Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.4 Pretoria abr. 2008
ORIGINAL ARTICLES
A review of internal medicine re-admissions in a peri-urban South African hospital
A StanleyI; N GrahamII; A ParrishII
IMB ChB. Department of Medicine, Groote Schuur Hospital, Cape Town
IIMB ChB. Department of Medicine, Cecilia Makiwane Hospital, East London
IIMB ChB, FCP. Department of Medicine, Cecilia Makiwane Hospital, East London
ABSTRACT
OBJECTIVE. To measure the re-admission rate and the number of preventable re-admissions in a secondary-level South African hospital, and to identify factors predictive of re-admission.
METHOD: The admission register for the medical wards at Cecilia Makiwane Hospital (CMH) was used to identify re-admitted patients, whose folders were then reviewed. A comparison group of patients who were not re-admitted was randomly generated from the same register.
RESULTS: The re-admission rate for the 7 months ending October 2006 was 8.5% (262/3 083). Patients who were more likely to be re-admitted had chronic respiratory disease (odds ratio (OR) 4.2, 95% confidence interval (CI) 1.2 - 14.6), HIV infection (OR 5.0, CI 2.1 - 12.0), were older than 50 years (OR 5.2, CI 2.5 - 10.9), had a first admission of more than 8 days (OR 3.2, CI 1.5 - 6.6) or a booked medical outpatients follow-up (OR 5.1, CI 2.6 - 10.3). Age distribution of re-admissions was bimodal, with HIV-positive individuals (27.4% overall) accounting for 50% of all admissions younger than 50 years, but only 9.1% of those 50 years or older. In individuals older than 50 years, 42.1% of admissions were due to chronic cardiorespiratory illnesses. Half of re-admissions were judged to be potentially preventable, mainly through improved patient education.
CONCLUSION: One in 12 general medical patients was readmitted. Chronic diseases and inadequate patient education and discharge planning accounted for the largest group of re-admissions in older patients. Re-admission of HIV/AIDS patients has generated a second peak in younger individuals, and the impact of the antiretroviral roll-out on admission rates warrants further scrutiny.
Many South African hospitals experience bed shortages exacerbated by the HIV epidemic, and re-admission rates serve as a potential marker of inefficiencies in the overall system. Premature discharge before adequate assessment or stabilisation leads to higher re-admission rates, unexpected mortality in recently discharged patients, and unnecessary morbidity in patients who cope at home but who could be managed more efficiently in hospital. In many state hospitals, this problem is worsened by rapid staff turnover, so that a pool of medical officers experienced in recognising 'at risk' patients never fully develops.
Re-admission of patients to hospital accounts for 5 - 29% of overall admissions, in studies from the UK and USA.1 This results in extra clinical and administrative work, increases health care costs, and can lead to increased morbidity and mortality. In the USA, the savings that resulted from a 25% decrease in the re-admission rate for congestive cardiac failure was estimated at $424 million annually, after deducting the cost of the programmes used.2 Several studies have shown that even costly follow-up programmes designed to reduce re-admissions can result in significant savings.2,3 These studies used mainly formalised discharge planning and social support interventions.2-6 One study looked at the effect of a 1-hour, nurse-directed education session about cardiac failure and found that it significantly reduced re-admission rates and overall costs.4 The same American and British studies failed to demonstrate that improved clinical management, as opposed to discharge planning, reduced re-admission rates.5
These studies were conducted in well-resourced centres in Europe and North America and focused on chronic diseases such as heart failure, diabetes, schizophrenia and ischaemic heart disease. There is little information on HIV/AIDS and re-admission rates. Two articles examined the risk factors associated with re-admission in HIV-positive patients with pneumonia and found that leaving hospital unaccompanied, recreational drug use, living in poor social circumstances and HIV-related co-morbidities were all associated with re-admission.9,10 One study found that highly active antiretroviral therapy (HAART) was associated with lower re-admission rates.6
The roles of patient anxiety, optimism and perceived health on re-admission have also been examined. An optimistic attitude after coronary bypass surgery predicted a lower re-admission rate,7 and similar findings have been reported in relation to perceived health status and anxiety with congestive cardiac failure (CCF) and chronic obstructive pulmonary disease (COPD).8,9
Effective and comprehensive discharge procedures, combined with simple patient education, are potentially the most cost-effective ways to reduce re-admissions and duplication of work. Despite these factors, there is little published evidence on re-admission rates, the causes of re-admissions, or their prevention in South Africa. We attempted to quantify the re-admission rate and to define modifiable factors contributing to this rate as part of a focused review of admissions in the Department of Medicine at the Cecilia Makiwane Hospital (CMH).
