, 4th ed. St Louis: Mosby, 2004: 105-125.
5. Simpson EL, Hanifin JM. Atopic dermatitis. Med Clin N Am 2006; 90: 149-167.
6. Johansson SGO, Bieber T, Dahl R, et al. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004; 113: 832-836.
7. Folster-Holst R, Pape M, Buss YL, Christophers E, Weichenthal M. Low prevalence of the intrinsic form of atopic dermatitis among adult patients. Allergy 2006; 61: 629-632.
8. Akdis CA, Akdis M. Immunological differences between intrinsic and extrinsic types of atopic dermatitis. Clin Exp Allergy 2003; 33: 1618-1621.
9. Novak N, Bieber T. Allergic and nonallergic forms of atopic diseases. J Allergy Clin Immunol 2003; 112: 252-262.
10. Wuthrich B, Schmid-Grendelmeier P. The atopic eczema/dermatitis syndrome. Epidemiology, natural course, and immunology of the IgE-associated ('extrinsic') and the nonallergic ('intrinsic') AEDS. J Investig Allergol Clin Immunol 2003; 13: 1-5.
11. Kerschenlohr K, Decard S, Przybilla B, Wollenberg A. Atopy patch test reactions show a rapid influx of inflammatory dendritic epidermal cells in patients with extrinsic atopic dermatitis and patients with intrinsic atopic dermatitis. J Allergy Clin Immunol 2003; 111: 869-874.
12. Ingordo V, D'Andria G, D'Andria C, Tortora A. Results of atopy patch tests with house dust mites in adults with 'intrinsic' and 'extrinsic' atopic dermatitis. J Eur Acad Dermatol Venereol 2002; 16: 450-454.
13. Schmid-Grendelmeier P, Simon D, Simon HU, Akdis CA, Wuthrich B. Epidemiology, clinical features, and immunology of the 'intrinsic' (non-IgE-mediated) type of atopic dermatitis (constitutional dermatitis). Allergy 2001; 56: 841-849.
14. Bieber T. Putative mechanisms underlying chronicity in atopic eczema. Acta Derm Venereol 2005; Suppl 215: 7-10.
15. Williams HC, Johansson SGO. Two types of eczema - or are there? J Allergy Clin Immunol 2005; 116: 1064-1066.
3. Aetiopathogenesis
This is probably multifactorial and most studies investigating the causes of atopic eczema deal with children. There is little to suggest that adult atopic eczema should have a different aetiopathogenesis apart from some clinical features that differ, such as the predominant involvement of the hands and the head and neck.1
3.1 Genetics
Population-based family studies in Europe suggest that in atopic families up to 50% of offspring will have atopic eczema.2 Twin studies showing a concordance rate for atopic eczema of 0.75 for monozygotic twins compared with 0.20 for dizygotic twins support a genetic basis for atopic eczema.2-4 Further evidence for a genetic predisposition to atopic eczema is the finding of candidate genes.2,4,5
3.2 Allergic sensitisation
The predisposition for IgE hyper-responsiveness to allergens defines the term atopy.6 A systematic review of the published evidence for allergic sensitisation and eczema in 12 population studies from around the world has shown that IgE hyper-responsiveness does not necessarily equate to atopic eczema even though it may be associated with the disease phenotype, especially in those with severe disease.7,8 Among those with atopic dermatitis up to 60% were not atopic. Geographical location was associated with the risk of being atopic among those with atopic eczema as compared with normal healthy controls.
In 5 studies that included adolescents and adults the findings were essentially similar. In the single cross-sectional household survey from Ethiopia, which included adults, 15% of those with atopic eczema and 8 % of those without atopic eczema were atopic by skin-prick testing.9 This lack of association between atopic eczema and allergen sensitisation was confirmed in a cross-sectional survey and nested case-control study of children.10
3.3 Environment
A documented increasing prevalence of atopic eczema over the last 30 years is not consistent with genetic drift alone11-13 but supports a strong environmental influence as evidenced by population migration studies.14 These environmental influences, which affect initial disease expression or aggravation of established disease, are summarised in Table 3.I. More detailed information can be obtained from published reviews on gene-environment interactions.2,4,5,14-23
The concept of a damaged barrier function (whether intrinsically normal or dysfunctional) inducing a state of epidermal repair coupled with aberrant responses to epidermal insults in the affected skin best explains the aetiopathogenesis of atopic eczema.4,5,17
1. Sandstrom Falk MH, Faergemann J. Atopic dermatitis in adults: does it disappear with age? Acta Derm Venereol 2006; 86: 135-139.
2. Schultz Larsen F. Genetic epidemiology of atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 113-124.
3. Schultz Larsen F. Atopic dermatitis: a genetic-epidemiologic study in a population-based twin sample. J Am Acad Dermatol 1993; 28: 719-723.
4. Morar N, Willis-Owen SAG, Moffatt MF, Cookson WOCM. The genetics of atopic dermatitis. J Allergy Clin Immunol 2006; 118: 24-34.
5. Cork MJ, Robinson DA, Vasilopoulos Y, et al. New perspectives on epidermal barrier dysfunction in atopic dermatitis: gene-environment interactions. J Allergy Clin Immunol 2006;118: 3-21.
6. Johansson SGO, Bieber T, Dahl R, et al Revised nomenclature review committee of the World Allergy Organisation, October 2003. Allergy Clin Immunol Int - J World Allergy Org 2005; 17:4-8.
7. Flohr C, Johansson SGO, Wahlgren C-F, Williams H. How atopic is atopic dermatitis? J Allergy Clin Immunol 2004; 114: 150-158.
8. Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol 2006; 118: 209-213.
9. Yemaneberhan H, Flohr C, Bekele Z, et al. Prevalence and associated risk factors of atopic dermatitis symptoms in rural and urban Ethiopia. Clin Exp Allergy 2004; 34: 779-785.
10. Abrahams H, Damtew D, Williams H, et al. Early risk factors for atopic dermatitis in Ethiopian children. J Allergy Clin Immunol 2005; 115: 370-376.
11. Williams HC. Atopic eczema - why we should look to the environment. BMJ 1995; 311: 12411242.
12. Williams HC. Is the prevalence of atopic dermatitis increasing? Clin Exp Dermatol 1992; 17:385-391.
13. Diepgen T. Is the prevalence of atopic dermatitis increasing? In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 96-112.
14. Burrell-Morris C, Williams HC. Atopic dermatitis in migrant population. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 169-182.
15. Flohr C, Pascoe D, Williams HC. Atopic dermatitis and the 'hygiene hypothesis': too clean to be true? Br J Dermatol 2005; 152: 202-216.
16. Akdis CA, Akdai M, Bieber T, et al. for the European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Group. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology /American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. J Allergy Clin Immunol 2006; 118:152-189.
17. Taieb A, Hanifin J, Cooper K, et al. Proceedings of the 4th Georg Rajka International Symposium on atopic dermatitis, Aacachon, France, September 15-17, 2005. J Allergy Clin Immunol 2006; 117: 378-390.
18. McNally N, Phillips D. Geographical studies of atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 71-84.
19. McNally N, Phillips D. Social factors and atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 139-154.
20. Godfrey K. Fetal and perinatal origins of atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 125-138.
21. Schafer T, Ring J. The possible role of environmental pollution in the development of atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 155-168.
22. Kolmer H, Platts-Mills TAE. The role of inhalant allergens in atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 1183-1201.
23. Braae Olesen A, Thestrup-Petersen K. The 'old mother' hypothesis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 148-154.
24. Flohr C, Tuyen LN, Lewis S, et al. Poor sanitation and helminth infection protect against skin sensitisation in Vietnamese children: a cross-sectional study. J Allergy Clin Immunol 2006; 118:1305-1311.
25. Adler UC. The influence of childhood infections and vaccination on the development of atopy: a systematic review of direct epidemiological evidence. Homeopathy 2005; 94: 182-195.
26. Williams HC, Wuthrich B. The natural history of atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 41-59.
27. Hoare C, Li Wan Po A, Williams H. Systematic review of treatments for atopic eczema. Health Technology Assessment 2000; 4(37): 1-191.
4. Epidemiology
4.1 How common is atopic eczema?
Much of the published work on the epidemiology of atopic eczema has been done in children1 and a variety of prevalence measures have been used which include lifetime prevalence, point prevalence and 1-year prevalence rates. The International Study of Asthma and Allergies in Childhood (ISAAC)2,3 has documented that the 1-year prevalence rate varies worldwide depending on the population and geographical area studied (globally, nationally or locally). A comparison of the two studies documents a decline or plateau in the 1-year prevalence rate in the developed world but an increasing prevalence in the developing world.
