Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 no.3 Pretoria Mar. 2008
ORIGINAL ARTICLES
Messages about dual contraception in areas of high HIV prevalence are not heeded
N NgubaneI; M L NewellII; R M BlandIII; D PatelIV; H M CoovadiaV; N RollinsVI; A CoutsoudisVII
IMPH. Africa Centre for Health and Population Studies, University of KwaZulu-Natal, Durban
IIPhD. Africa Centre for Health and Population Studies, University of KwaZulu-Natal, Durban
IIIMD. Africa Centre for Health and Population Studies, University of KwaZulu-Natal, Durban
IVPhD. Centre for Paediatric Epidemiology and Biostatistics, Institute of Child Health, University College, London
VPhD. Centre for HIV/AIDS Networking, University of KwaZulu-Natal
VIMD. Department of Paediatrics and Child Health, University of KwaZulu-Natal
VIIPhD. Department of Paediatrics and Child Health, University of KwaZulu-Natal
ABSTRACT
BACKGROUND: Dual protection is recommended for prevention of unwanted pregnancies and protection against sexually transmitted infections, including HIV. It is critical for HIV-negative women to prevent seroconversion and HIV transmission to their infants during pregnancy and breastfeeding.
METHODS: Women were followed up after delivery, monthly for the first 9 months and then 3-monthly to 24 months, in a cohort study investigating postnatal HIV transmission. Study nurses discussed family planning, including condom use, at each visit. Contraceptive methods used since the last visit were recorded. All women knew their HIV status, and most women breastfed for a minimum of 6 months.
RESULTS: Among 1 137 HIV-positive and 1 220 HIV-negative women the most common contraceptive method was the hormonal injectable; few women used condoms alone or as dual contraception (0 - 3 months 6.8%; 7 - 12 months 16.3%; 19 - 24 months 14.4%). Compared with uninfected women, HIV-positive women were more likely to use condoms in years 1 and 2 after delivery (adjusted odds ratio (AOR) 1.72, 95% confidence interval (CI) 1.38 - 2.14, p<0.001; AOR 1.61, 95% CI 1.15 - 2.25, p=0.006 respectively). Compared with women with a flush toilet, those with a pit latrine were less likely to use condoms in years 1 and 2 (AOR 0.22, 95% CI 01.7 - 0.28, p<0.001; AOR 0.27, 95% CI 0.19 - 0.39, p<0.001). Older women were more likely to use condoms in the first postpartum year (AOR 1.78, 95% CI 1.03 - 3.09, p=0.040).
CONCLUSIONS: More creative ways of promoting condoms and dual contraception need to be found if new HIV infections, in women and children, are to be prevented.
South Africa is one of the countries in sub-Saharan Africa hardest hit by the HIV pandemic, with women more likely to be infected than men of the same age.1 HIV prevalence among pregnant women attending antenatal clinics has reached its highest level to date: 29.5% (95% confidence interval (CI) 28.5 - 30.5) of women were HIV positive in 2004 (95% CI 36.8 -41.4), with the prevalence reaching 40% in KwaZulu-Natal.2 While much attention is paid to reduction of vertical HIV transmission from mother to child during the antenatal period and delivery, with modified obstetric techniques and the use of antiretroviral regimens,3,4 the postpartum period is also critically important.5 Exclusive breastfeeding is recommended for the first 6 months of life for infants of HIV-negative women, and for infants of HIV-positive women who do not have the resources for safe and sustainable replacement feeding.6 It is crucial for HIV-negative women to prevent seroconversion and HIV transmission to their infant during breastfeeding.
We present data on the use of contraceptives, in particular dual protection (i.e. the use of a condom, plus another contraceptive method, to simultaneously reduce the risk of unwanted pregnancies and sexually transmitted infections (STI) including HIV), in the first 2 years after delivery, in HIV-infected and uninfected women, in an area of South Africa with a high HIV prevalence.7-9
Population and methods
The data presented here are from a non-randomised intervention cohort study examining postnatal transmission of HIV and infant feeding in KwaZulu-Natal, South Africa.10 Pregnant women were enrolled at 7 rural, 1 peri-urban, and 1 urban government clinic. All women received HIV counselling and testing from lay HIV counsellors, and all women received post-test counselling and were aware of their HIV results. Maternal sociodemographic data were recorded antenatally.