Methods
Sample and setting
The 750-bed Cecilia Makiwane Hospital serves a peri-urban and rural population of about 1.5 million people in the Eastern Cape Province of South Africa. The Department of Medicine has 160 beds and admits an average of 13 patients per day.
The sample consisted of all re-admissions to the Department of Medicine at CMH between 1 April 2006 and 31 October 2006.
Folder numbers were captured from the medical ward admission registers, and a spreadsheet was used to search for duplications occurring between April and October 2006. These folders were identified as potential re-admissions and were retrieved for examination. Folders were excluded if either admission fell outside of the 7-month study period. Re-admissions were defined as any patient with two or more admissions within the 7-month study period as confirmed by case records and discharge summaries in the folder. Information from the discharge summaries was captured onto a summary sheet and then entered into a spreadsheet for analysis.
A comparison group was selected from the same list using a random number generator. Folders from this list were excluded if the admission fell outside the study period, if the patient died during the same admission, or if the patient had had a previous admission in the preceding year.
We captured basic demographic information about each patient and coded for the presence or absence of nine disease categories as well as the individual disease. Diagnostic categories consolidated similar conditions for ease of analysis. The diagnoses on the first and second admission were recorded separately, and reported rates show the diagnosis on first admission. Information about mortality, follow-up, discharge medication and the rank of the discharging doctor were also captured.
Coding disagreements were settled by consensus. Approval for the study was obtained from the hospital's ethics review board.
Data collection instrument
Data items were chosen based on factors investigated in other studies, as well as factors that we felt might influence re-admission. Clinician data reviewers were asked to make a subjective judgement about whether or not they felt that an admission was preventable. An admission was defined as preventable if it was felt that there were any correctable factors that might have prevented the re-admission.
Results
We captured a total of 3 083 admissions, of which 262 (8.5%) were thought to be re-admissions. Of these, 141 (4.6%) were confirmed re-admissions, and further analysis was conducted on these. Of the initial 262 cases, 106 (3.4%) could not be located and therefore could not be confirmed as re-admissions. Fifteen cases (0.5%) were excluded because the re-admission could not be confirmed from information available in the file.
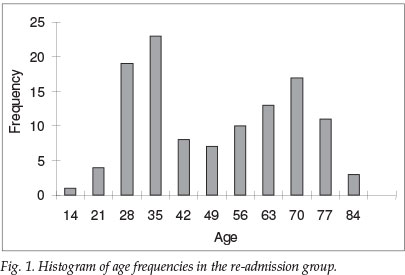
The mean age was 49.7 years with 72% female patients and 28% male. A histogram of age frequencies showed two peaks: one at 30 years and one between 55 and 65 years (Fig. 1). The mean time to re-admission was 38.4 days (standard deviation (SD) 33.54 days), and the mean length of first admission was 9.2 days (SD 8.93). Of the re-admission group, 37% had more than one diagnosis.
In the comparison group, the mean age was 43.8 years, with 62% female and 38% male patients. The average length of a single admission was 7.1 days, and 27.7% had more than one diagnosis.
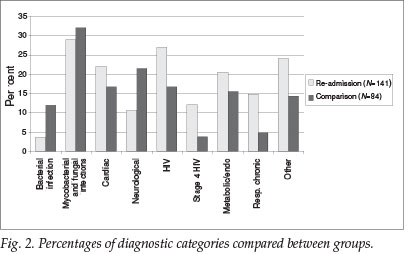
The most frequent diagnostic categories in the re-admission group were mycobacterial and fungal infections, HIV, cardiac diseases, metabolic and endocrine diseases and chronic respiratory disease (COPD and cor pulmonale) ( Fig. 2). Multiple diagnoses were present in 37.0% of patients on their first admission.
Indicators suggested by the literature as likely to predict re-admissions were compared between the re-admission group and the comparison group using logistic regression. Age, multiple diagnoses, seniority of the discharging doctor, booked medical outpatient department (MOPD) follow-up (whether or not they attended) and diagnosis on first admission (i.e. did certain diseases predict re-admission) were included. Factors found to be significant were: chronic respiratory disease (OR 4.2, 95% CI 1.2 - 14.6), HIV infection (OR 5.0, CI 2.1 - 12.0), age
Re-admitted HIV-positive patients were significantly younger (mean age 34.5 years, SD 11.8) than those who were HIV-negative (mean age 55.6, SD 21.1 years) (p< 0.001).