While it is accepted that atopic eczema is a particular problem in children, the burden of disease is significant in adults. A study among adults in Scotland documents a 0.2% 1-year point prevalence for atopic eczema in those over 40 years of age. Adults accounted for 38% of the atopic eczema population.4
Few incidence studies have been done and these are in cohorts of children.5
There are no studies addressing the prevalence of atopic eczema in South African adults. The phase I ISAAC study2 of 13 - 14-year-old schoolchildren in Cape Town showed an 8.3% 1-year prevalence rate with 2.3% having severe disease. The phase III follow-up study3 documented an increased 1-year prevalence of 13.3% among children of the same age. In 3 - 11-year-old normal children the 1-year prevalence rate was 1 - 2.5% in Xhosa children depending on the methodology used to define atopic eczema.6
4.2 What is the natural history of atopic eczema?
Studies on the natural history of atopic eczema document up to 60% spontaneous clearing by puberty.5,7,8 Studies on adults are rare but suggest that early adult atopic eczema is associated with persistent disease in later life. Atopic eczema may recur in adults and the risk is associated with the severity and persistence of childhood atopic eczema. In adults the clinical picture may be altered. Patients may present with hand eczema caused by exposure to additional insults such as irritants, e.g. wet work, detergents, chemicals and solvents, or head and neck involvement.9
The historical concept of the 'atopic march' where atopic eczema in children would evolve into mucosal forms of atopic disease has been challenged by cohort studies.10,11 Early wheeze and specific sensitisation pattern (wheat, cat, mite, soy, birch) were predictors of wheezing at school age irrespective of the presence of atopic eczema in a German birth cohort study.8 The development of rhinoconjunctivitis is more strongly associated with atopic eczema than is asthma. It is probable that there are many subsets of the atopic eczema phenotype.
Studies assessing the severity of atopic eczema in Europe revealed that in children, 84% have mild, 14% moderate and 2% severe disease.12,13 In adult cohorts, those who had severe disease accounted for 12% using the SCORAD scoring system.9
1. Diepgen T. Is the prevalence of atopic dermatitis increasing? In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 96-112.
2. Williams H, Robertson C, Stewart A, et al. Worldwide variations in the prevalence of symptoms of atopic eczema in the International Study of Asthma and Allergies in Childhood. J Allergy Clin Immunol 1999; 103: 125-138.
3. Asher MI, Montefort S, Bjorkstein B, et al. Worlwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phase One and Three repeat multicountry cross-sectional surveys. Lancet 2006; 368: 733-743.
4. Herd RM, Tidman MJ, Prescott RJ, Hunter JAA. Prevalence of atopic eczema in the community: the Lothian atopic dermatitis study. Br J Dermatol 1996; 135: 18-19.
5. Halkjaer LB, Loland l, Buchvald FF, et al. Development of atopic dermatitis during the first 3 years of life. The Copenhagen prospective study on asthma in childhood cohort study in high risk children. Arch Dermatol 2006; 142: 561-566.
6. Chalmers DA, Todd G, Saxe N, et al. Validation of the UK Working Party criteria for atopic eczema in a Xhosa-speaking African population. Br J Dermatol 2007; 156: 111-116.
7. Williams HC, Wuthrich B. The natural history of atopic dermatitis. In: Williams HC, ed. Atopic Dermatitis. The Epidemiology, Causes and Prevention of Atopic Eczema. Cambridge: Cambridge University Press, 2000: 41-59.
8. Illi S, von Mutius, Lau S, et al. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol 2004; 113: 925-931.
9. Sandstrom Falk MH, Faergemann J. Atopic dermatitis in adults: does it disappear with age? Acta Derm Venereol 2006; 86: 135-139.
10. Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol 2006; 118: 209-213.
11. Flohr C, Johansson SGO, Wahlgren C-F, Williams H. How atopic is atopic dermatitis? J Allergy Clin Immunol 2004; 114: 150-158.
12. Emerson RM, Williams HC, Allen BR. Severity distribution of atopic dermatitis in the community and its relationship to secondary referral. Br J Dermatol 1998; 139: 73-76.
13. Dotterud LK, KvammenB, Lund E, Falk ES. Prevalence and some clinical aspects of atopic dermatitis in the community of Sor-Varanger. Acta Dermatol Venereol 1995; 75: 50-53.
5. Diagnosis of atopic dermatitis in adults
The diagnosis of this condition is often not straightforward and several other conditions have to be considered in the differential diagnosis (see below). Where the disease represents mere continuation of atopic dermatitis (AD) from childhood, the diagnosis is usually easy and the clinical picture also typical. Difficulty arises where onset occurs after the age of 18 years (adult-onset AD) and in these cases the disease pattern is often not obvious, although it may still present with the usual flexural dermatitis seen in children. Non-typical morphology and localisation are common with nummular, prurigolike, follicular and seborrhoeic patterns often seen.1 Erythroderma is a rare manifestation of AD in adults.2 The physical and environmental factors at play in adults differ from those in children, and these are responsible for the different patterns of involvement.
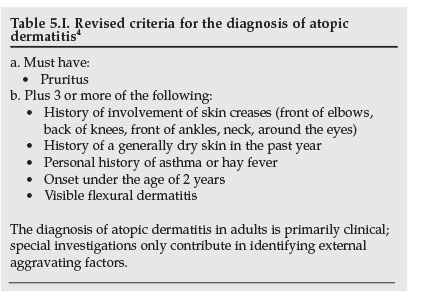
The time-honoured criteria set out by Hanifin and Rajka3 have received severe criticism over the past decade or two, and these criteria are even more unreliable when applied to adult cases. Williams et al. developed a revised set of criteria and these were validated in the hospital setting5 and in the community.6 It is the opinion of this work group that these criteria should be adopted for the diagnosis of AD in adults in South Africa, even though a recent study7 has shown that these criteria are not reliable when applied in the low prevalence, rural areas of the Eastern Cape, in a study done in children.
The revised criteria are set out in Table 5.I.
The histological findings on skin biopsy can be suggestive of the diagnosis, but on the whole it is not helpful and cannot be relied upon to make the diagnosis.4
Total IgE levels are significantly raised in about 80% of cases, being normal in the rest, therefore reducing the value thereof in the diagnosis. The level of IgE does not correlate with severity of the dermatitis and 15% of non-atopic individuals have raised IgE levels.
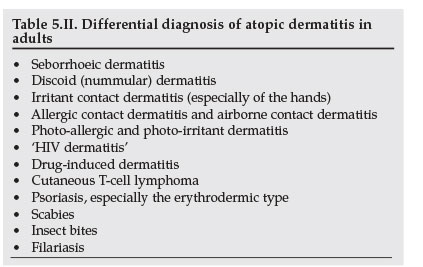
Several conditions have to be considered in the differential diagnosis of AD in adults, as listed in Table 5.II. These have to be excluded on clinical grounds and by employing appropriate investigations.
5.1 Measuring the severity of AD
The severity of dermatitis in individual cases can be measured and monitored in several ways. The SCORAD index (SCORing Atopic Dermatitis)8 uses clinical parameters developed by the European Task Force on Atopic Dermatitis (1990-1992) where the patient's condition is compared with a set of standard colour photographs and parameters are scored on an easy-to-use computer program, which assigns a numerical value to the severity of the dermatitis at that point in time.
The Objective Severity Assessment of Atopic Dermatitis
(OSAAD) score utilises non-invasive bioengineering methods and computer-assisted estimates of disease extent to measure transepidermal water loss, stratum corneum hydration and affected body surface. A numerical score is then produced to denote severity.9 The reliability and sensitivity of this test in adult patients have been confirmed recently,10 when it was compared with SCORAD and it also significantly correlated with serum levels of interleukin-16, which seems to be a sensitive and reliable marker of disease activity in AD,11 also in adults.12
The three-item severity score only utilises excoriations, erythema and papulation/vesiculation as parameters and best reflects the severity of dermatitis from the patient's point of view. This is also far more practical for use in clinical practice.13
It is the opinion of this panel that the severity assessment should be simplified to make it easy to use in practice. The aim is to stratify treatment accordingly in individual patients. We propose:
1. A measurement of the area involved in percentage of body surface, where 1% body surface is equal to the size of one of the patient's hands.
2. Acute, subacute or chronic changes, where acute changes would imply more severe dermatitis. These changes have been explained under the heading of definitions.
3. Impact on the quality of life of the patient, as measured by sleep disturbance, absenteeism, visible scratching, social withdrawal, etc., according to the judgement of the clinician managing the case.
Dermatitis can then be classified as mild, moderate or severe as outlined in Table 5.III. Stratification of treatment according to this scheme will be explained below.
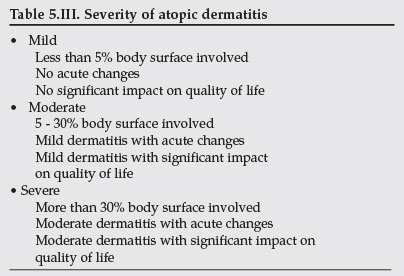
A flare of dermatitis can be defined as any episode of 'upgrading' of the dermatitis from one group to the next, e.g. mild to moderate.
1. Ozkaya E. Adult-onset atopic dermatitis. J Am Acad Dermatol 2005; 52: 579-582.
2. Rym BM, Mourad M, Bechir Z, et al. Erythroderma in adults: a report of 80 cases. Int J Dermatol 2005; 44: 731-735.
3. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh) 1980;suppl 92: 44-47.
4. Williams HC, Burney PG, Hay RJ, et al. The U.K. Working Party's diagnostic criteria for atopic dermatitis. I. Derivation of a minimum set of discriminators for atopic dermatitis. Br J Dermatol 1994; 131: 383-396.
5. Williams HC, Burney PG, Pembroke AC, Hay RJ. The U.K. Working Party's diagnostic criteria for atopic dermatitis. III. Independent hospital validation. Br J Dermatol 1994; 131: 406-416.
6. Williams HC, Burney PG, Strachan D, Hay RJ. The U.K. Working Party's diagnostic criteria for atopic dermatitis. II. Observer variation of clinical diagnosis and signs of atopic dermatitis. Br J Dermatol 1994; 131: 397-405.
7. Chalmers DA, Todd G, Saxe N, et al. Validation of the U.K. Working Party diagnostic criteria for atopic eczema in a Xhoza-speaking African population. Br J Dermatol 2007; 156: 111-116.
8. European Task Force on Atopic Dermatitis. Severity scoring of atopic dermatitis. The SCORAD index: Consensus report of the European Task Force on Atopic Dermatitis. Dermatology 1993; 186: 23-31.
9. Sugarman J, Fluhr J, Fowler A, et al. The Objective Severity Assessment Atopic Dermatitis score. Arch Dermatol 2003; 139: 1417-1422.
10. Angelova-Fischer I, Bauer A, Hipler UC, et al. The Objective Severity Assessment of Atopic Dermatitis (OSAAD) score: validity, reliability and sensitivity in adult patients with atopic dermatitis. Br J Dermatol 2005; 153: 767-773.
11. Frezzolini A, Paradisi M, Faffiro A, et al. Circulating interleukin-16 (Il-16) in children with atopic eczema/dermatitis syndrome (AEDS): a novel marker of disease activity. Acta Derm Venereol 2002; 57: 815-820.
12. Masuda K, Katoh N, Okuda F, Kishimoto S. Increased levels of serum interleukin-16 in adult type atopic dermatitis. Acta Derm Venereol 2003; 83: 49-53.
13. Charman CR, Venn AJ, Williams HC. Measuring atopic eczema severity visually: which variables are most important to patients? Arch Dermatol 2005; 141: 1146-1151.
6. Special investigations in atopic dermatitis
Special investigations are rarely essential to make a diagnosis of atopic eczema. Investigations are done mainly to identify trigger factors that flare up or aggravate eczema so that patients may be advised to avoid these. These investigations are useful mainly in the management of atopic eczema in children.
The role of skin biopsy and total IgE levels has been addressed.
Formal patch testing can help to diagnose superimposed allergic contact factors,1 but has no value in diagnosing or excluding the diagnosis of AD. This is probably of more value in the adult-onset subgroup of patients.
The skin-prick test (SPT) is the most common procedure used to confirm food allergy. These tests are also used to confirm inhaled or aeroallergens. Fresh food extracts of cow's milk, egg, wheat, soy, fish and peanuts are used. A standardised test lancet is dipped into the test food solution and the patient's skin is pricked with the allergen-impregnated lancet. A new lancet is used for each skin test. The test site is then observed for 15 - 20 minutes and any wheal reaction measured. A positive control is a wheal of 3 mm or more greater than the negative saline control. A positive test is a wheal produced by histamine. This should measure at least 3 mm.
Variants of SPT include the scratch patch test (the skin is scratched first and then the food applied under an occlusive patch) and the skin food application test (food is applied to skin without pricking and examined at 10 minute intervals for a reaction). These tests are not commonly used as they offer no additional benefit to the routine SPT.
Patients have to be off steroids and antihistamines for 72 hours prior to SPTs. It is important to note that SPT antigen kits have a fixed shelf life.
Radioallergosorbent tests (RASTs) for specific food IgE antibodies measure serum specific IgE to recognised food allergens in kU/l. The tests are less accurate than SPTs. The food mix (egg white, milk, gluten, peanut and wheat) is commonly used in children. In adults egg yolk and gluten are frequently used. RASTs are expensive. The tests are not affected by steroids and antihistamines.
As mentioned previously SPT and RAST have a high negative predictive value (95%) for the diagnosis of food and environmental allergies but positive tests are less reliable. The tests are of greater value in excluding allergies. Positive tests are of far less value with only a 40% predictive value.2 Atopic individuals typically show numerous positive results on these tests and the exact clinical relevance of these reactions to specific allergens is doubtful.3
In atopy patch tests (APT) common aeroallergens and foods are patch-tested to investigate the role of these allergens in individual cases.4 Antigens include house-dust mite (HDM), cat dander, Bermuda grass and cockroach. The results correlate somewhat with RAST and SPT, but further refinement is necessary to make the test more reliable.5 Unlike SPTs which measure IgE sensitivity to HDM, the APT elicits a delayed type response mediated by specific CD4+ which clinically resembles eczema. The patch test reaction to aeroallergens is specific to sensitised atopic eczema patients and does not occur in healthy individuals. Although APTs are found more commonly in the presence of high IgE levels, they may also be absent despite them. APT is much more likely to be positive among patients whose eczema is predominantly on exposed parts of the skin. The ATPs are currently being standardised. Combining APT and SPT may improve accuracy.6
Double-blind placebo-controlled food challenge tests are the gold standard for diagnosing associated food allergies, but they are very difficult to perform, time consuming and available to few. In adult patients these are seldom performed.7,8
Some foods give rise to clinical symptoms of urticaria, itching, angio-oedema and exacerbation of eczema where the histamine release is by non-IgE immunological mechanisms. For these reactions the term food intolerance is suggested. Many 'junk' foods appear to aggravate eczema by this mechanism. These foods are best identified by using a basic elimination diet for 2 weeks to assess whether the symptoms improve. During this period, rice cakes, rice, apples, pears, apricots, grapes (no skin), lamb, chicken (free range), potatoes, sweet potato, butternut, beetroot, asparagus, lettuce, squash, olive or sunflower oil and table salt are allowed. Tinned, packet or bottled foods are forbidden. Test foods are introduced one by one on a daily basis. A repeat challenge is necessary to confirm the culprit food. These elimination diets are best supervised by an allergist with the assistance of a dietician.
If immunodeficiency is suspected with atopic eczema, tests like HTLV1, HIV, immunoglobulin levels, T and B cell number and functions will need to be done. If secondary bacterial infections are suspected, appropriate swab for microscopy, culture and sensitivity is necessary. Tzanck smears are recommended for suspected herpes infection.
It is the opinion of this panel that special investigations are seldom helpful in the management of AD in adults, they are not cost-effective and investigations should be kept to a minimum.
1. Vender RB. The utility of patch testing children with atopic dermatitis. Skin Therapy Lett 2002;7: 4-6.
2. Eigenmann PA, Sampson HA. Interpreting skin prick tests in the evaluation of food allergy in children. Pediatr Allergy Immunol 1998; 9: 186-191.
3. Sampson HA, Albergo R. Comparison of results of skin tests, RAST and double-blinded, placebocontrolled food challenges in children with atopic dermatitis. J Allergy Clin Immunol 1984; 74: 26-33.
4. Darsow U, Vieluf D, Ring J. Evaluating the relevance of aeroallergen sensitization in atopic eczema with the atopy patch test: a randomized, double-blind multicenter study. Atopy Patch Test Study Group. J Am Acad Dermatol 1999; 40: 187-193.