Using the subjective, unblinded measure as defined in the Methods section above, we felt that approximately 60% of the re-admissions were preventable. Of these, 52% were considered preventable by improved patient education and counselling. Therefore, the subjective measure found that, overall, 30% of total re-admissions might have been preventable by patient education. Management issues accounted for fewer preventable admissions: 28% of preventable admissions needed different discharge treatment, and 18% were potentially preventable by longer initial admissions.
Discussion
The re-admission rate of 4.2% is at the lower end of the range found by most of the studies that we reviewed. The percentage of possible re-admissions identified at the first stage of the study was 8.4%. It is common for CMH patients to take their folders home with them to prevent losses in filing, which means the folders would have been inaccessible for study. It is suspected that the true re-admission rate may be closer to the second figure, with the difference due to files that could not be traced.
Of the diagnostic categories, only chronic respiratory disease and HIV significantly predicted re-admission in this study. This finding is not unexpected, but the significance of other disease categories might have been missed due to a reliance on discharge summaries that have a tendency to omit diagnoses not directly related to the current admission. This might have led to HIV being under-represented in the comparison group. However, the re-admission group did have more AIDS-defining conditions (12% v. 3.7%), which suggests that the difference found in the study is accounted for by more advanced disease.
Most international studies have found that older patients tended to be re-admitted. The histogram of frequencies of age in this study shows two peaks (see Fig. 1). It is believed that the younger peak reflects the increased re-admissions in the HIV-positive population. HIV-positive patients accounted for 27% of the re-admission group, and it is many of these re-admissions that may be preventable. A Canadian study showed that HAART can reduce re-admission rates.6 The effect of HAART on re-admissions in South Africa may be more complex. Those starting HAART at more advanced stages of HIV are more likely to develop the immune reconstitution inflammatory syndrome (IRIS), especially when they are co-infected with tuberculosis.10 This is often a situation that we are faced with in South Africa, which suggests that IRIS may be more common in our population and may correspond with an increase in re-admissions. Also, patients started on HAART are likely to live longer and may therefore access health services more frequently, but this may be offset by a decrease in patients presenting with HIV-related illnesses. The impact of HAART on re-admission rates is difficult to predict, and the impact of HAART on admission and re-admission rates should be studied further in the South African context.
The more traditional peak in older age groups was also found, and this seemed to reflect admissions due to COPD and cardiac failure. This dual burden of disease increases the value of examining strategies aimed at preventing re-admissions.
Increased length of first admission was found to be linked to re-admission. This is not surprising, and may reflect more severe baseline disease.7-9 However, re-admission has also been linked to perceived ill health.6,9 Patients who perceive themselves as 'extra-sick' may spend longer in hospital and make a slower recovery. Patients' perception of their illness could also be a factor linking longer initial admission with the likelihood of re-admission.
Booked MOPD follow-up was associated with an increased re-admission rate. This finding suggests that chronic cases followed up in a hospital outpatient setting are more likely to be re-admitted. Why this should be so is unclear. These patients should be receiving optimal care and continuous education about their disease. It may be that patients judged to be at increased risk are more likely to be followed up at MOPD, and that it is therefore a marker of severity of disease. It is also possible that patients with whom OPD clinicians are more familiar are more likely to be admitted, as smaller deviations from baseline will be more readily picked up and judged as more severe.
Overall, relatively few predictive factors for re-admission could be identified. This is in keeping with the general trend found in other studies. Although our analysis was not complete in terms of physiological indicators or disease classification, it suggests that patient-related factors are important in determining re-admission. Over half of all re-admissions were judged to be preventable and, of these, half were felt to be preventable by means of better patient education. Patient education and discharge planning is not costly and, with creativity, is relatively easy to provide even in resource-poor settings. This represents a potential financial saving, as well as decreased morbidity and mortality, and increased efficiency. Further factors affecting re-admission (such as health-related quality of life, perceived ill-health, and anxiety or depression) warrant evaluation in the South African context.
We believe that CMH is representative of the average South African public sector hospital in terms of staff ratios, resource availability and population served. Our findings suggest that between 5% and 10% of admissions are re-admissions, and we believe that approximately one-third of these may be preventable by ensuring that patients understand their disease, and by proper planning for post-discharge care and support.