5. Goon A, Leow YH, Chan YH, Ng SK, Goh CL. Clin Exp Dermatol 2005; 30: 627-631.
6. Isolauri E, Turjanmaa K. Combined skin prick and patch testing enhances identification of food allergy in infants with atopic dermatitis. J Allergy Clin Immunol 1996; 97: 9-15.
7. De Maat-Bleeker F, Bruijnzeel-Koomen C. Food allergy in adults with atopic dermatitis. Monogr Allergy 1996; 32: 157-163.
8. Munkvad M, Danielsen L, Hoj L, et al. Antigen-free diet in adult patients with atopic dermatitis: a double-blind controlled study. Acta Derm Venereol 1984; 64: 524-528.
7. Non-pharmacological treatment modalities for atopic dermatitis
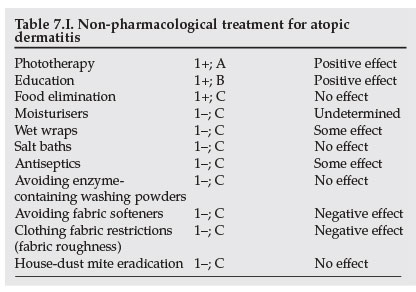
These non-therapeutic interventions are used together with standard treatments to prevent or improve control of atopic eczema. Most of the studies involve children; a few include adolescents and occasionally adults. Only evidence for adolescents and adults is included. Table 7.I summarises the results.
7.1 Moisturisers [1-; C]
Moisturisers are classified according to their mechanism of action as occlusive (prevent water loss from the skin) or humectant (improve water binding in the skin). They are widely used to relieve symptoms in many skin diseases and may also reduce pruritus through an unknown mechanism.1 They can be applied directly to the skin or used as a bath additive. Generally emollients are side-effect free but they can cause contact dermatitis.
Moisturisers must be applied frequently as the desired effects may last only a few hours. There is little basis for suggesting the use of one moisturiser as opposed to another. Adults need a minimum of 500 g/week for the whole body.
There is a paucity of evidence to support a direct benefit for moisturisers in atopic eczema but they may improve barrier function and transepidermal water loss in affected patents.2-4
Despite the lack of good clinical trials to support the use of moisturisers, patients should be advised to use them with personal preference directing the emollient of choice.5
7.2 Phototherapy [1+; A]
This therapy is well established as second-line treatment for adults, 4-6 but requires personnel expertise for safe, effective delivery. Research suggests that the effects are mediated by modulation of the immune system.
The following therapy options are available: broad-band UVB (280 - 320 nm), narrow-band UVB (311 - 313 nm), UVA (320 - 400 nm), UVA1 (340 - 400 nm), psoralen (oral) and UVA (PUVA), and bath-PUVA. In addition combinations of UVB and topical corticosteroids and UVB with UVA, as well as UVA1 medium- and high-dose therapy, have all showed favourable results.
Systematic reviews of randomised clinical trials have shown that phototherapy is effective and beneficial in the short-term treatment of atopic eczema in adults and adolescents.7,8 Meta-analysis of the trials was not possible as disease severity, treatment regimen and outcome scoring methods varied widely. Current evidence on the choice of phototherapy from these limited studies suggests that UVA1 (if available) is a useful single therapy for acute eczema and flares while UVB (TL01), UVA and bath-PUVA are beneficial for all forms of eczema. The long-term effects of phototherapy include an increased risk for developing skin cancer while the short-term adverse effects include itch and acute burns.
Guidelines of care for phototherapy and photochemotherapy are documented.9
7.3 Wet wraps [1-; C]
A critical review of wet wraps as an intervention for severe and refractory atopic eczema10 found the wet-wrap method varied widely between studies, making comparisons difficult. Their findings suggest that wet wraps (cream or ointment applied to the skin, then covered by a double layer of cotton bandages, with a moist first layer and a dry second layer and kept in place for 24 hours) were safe short-term interventions. Used together with topical steroids they were more efficacious. They reduced the absolute amount of topical steroid required and could be recommended as a second-line short-term (14 days) intervention to limit systemic absorption. The number of adolescents and adults included in the review was small, and the authors raise the concern of possible increased risk of striae if wet wraps are used with topical steroids during puberty.
Studies in mild to moderate eczema comparing the addition of wet wraps with standard therapy showed no additional benefit from wet wraps in children.11
Evidence for use in adults is minimal.
No studies have been done in South Africa.
7.4 Salt baths [1-; C]
Although salt has been used for centuries for treating skin diseases, including eczema, there is little evidence to support the use of salt baths for treating atopic eczema in adults, according to a systematic review.7
7.5 Antiseptics [1-; C]
Although secondary infection and colonisation of damaged skin by bacteria is understandable, the role of bacteria in the pathogenesis of atopic eczema is not clear.
Evidence for the regular use of antimicrobial and antiseptic agents being of benefit in the control of uninfected eczema has been reported in a systematic review of trials that included adults and adolescents.12 There was little evidence to support the use of antiseptics in either bath water or applied directly to the skin. The intermittent use of short-term mupirocin was of benefit for relapsing atopic eczema that was not overtly infected and there were no randomised control trials supporting the use of oral antibiotics.
No benefit for the regular use of topical antifungals in addition to topical steroids was found for 60 adult patients with head and neck involvement, although yeast colonisation fell significantly.
7.6 Laundry practices
Patients are often advised to avoid certain products based on reported cases of skin irritation or allergy after exposure. Evidence for this advice is scarce.3,7
7.6.1 Enzyme-containing washing powders [1-; C]
One randomised double-blind crossover study in adults failed to show any benefit from avoiding enzyme-containing washing powders for laundry.
7.6.2 Fabric softeners [1-; C]
For both the irritated and normal skin, the 'softened' fabric was less irritating by all measured parameters, in a right/left comparison study of atopic eczema volunteers with no active eczema.
There is limited evidence suggesting that laundry practices have little effect on atopic eczema control. Logic would support adopting practices that are simple and reduce undue exposure to potential allergens and irritants in those with impaired skin barrier function. The benefit of using fabric softeners, that reduce fabric roughness, is indirectly supported by evidence relating to clothing choices (see below). The development of fabric softeners free of perfumes would be in keeping with the simple approach alluded to above.
7.7 Clothing [1-; C]
Wool intolerance is a minor criterion for diagnosis in atopic eczema according to Hannifin. Despite this there are few studies on the benefits of specific clothing in atopic eczema. In the NHS systematic review two small, randomised controlled trials were reported and both included adult patients.7 Itching and discomfort caused by garments made of various fibres, including cotton, of different weave, weight and roughness was related to fibre weight and roughness only. Sweating increased discomfort for all tested fibres.
Fabric roughness - not the type of textile - determines skin irritation. This is indirectly supported by the finding that cloth washed with fabric 'softeners' causes less irritation than control cloth.
As these studies were done in Europe they may have no bearing to the South African climate where the more occlusive synthetic materials may provoke sweating and itch.
7.8 Education [1+; B]
Education interventions cover a broad range of approaches that may be directed at the parents, patient (child or adult), family or community. These interventions, which can include audiovisual tools, printed literature, lectures, demonstrations and interactive session formats, are aimed at changing behaviour by increasing knowledge or skills and thereby empowering self-management. They can be delivered by various individual members of the health care team, by multidisciplinary teams or as self-directed learning. They may be combined with psychological interventions.
A systematic review13 and randomised14-18 controlled trials involving education intervention in adolescent and adult patients reported significant benefits. These included improved severity and self-care, increased knowledge of treatments and reduced need for medical help.
There is some evidence that education intervention in addition to standard therapy improves atopic eczema disease control.19 These interventions should be delivered by suitably trained personnel. The most effective educational process still needs to be researched.
7.9 Allergen avoidance
Recent evidence has demonstrated that up to two-thirds of those with the atopic eczema phenotype do not show IgE hyper-responsiveness and are thus not atopic by definition.20,21 Despite this it remains fashionable for patients with atopic eczema to be treated with allergen avoidance, with or without supporting evidence of allergy.
Avoidance of allergen exposure can be associated with prevention of atopic disease or aggravation of established disease. Once sensitised, desensitising therapeutic interventions can be attempted. Only the evidence for a role of allergen avoidance in established atopic eczema will be addressed here.
7.9.1 Inhalant allergy - house-dust mite [1-; C]
Circumstantial evidence suggests an important precipitating role for house-dust mite allergens in patients with atopic eczema. Reducing exposure to the allergen should theoretically be beneficial for cases of established eczema.
A review of the evidence for house-dust mite reduction revealed 4 randomised controlled trials done on adults with atopic eczema.3,7 From these, there is little evidence to support a clinical benefit from house-dust mite allergen reduction in adult atopic eczema patients.
7.9.2 Ingestant allergy - food [1+; B]
The evidence for dietary interventions has been reviewed.22 Food avoidance can be achieved in several ways:
- The elimination of a specific food, e.g. egg - simple elimination
- The elimination of all but a few foods - few foods diet
- A liquid diet of amino acids, carbohydrate, fat, minerals and vitamins - elemental diet.
Simple diet
A randomised cross-over study in children and young adults comparing an egg and cow's milk free diet (soy milk substitute) with a normal diet (egg and cow's milk cocktail) had a high drop-out rate but no statistically significant differences in severity scores were found.23
Few foods diet
No adult randomised controlled trials have been done.
Elemental diet
An elemental diet compared with a blended diluted hospital diet in a parallel randomised controlled trial of hospitalised adults with atopic eczema involving more than 10% body surface area showed no benefit for the unpalatable diet despite one-third of the patients having a history of food intolerance.24
There is no good evidence to support elimination diets for adults with atopic eczema.
1. Lodén M. The clinical benefit of moisturizers. J Eur Acad Dermatol Venereol 2005; 19: 672-688.
2. Hoare C, Li Wan Po A, Williams H. Systematic review of treatments for atopic eczema. Health Technology Assessment 2000; 4(37): 31-38.
3. Williams H, Thomas K, Smethurst A, Ravenscroft J, Charman C. Atopic eczema. In: Williams H, ed. Evidenced-based Dermatology. London: BMJ Publishing Group, 2003: Chapter 17: 144218.
4. Williams HC. Atopic eczema. N Engl J Med 2005; 352: 2314-224.
5. McHenry PM, Williams HC, Bingham EA. Management of atopic eczema: Joint Workshop of the British Association of Dermatologists and the Research Unit of the Royal College of Physicians of London. BMJ 1995; 310: 843-847.
6. Scheinfeld NS, Tutrone WD, Weinberg JM, DeLeo VA. Phototherapy of atopic dermatitis. Clin Dermatol 2003; 21: 241-248.
7. Hoare C, Li Wan Po A, Williams H. Systematic review of treatments for atopic eczema. Health Technology Assessment 2000; 4(37): 81-92.
8. Meduri NB, Vandergiff T, Rasmussen H, Jacobe H. Phototherapy in the management of atopic dermatitis: a systematic review. Photodermatol Photoimmunol Photomed 2007; 23: 106-112.
9. Drake LA, et al. AAD Committee on Guidelines of Care. Guidelines of care for phototherapy and photochemotherapy. J Am Acad Dermatol 1994; 31: 643-648.
10. Devilliers ACA, Oranje AP. Efficacy and safety of 'wet-wrap' dressings as an intervention treatment in children with severe and/or refractory atopic dermatitis: a critical review of the literature. Br J Dermatol 2006; 154: 579-585.
11. Beattie PE, Lewis-Jones MS. A pilot study on the use of wet wraps in infants with moderate atopic eczema. Clin Exp Dermatol 2004; 29: 348-353.
12. Hoare C, Li Wan Po A, Williams H. Systematic review of treatment for atopic eczema. Health Technology Assessment 2000; 4(37): 39-44.
13. Ersser SJ, Latter S, Sibley A, Satherley PA, Welbourne S. Psychological and educational interventions for atopic eczema in children. Cochrane Database Syst Rev 2007; 3: CD004054.
14. Staab D, Diepgen TL, Fartasch M, et al. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomized controlled trial. BMJ 2006; 332: 933-938.
15. Gradwell C, Thomas KS, English JSC, Williams HC. A randomised controlled trial of nurse follow-up clinics: do they help patients and do they free up consultants' time? Br J Dermatol 2002; 147: 513-517.
16. Coenraads PJ, Span L, Jaspers JP, Fidler V. Intensive patient education and treatment program for young adults with atopic eczema. Hautarzt 2001; 52(5): 428-433.
17. Jaspers JPC, Span L, Molier L, Coenraads PJ. A multimodal education and treatment program for young adults with atopic dermatitis: a randomised controlled trial. Dermatol Psychosomatics 2000; 1: 148-153.
18. Ehlers A, Strangier U, Gieler U. Treatment of atopic dermatitis: a comparison of psychological and dermatological approaches to relapse prevention. J Consult Clin Psychol 1995; 63: 624-635.
19. Williams HC. Educational programmes for young people with eczema. BMJ 2006; 332: 923-924.
20. Flohr C, Johansson SGO, Wahlgren C-F, Williams H. How atopic is atopic dermatitis? J Allergy Clin Immunol 2004; 114: 150-158.
21. Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol 2006; 118: 209-213.
22. Hoare C, Li Wan Po A, Williams H. Systematic review of treatment for atopic eczema. Health Technology Assessment 2000; 4(37): 65-80.
23. Neild VS, Marsden RA, Bailes JA, Bland JM. Egg and milk exclusion diets in atopic eczema. Br J Dermatol 1986; 114: 117-123.
24. Munkvad M, Danielsen L, Hoj L, et al. Antigen-free diet in adult patients with atopic dermatitis: a double-blind controlled study. Acta Derm Venereol 1984; 64: 524-528
8. Pharmacological treatment of atopic dermatitis
Difficult, refractory cases should ideally be referred to an experienced dermatologist.
The reader can refer to guidelines published recently in the European and American literature:
Akdis CA, Akdis M, Bieber T, et al. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. J Allergy Clin Immunol 2006; 118: 152-169.
Ellis C, Luger T, Abeck D, et al. International Consensus Conference on Atopic Dermatitis II (ICCAD II*): clinical update and current treatment strategies. Br J Dermatol 2003; 148 (Suppl 63): 3-10.
The more important drugs are firstly discussed in detail and in the next section a general approach is given to treating the different degrees of severity of the condition, followed by a suggested algorithm.
8.1 Topical corticosteroids (TCS) [1+; B]
Topical corticosteroids continue to be the mainstay of atopic dermatitis (AD) treatment.1,2 Different strengths and formulations of TCS are available. There are no adequate trials to suggest superiority of one over the other.
Guidelines for prescribing TCS are well described.3,4 Preparations of very weak or moderate strength are used on the face and genital area, whereas those of moderate or potent strength are used on other areas of the body.5 Patients should be educated about the different steroid potencies in order to minimise untoward side-effects.6
The vehicle through which the active steroid is delivered plays an important role in absorption and can enhance its efficacy. Generally ointments are more effective than creams, as the emollient action and occlusive effect result in better penetration. Ointments also require fewer preservatives so the potential for irritant and allergic reactions is lower. Wet wraps and application under occlusion enhance absorption of topical steroids. A novel foam vehicle for drug delivery is available in the USA.7
Topical steroids can be used for 10 - 14 days when the eczema is active, followed by 'holidays' with just emollients. TCS can also be used in bursts of 3 - 7 days to treat exacerbations. This rationale can be extended to using potent TCS for a few days to initiate control, followed by use of a milder potency TCS and/or emollient.4 For chronic lichenified eczema, however, frequent potent steroids are required for much longer periods.
The amount of TCS to use is a frequent practical problem for patients. The fingertip unit is useful: index finger: from distal crease to finger tip = 0.5 g. This aids monitoring compliance and use. There is no clear evidence to suggest that twice-daily application of TCS is better than a once-daily application. It would be justifiable to use once-daily corticosteroids as a first step in all patients with AD, thus reducing cost, improving compliance and reducing side-effects.
No convincing evidence is available to demonstrate superior clinical efficacy of corticosteroid-antibiotic combination to corticosteroid alone.
There is no randomised controlled trial (RCT) evidence to support the notion that diluting TCS reduces adverse effects while maintaining efficacy in AD.