Limitations
We encountered a significant number of filing errors and lost folders, which might have skewed our data. The study period included mainly winter months, and this might have led to over-representation of certain conditions, especially chronic pulmonary conditions, in the sample.
The coding and analysis was unblinded and performed by the same investigators, although all disagreements or borderline cases were resolved by discussion among the authors. The assessment of whether a re-admission was preventable or not was also made on subjective grounds, but an attempt was made to standardise judgements between authors.
Our data were also based on discharge summaries, which tend to reflect only the complaint for which the patient was admitted, and not necessarily background co-morbidities. Significant diseases which might not have been directly related to admission, but which might have had an overall effect, could have been missed e.g. diabetes and hypertension.
Conclusion
Re-admissions account for a significant proportion of the workload in general medical departments. Preventing re-admissions is desirable in terms of increasing the efficiency of bed utilisation, decreasing costs and reducing morbidity. HIV/ AIDS contributes significantly to re-admissions in South Africa, especially among the young. Assessing patients for HAART as part of general medical admission and expediting treatment for those who need it may reduce re-admissions in this group; however, the impact of HAART on re-admission is likely to be complex and deserves further study. Some re-admissions are unavoidable and are linked to severity of disease, but a proportion can probably be avoided by improved patient education, counselling and support. Further research is needed to evaluate different educational interventions in a South African context.
References
1. Hasan M. Readmission of patients to hospital: Still ill defined and poorly understood. Int J Qual Health Care 2001; 13: 177-179. [ Links ]
2. Phillips CO, Wright SM, Keen DE, et al. Comprehensive discharge planning with post discharge social support for older patients with congestive cardiac failure: A meta analysis. JAMA 2004; 291(11): 1358-1367. [ Links ]
3. Parker SG. Do current discharge arrangements from inpatient hospital care reduce readmission rates, the length of inpatient stay or mortality, or improve health status? Copenhagen: WHO regional office for Europe (Health Evidence Network report) http://www.euro.who.int/Document/E87542.pdf (accessed 11 August 2006). [ Links ]
4. Naylor M, Brooten D, Jones R, et al. Comprehensive discharge planning in the hospitalized elderly: A randomized control trial. JAMA 1994; 120(12): 999-1006. [ Links ]
5. Krumholz, HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol 2002; 39:83-88. [ Links ]
6. Nikolaus T, Specht-Leible N, Bach M, et al. A randomized trial of comprehensive geriatric assessment and home intervention in the care of the hospitalized elderly. Age Ageing 1999; 28: 543-550. [ Links ]
7. Koelling TM, Johnson ML, Cody RJ, Aarnson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation 2005; 111: 179-185. [ Links ]
8. Luthi JC, Burnand B, McClellan WM, et al. Is readmission to hospital an indicator of poor quality of care for patients with heart failure? Qual Saf Health Care 2004; 13: 46-51. [ Links ]
9. Grant RW, Charlebois ED, Wachter RM. Risk factors for early hospital readmission in patients with AIDS and pneumonia. J Gen Intern Med 1999; 14: 531-536. [ Links ]
10. Palepu A, Sun H, Kuyper L, et al. Predictors of early hospital readmission in HIV-infected patients with pneumonia. J Gen Intern Med 2003; 18: 242-247. [ Links ]
11. Nosyk B, Sun H, Li X, et al. Highly active antiretroviral therapy and hospital readmission: comparison of a matched cohort. BMC Infect Dis 2006; 6: 146. [ Links ]
12. Scheier MF, Matthews KA, Owens JF, et al. Optimism and rehospitalization after coronary bypass graft surgery. Arch Intern Med 1999; 159: 829-835. [ Links ]
13. Gudmundson G, Gislason T, Janson C, et al. Risk factors for rehospitalisation in COPD: role of health status anxiety and depression. Eur Resp J 2005; 26: 414-419. [ Links ]
14. Rodriguez-Artalejo F, Guallar-Castillon P, Pascual CR. Health related quality of life as a predictor of hospital readmission and death among patients with heart failure. Arch Intern Med 2005; 165: 1274-1279. [ Links ]
15. Lawn SD, Bekker G, Miller R. Immune reconstitution disease associated with mycobacterial infections in HIV-infected individuals receiving antiretrovirals. Lancet Infect Dis 2005; 5: 361-373. [ Links ]
 Correspondence:
Correspondence:
A Stanley
(alanmstanley@yahoo.co.uk)
Accepted 15 October 2007.