The reduced efficacy of TCS is thought to be related to disease severity rather than glucocorticoid resistance.8
There are many challenges on the subject of TCS use, especially in the light of steroid abuse, steroid misuse, steroid phobia and side-effects. There are as a result many publications addressing these issues and certain recommendations as already discussed have been suggested.9
Adverse effects are well documented and it is important to recognise the side-effects of skin atrophy, telangiectasia, hypopigmentation, steroid acne, hirsutism, rosacea and contact sensitisation to the steroid itself. Skin thinning is not a problem when topical steroids are used correctly. Uncommon systemic effects are the suppression of the hypothalamic-pituitary-adrenal axis, growth retardation, tachyphylaxis, glaucoma, cataract formation and Cushing's syndrome.10
Over recent years the risk of adverse effects of TCS has been reduced by optimising application protocols and using newer steroid preparations with improved risk/benefit ratios, e.g. prednicarbate, mometasone furoate, fluticasone and methylprednisolone aceponate.5,6
The judicious use of TCS would be short-term appropriate application as initial monotherapy or in combination with other therapeutic agents that ideally possess complementing mechanisms of action. These drugs could be either systemic or topical agents such as newer topical calcineurin inhibitors.11
8.2 Topical calcineurin inhibitors (TCIs) [2+; C]
TCIs (pimecrolimus and tacrolimus) are complex macrocyclic compounds that result in selective inhibition of cytokine transcription in activated T-cells.3 Pimecrolimus selectively targets T cells and mast cells. In contrast to tacrolimus, pimecrolimus has no effects on the differentiation, maturation and function of dendritic cells. In contrast to corticosteroids, pimecrolimus does not affect endothelial cells and fibroblasts and does not induce skin atrophy. Clinical trial data12-14 have proven that pimecrolimus reduces the incidence of flares and has a significant effect on reducing pruritus; these trials have not been performed for tacrolimus.
Pimecrolimus and tacrolimus are safe and effective in reducing the severity of AD symptoms in children and adults. Only pimecrolimus is available in South Africa. Pimecrolimus has been studied in clinical trials in infants as young as 3 months, as compared with tacrolimus from 2 years.
TCIs provide a steroid-free, anti-inflammatory topical therapy for AD. The anti-inflammatory potency of 0.1% tacrolimus ointment is similar to a corticosteroid with moderate potency15 whereas 1% pimecrolimus cream is less active.12 Both agents proved to be effective with a good safety profile for a period of up to 2 years with pimecrolimus and up to 4 years with tacrolimus.13,14
TCIs are frequently associated with a transient burning sensation of the skin, less so with pimecrolimus than tacrolimus.16 TCIs are not associated with skin atrophy and are therefore useful for the face and intertriginous areas.17 This property can be an advantage of long-term use and tacrolimus ointment therapy additionally reverses corticosteroid-induced skin atrophy.18
Pimecrolimus was found to be a safe drug with none of the side-effects seen with topical steroids and was also found to reduce the dependency of patients on topical steroids.19 The percutaneous absorption of TCIs was found to be low. A significant proportion of patients could also be maintained without topical steroids for a year. A 12-month vehicle controlled study of children showed that early use of pimecrolimus reduced the frequency of flares, although early use of topical steroids might have shown similar benefits.20
In the UK the National Institute of Clinical Excellence approves the use of topical tacrolimus for children older than 2 years of age with moderate to severe dermatitis not controlled by TCS, and of topical pimecrolimus as a second-line option for resistant dermatitis of the head and neck.21 In the USA both of these agents are approved as second-line treatments, and the site of application is not restricted for pimecrolimus.
Tacrolimus has a favourable safety profile for up to 4 years.
Generalised herpetic and molluscum infection have been observed with TCIs but it is unclear whether there is an increased susceptibility to viral infections with TCIs. TCIs are not safe to use in pregnancy or during breastfeeding.
8.3 Antihistamines [0]
There is no clear RCT evidence to support the therapeutic value of antihistamines in the treatment of atopic eczema.22,23 Their sedative effects are useful and can be used as a short-term adjuvant to alleviate severe pruritus during acute flares.24 Non-sedating antihistamines seem to have no objective value in treating atopic eczema.25 The results of studies are conflicting thus far.26-28
8.4 Cyclosporine [3; D]
Cyclosporine is an oral calcineurin inhibitor available as 25 mg or 100 mg soft gelatin capsules. Efficacy in treating mild to moderate eczema is well established but is restricted to case reports,29 while the use of cyclosporine for the treatment of severe AD is recommended on the basis of the results of well-designed RCTs although the agent is not approved by the FDA for treating AD.1
Cyclosporine should be used on a short-term basis for severe refractory AD.30 Maximal efficacy is observed within 2 weeks, but relapses following cessation of treatment are common.31 An open study in adults found that one to two 6-week courses of cyclosporine resulted in long-term remission of atopic eczema at 1 year32 but open trials in children found that continuous rather than intermittent use achieved better control.33
The starting dose is usually 5 mg/kg daily in divided doses tapering down to 2 - 3 mg/kg daily in divided doses.34 Careful monitoring is essential with cyclosporine use. Documented side-effects include nephrotoxicity, immunosuppression, and predisposition to cancer, particularly cutaneous non-melanoma skin cancer and lymphoma. Cyclosporine also interacts with a variety of commonly used blood pressure medications, statins, antibiotics, antifungals, anti-epileptics, and HIV protease inhibitors.35,36
8.5 Azathioprine [2+; B]
Very few scientific data support its use except for two recent RCTs37,38 showing 25 - 37% improvement in disease activity, but 15 - 35% of the participants withdrew owing to side-effects. Sustained improvement for at least 3 months after stopping azathioprine may also occur. A retrospective open study showed good or excellent response in 41/48 (85%) children with atopic eczema.39
Treatment with azathioprine as systemic monotherapy is a cost-effective adjunctive treatment in moderate to severe atopic eczema that does not respond despite optimum therapy with topical corticosteroids.40 Optimal use is achieved when combined with systemic steroids, providing a steroid-sparing effect, after determining the level of thiopurinemethyl transferase (TPMT), a key enzyme in thiopurine metabolism status.
The dose is 2.5 mg/kg/day. One can start with 50 mg a day increasing it gradually. Onset of effect is slow and therapeutic effects are not dramatic, which is discouraging to patients. Hypersensitivity reactions can occur. Long-term risks are unknown.41
8.6 Methotrexate [0]
Methotrexate is a folic acid antagonist that prevents the production of tetrahydrofolic acid by binding to dihydrofolate reductase. There are no evidence-based RCTs to support its use in AD.42,43
8.7 Mycophenolate mofetil (MMF) [3; D]
Severe refractory AD was documented to be responsive to MMF in a few trials.44-46
The standard dosage in adults appears to be 1 g orally twice daily, on an empty stomach. It is available as a 250 mg capsule. The safety profile concerning neutropenia and the development of lymphomas and other malignancies in long-term use of MMF also needs to be evaluated.47,48
8.8 Antibiotics
These drugs are often needed to treat complicating bacterial infections, especially those caused by Staphylococcus aureus. This can also help to control difficult-to-manage dermatitis. It is, however, not advisable to use long-term antibiotics to suppress growth of this organism as the disadvantages outweigh the benefits.
8.9 Antivirals
Drugs like aciclovir, valaciclovir and famciclovir are sometimes needed to treat complicating herpes simplex infections.
1. Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology. J Am Acad Dermatol 2004; 50: 391-404.
2. Korting HC, Kerscher MJ, Schafer-Korting M. Topical glucocorticoids with improved benefit/ risk ratio: do they exist? J Am Acad Dermatol 1992; 27: 87-92.
3. Sulzberger MB, Witten VH. Effect of topically applied compound in selected dermatoses. J Invest Dermatol 1952; 19: 101-102.
4. Ayres PJ, Hooper G. Assessment of the skin penetration properties of different carrier vehicles for topically applied cortisol. Br J Dermatol 1978; 99: 307-317.
5. McHenry PM, Williams HC, Bingham EA. Management of atopic eczema: Joint Workshop of the British Association of Dermatologists and the Research Unit of the Royal College of Physicians of London BMJ 1995; 310: 843-847.
6. Management of atopic eczema in primary care, Prodigy, 2004. http://www.prodigy.nhs.uk (last accessed 16 January 2007).
7. Huang X, Tanojo H, Lenn J, et al. A novel foam vehicle for delivery of topical steroids. J Am Acad Dermatol 2005; 53: S26-38.
8. Ellison JA, Patel L, Ray DW, et al. Hypothalamic-pituitary-adrenal function and glucocorticoid sensitivity in atopic dermatitis. Pediatrics 2000; 105: 794-799.
9. Sidbury R, Hanifin JM. Old, new and emerging therapies for atopic dermatitis. Dermatol Clin 2000; 18: 1-11.
10. Hengge UR, Ruzicka MD, Robert A, et al. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol 2006; 54: 1-15.
11. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid sparing therapy. J Am Acad Dermatol 2005; 53: S50-58.
12. Luger T, van Leent EJ, Graeber M, et al. SDZ ASM 981: an emerging safe and effective treatment for atopic dermatitis. Br J Dermatol 2001; 144: 788-794.
13. Paul C, Cork M, Rossi AB, et al. Safety and tolerability of 1% pimecrolimus cream among infants. Pediatrics 2006; 117: 118-128.
14. Breuer K, Werfel T, Kapp A. Safety and efficacy of topical calcineurin inhibitors in the treatment of childhood eczema. Am J Clin Dermatol 2005; 6: 65-77.
15. Ashcroft DM, Dimmock P, Garside R, et al. Efficacy and tolerability of topical pimecrolimus and tacrolimus in the treatment of atopic dermatitis: meta-analysis of randomized controlled trials. BMJ 2005; 330: 516-522.
16. Kempers S, Boguniewicz M, Carter E, et al. A randomized investigator-blinded study comparing pimecrolimus cream with tacrolimus in the treatment of pediatric patients with moderate atopic dermatitis. J Am Acad Dermatol 2004; 51: 515-525.
17. Queille-Roussel C, Paul C, Duteil L, et al. The new topical ascomycin derivate SDZ ASM 981 does not induce skin atrophy. Br J Dermatol 2001; 144: 507-513.
18. Kyllonen H , Remitz A, Mandelin JM, et al. Effects of 1 year intermittent treatment with topical tacrolimus monotherapy on skin collagen synthesis in patients with atopic dermatitis. Br J Dermatol 2004; 150: 1174-1181.
19. Luger TA, Lahfa R, Folster-Holst R, et al. Long term safety and tolerability of pimecrolimus cream 1% and topical steroids in adults with moderate to severe atopic dermatitis. Journal of Dermatological Treatment 2004; 15: 169-178.
20. Wahn U, Bos JD, Goodfield M, et al. Efficacy and safety of pimecrolimus cream in the long term management of atopic dermatitis in children. Pediatrics 2002; 110: 2.
21. National Institute for Clinical Excellence. Final appraisal determination: tacrolimus and pimecrolimus for atopic eczema. http://www.nice.org.uk/pdf/P&TFAD.Pdf (last accessed 16 January 2007).
22. Klein P, Clark R. An evidence-based review of the efficacy of antihistamines in relieving pruritus in atopic dermatitis. Arch Dermatol 1999; 135: 1522-1525.
23. Munday J, Bloomfield R, Goldman M, et al. Chlorpheniramine is no more effective than placebo in relieving the symptoms of childhood atopic dermatitis with a nocturnal itching and scratching component. Dermatology 2002; 205: 40-45.
24. Kawashima M, Tango T, Noguchi T, et al. Addition of fexofenadine to a topical steroid reduces the pruritus associated with atopic dermatitis in a 1 week randomized, multicenter, double-blind, placebo-controlled parallel-group study. Br J Dermatol 2003; 148: 1212-1221.
25. Wahlgren CF, Hagermark O, Bergstrom R. The antipruritic effect of a sedative and a non-sedative antihistamine in atopic dermatitis. Br J Dermatol 1990; 122: 545-551.
26. Langelnd T, Fagertun HE, Larsen S. Therapeutic effect of loratadine on pruritus inpatients with atopic dermatitis. Allergy 1994; 49: 22-26.
27. Berth-Jones J, Graham-Brown RA. Failure of terfenadine in relieving the pruritus of atopic dermatitis. Br J Dermatol 1989; 121: 635-637.
28. Doherty V, Sylvester DG, Kennedy CT, et al. Treatment of itching in atopic eczema with antihistamines with a low sedative profile. BMJ 1989; 298: 96.
29. Leung DY, Bieber T. Atopic dermatitis. Lancet 2003; 361; 151-160.
30. Naeyaert JM, Lachapelle JM, Degreef H, et al. Cyclosporine in atopic dermatitis, review of the literature and outline of a Belgian consensus. Dermatology 1999; 198: 142-152.
31. Granlund H, Erkko P, Sinasalo M. Cyclosporin in atopic dermatitis: time to relapse and effect of intermittent therapy. Br J Dermatol 1995; 132: 106-112.
32. Grandlund H, Erkko P, Reitamo S. Long term follow up of eczema patients treated with cyclosporine. Acta Derm Venerol 1998; 78:40-43.
33. Harper JI, Ahmed I, Barclay G, et al. Cyclosporin for severe childhood atopic dermatitis. Short course versus continuous therapy. Br J Dermatol 2000; 142: 52-58.
34. Sowden JM, Berth-Jones J, Ross JS, et al. Double-blind, controlled, crossover study of cyclosporine in adults with severe refractory atopic dermatitis. Lancet 1991; 338: 137-140.
35. Thompson PD, Clarkson P, Karas RH. Statin associated myopathy. J Am Med Assoc 2003; 289:1681-1690.
36. Akhavan A, Rudikoff D. The treatment of atopic dermatitis with systemic immunosuppressive agents. Clin Dermatol 2003; 21: 225-240.
37. Berth-Jones J, Takwale A, Tan E, et al. Azathioprine in severe adult atopic eczema; a double blind, placebo controlled, crossover trial. Br J Dermatol 2002; 147: 324-330.
38. Meggitt SJ, Gray JC, Reynolds NJ. Azathioprine dosed by thiopurine methyltransferase activity for moderate to severe atopic eczema: a double-blind, randomized controlled trial. Lancet 2006; 367: 839-846.
39. Murphy LA, Atherton D. A retrospective evaluation of azathioprine in severe childhood atopic eczema using TPMT levels to exclude patients at high risk of myelosuppression. Br J Dermatol 2002; 147: 308-315.
40. Buckley DA, Baldwin P, Rogers S. The use of azathioprine in severe adult atopic eczema. J Eur Acad Dermatol Venereol 1998; 11: 137-140.
41. Kwon JH, Farrel RJ. The risk of lymphoma in the treatment of inflammatory bowel disease with immunosuppressive agents. Crt Rev Clin Oncol 2005; 56: 169-178.
42. Egan CA, Rallis TM , Meadows KP. Low dose oral methotrexate treatment for recalcitrant palmoplantar pompholyx. J Am Acad Dermatol 1999; 40: 612-614.
43. Shaffrali FC, Colver GB, Messenger AG. Experience with low dose methotrexate for the treatment of eczema in the elderly J Am Acad Dermatol 2003; 48: 417-419.
44. Neuber K, Schwartz I, Itschert G. Treatment of atopic eczema with oral mycophenylate mofetil. Br J Dermatol 2000; 143: 385-391.
45. Grundmann-Kollman M, Podda M, Ochsendorf F. Mycophenolate mofetil is effective in the treatment of atopic dermatitis. Arch Dermatol 2001; 137: 870-873.
46. Murray ML, Cohen JB. Mycophenolate mofetil therapy for moderate to severe atopic dermatitis. Clin Exp Dermatol 2006; 2: 1-5.
47. Stern DK, Tripp JM, Ho VC, Lebwohl M. Use of systemic immune modulators in dermatology an update. Dermatol Clin 2005; 23: 259-300.
48. Heymann WR. Mycophenolate mofetil. J Am Acad Dermatol 2005; 53: 1045-1046.
9. Complementary/alternative therapies
The use of these modalities has become very popular,1 which is understandable when people are faced with an intractable, incurable, highly symptomatic condition for which conventional medicine seems to be only partially beneficial. These treatments can be defined as forms of therapy that involve any treatment method without scientific proof of adequate or superior efficacy compared with conventional treatment.2 Approximately 30% of patients with allergies report the use of complementary treatments in Europe; these tend to be younger women with higher educational background.3 Traditional healers in Africa probably treat large numbers of patients with atopic dermatitis (AD), but no reliable figures or records of treatment methods exist for this group of patients.
9.1 Phytotherapy
9.1.1 Chinese herbal medicine (CHM) [1-; C]
Conflicting evidence exists regarding the efficacy and toxicity of these medicines, probably because there is a big variation in the actual composition of the different products used by different practitioners.4,5 Some preparations illegally contain potent topical corticosteroids.6 One meta-analysis7 showed that there might be some evidence of efficacy in reducing symptoms. Close monitoring of hepatic and renal function is necessary and treatment is contraindicated in pregnancy and in patients with pre-existing liver, renal and cardiac disease.
9.1.2 Kampo (Japanese herbal medicine) [3; D]
These treatments include composite herbs like Zemaphyte, Shofu-san, Ji-zuso-ippo, Eppi-ka-jutsu-to and Hochu-ekki-to. 'Kampo and diet' has been proposed as second-line treatment for AD in cases where first-line conventional treatment has failed, as first-line therapy with Kampo is no more effective than standard treatment. It should, according to the authors, be tried before immunosuppressives are introduced.8,9
9.1.3 Tea tree oil [0]
No controlled trials to prove efficacy in AD have been done. Allergic contact dermatitis is a frequent complication, mainly due to the sesquiterpine content.10
9.1.4 Essential fatty acids [1++; 0]
No benefit could be demonstrated in one excellent meta-analysis11 of 34 qualifying publications. There are therefore no grounds for the use of these preparations. A single study using hempseed oil done after publication of the meta-analysis did show some benefit, presumed to be due to its effect on essential fatty acid metabolism.12
9.1.5 Kiwi fruit extract [2-; D]
A single study showed some benefit in improving some signs, but not symptoms, in 51 adults.13
9.1.6 Other herbal medicine [0]
No evidence exists to support the use of arnica, calendula flos and German chamomile.
9.2 Homeopathy [0]
No evidence for efficacy exists, as no valid clinical studies have been reported.
9.3 Hypnotherapy [2-; D]
Evidence supporting its use is weak, but some studies show promising results.14,15
9.4 Stress management [2-; D]
9.5 Topical streptococcal preparation [3; D]
One uncontrolled, open trial showed complete 'cure' in four cases.16
9.6 Massage therapy [2-; D]
One study reported symptomatic improvement with this method, with massage alone, but the addition of a series of essential oils to the massage oils (aromatherapy) brought no additional benefits.17
9.7 Reiki [0]
No studies to support the use of this modality in AD could be found. The reasoning behind this treatment has been published.18
9.8 Autologous blood therapy [2-; D]
One controlled study showed some improvement over placebo.19
9.9 Other complementary therapies without proven efficacy
Acupuncture,20 Bioresonance treatment,21 balneotherapy and cleansing of the colon with enemas fall into this group. Sublingual immunotherapy has shown some promising provisional results in respiratory allergies, but no evidence exists for efficacy in dermatitis.22
9.10 interactions between herbs and conventional medicine
The blood levels of anticonvulsant treatment need to be checked and the dosages increased when evening primrose oil (gamolinolenic acid) is administered, because epilepsy can become unstable. Hepatitis can be induced by CHM and echinacea and it can potentiate the hepatic toxicity of drugs like methotrexate.23 The effectiveness of immunosuppressants can be reduced by the concomitant use of zinc, echinacea and vitamin E.24
9.11 Complementary and alternative allergy tests
Several of these tests are done regularly, but none has any scientific foundation or proof of validity.25 These include: the leucocytotoxic test; the IgG ELISA allergy test; applied kinesiology; electrodermal testing; hair analysis; auriculocardiac reflex; Nampudripad's allergy elimination technique; live blood analysis and stool analysis and microscopy for yeasts and parasites.
10. General approach to the treatment of atopic dermatitis
1. Jensen P. Use of alternative medicine by patients with atopic dermatitis and psoriasis. Acta Dermatol Venereol 1990; 70: 421-424.
2. Artik S, Ruzicka T. Complementary therapy for atopic eczema and other allergic skin diseases. Dermatological Therapy 2003; 16: 150-163.
3. Schafer T. Epidemiology of complementary alternative medicine for asthma and allergy in Europe and Germany. Ann Allergy Asthma Immunology 2004; 93: suppl 1, S5-10.
4. Koo J, Arain S. Traditional Chinese medicine for the treatment of dermatological disorders. Arch Dermatol 1998; 134: 1388-1393.
5. Ferguson JE, Chalmers RJG, Rowlands DJ. Reversible dilated cardiomyopathy following treatment of atopic eczema with Chinese herbal medicine. Br J Dermatol 1997; 136: 592-593.
6. Ramsay HM, Goddard W, Gill S, Moss C. Herbal creams used for atopic eczema in Birmingham, UK, illegally contain potent corticosteroids. Arch Dis Child 2003; 88: 1056-1057.
7. Zhang W, Leonard T, Bath-Hextall F, et al. Chinese herbal medicine for atopic eczema. Cochrane Database Syst Rev 2004; 4: CD002291:1-22.
8. Kobayashi H, Takahashi K, Mizuno N, Kutsuna H, Ishii M. An alternative approach to atopic dermatitis: Part I - Case series presentation. Evidence Based Complementary and Alternative Medicine 2004; 1: 49-62.
9. Kobayashi H, Takahashi K, Mizuno N, Kutsuna H, Ishii M. An alternative approach to atopic dermatitis: Part II - Summary of cases and discussion. Evidence Based Complementary and Alternative Medicine 2004; 1: 145-155.
10. Bedi MK, Shenefeldt PD. Herbal therapy in dermatology. Arch Dermatol 2002; 138: 232-242.
11. Van Gool CJAW, Zeegers MPA, Thijs C. Oral essential fatty acid supplementation in atopic dermatitis - a meta-analysis of placebo-controlled trials. Br J Dermatol 2004; 150: 728-740.
12. Callaway J, Schwab U, Harvima I, et al. Efficacy of dietary hempseed oil in patients with atopic dermatitis. Journal of Dermatological Treatment 2005; 16: 87-94.
13. Mraz S, Miller B, Bocko A, Tschen E. A multicenter, double-blind, placebo-controlled study of the effectiveness of kiwi-fruit extract in adults with atopic dermatitis of moderate severity. J Am Acad Dermatol 2006; 54: AB3.
14. Stewart AC, Thomas SE. Hypnotherapy as a treatment for atopic dermatitis in adults and children. Br J Dermatol 1995; 132: 778-783.
15. Baron S, Layton A, Goulden V. A pilot study of hypnotherapy to treat adults and children with moderate to severe atopic dermatitis. J Am Acad Dermatol 2006; 54: AB2.
16. Horiuchi Y. Topical Streptococcal preparation, OK-432, for atopic dermatitis. Journal of Dermatological Treatment 2005; 16: 117-120.
17. Anderson C, Lis-Balchin M, Kirk-Smith M. Evaluation of massage with essential oils on childhood atopic eczema. Phytother Res 2000; 14: 452-456.
18. Nield-Anderson L, Ameling A. The empowering nature of Reiki as a complementary therapy. Holistic Nursing Practice 2000; 14: 21-29.
19. Pittler MH, Armstrong NC, Cox A, Collier PM, Hart A, Ernst E. Randomized, double-blind, placebo-controlled trial of autologous blood therapy for atopic dermatitis. Br J Dermatol 2003; 148: 307-313.
20. Koo J, Arain S. Traditional Chinese medicine for the treatment of dermatological disorders. Arch Dermatol 1998; 134: 1388-1393.
21. Schoni MH, Nicolaizik WH, Schoni-Affofter F. Efficacy trial of bioresonance in children with atopic dermatitis. Int Arch Allergy Immunol 1997; 112: 238-246.
22. Pajno GB, Barberio G, Boner AL. Efficacy of sublingual immunotherapy in asthma and eczema. Chem Immunol Allergy 2003; 82: 77-88.
23. Ferguson JE, Chalmers RJG, Rowlands DJ. Reversible dilated cardiomyopathy following treatment of atopic eczema with Chinese herbal medicine. Br J Dermatol 1997; 136: 592-593.
24. Miller LG. Herbal medicinals. Arch Intern Med 1998; 158: 2200-2208.
25. Morris, A. Complementary and alternative allergy tests. Current Allergy & Clinical Immunology 2006; 19: 26-28.
10.1 Mild dermatitis
- Appropriate general measures
- Emollients
- Topical corticosteroids
- Topical calcineurin inhibitors as second line or where corticosteroids are contraindicated.
10.2 Moderate dermatitis
- Appropriate general measures
- Emollients
- Potent topical corticosteroids for flares
- Topical calcineurin inhibitors as maintenance
- Sedating antihistamines.
10.3 Severe dermatitis
- Appropriate general measures
- Emollients
- Topical corticosteroids.
10.3.1 Acute flares
- Systemic corticosteroids (short courses)
- Topical corticosteroids in hospital
- Sedating antihistamines
- Thereafter maintenance as for chronic disease.
10.3.2 Chronic disease
- UV light
- Non-steroidal systemic drugs: azathioprine, cyclosporine, methotrexate, mycophenylate.
The general approach to the treatment of atopic dermatitis can be presented schematically (Fig. 1).
 Correspondence:
Correspondence:
W Sinclair
(sinclaiw@fshealth.gov.za)