Women were followed up at clinics, postnatally, for a maximum period of 24 months: monthly for the first 9 months, and every 3 months from 10 to 24 months. At each clinic visit the mother was interviewed by a dedicated study nurse, known to the mother, who had received training in family planning, and was aware of the full medical history and HIV status of the mother. At each visit the mother was specifically asked about her contraceptive use since the last clinic visit. If more than one contraceptive method had been used during this period, all were documented. Most women opted to breastfeed for at least the first 6 months of the infant's life.11 An integrated mother and child health service, including family planning, was provided by the study nurses.
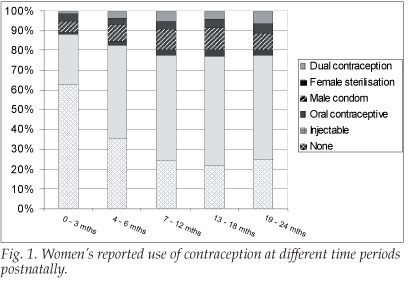
Contraceptive methods were classified as: none, injectable, oral contraception, male condom, female sterilisation or dual contraception. Contraceptive use was described over five time periods: 0 - 3, 4 - 6, 7 - 12, 13 - 18 and 19 - 24 months after delivery. The characteristics of mothers who did, or did not, use male condoms were examined over two time periods: 0 -12 and 12 - 24 months after delivery.
Data were captured using optical imaging recognition software (Teleform, Cardiff, and San Diego) into a Microsoft SQL server database. Statistical analyses used were performed using SPSS, version 13 (SPSS Inc., Chicago, Ill.). Univariable comparisons for categorical variables were assessed with a chi-square test or chi-square test for linear trend. Univariable comparisons for continuous variables were assessed using either a two-tailed unpaired t-test or the Mann-Whitney test. Determinants of condom use were assessed in a multivariable logistic regression analysis.
Results
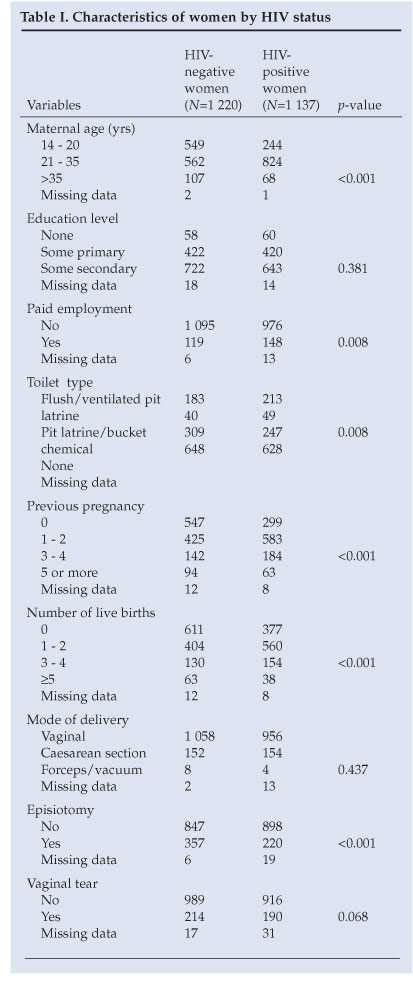
A total of 1 137 HIV-positive and 1 220 HIV-negative Zulu women were followed up postnatally. HIV-positive women were more likely to have had a previous pregnancy, have paid employment, be older and have better toilet facilities than HIV-negative women (Table I).
Injectable contraceptives were the most common method of contraception used, although a significant number of women did not use any form of contraceptive, particularly during the first 6 months after delivery (Fig. 1). Condom use in women was low, but increased during the first year from 6.8% in the period 0 - 3 months after delivery to 11.9%, 16.3%, 15% and 14.4% in the periods 4 - 6, 7 - 12, 13 - 18 and 19 - 24 months after delivery respectively.
Maternal factors associated with condom use are presented in Table II. Women who were HIV positive and those who had better toilet facilities were more likely to use condoms in both the first and second years after delivery. In addition, older women were more likely to use condoms compared with younger women in the first year after delivery.
Discussion
These results provide information about the choice of contraceptives by a large cohort of mostly rural African, women in the first 2 years after delivery. Few women used condoms, or dual contraception, despite regular counselling from the same study nurse and the ready availability of condoms at the clinics. The clinics used had a comprehensive range of family planning methods available and women could be seen at any time by the study nurse or HIV counsellor.
Furthermore, all women knew their HIV status, most women breastfed and all HIV-negative women were counselled on the risks of seroconversion during lactation. This finding is in line with other studies showing low use of condoms or dual contraception by sexually active women.12,13
A known HIV-positive status was an important determinant of condom use in this area. Interestingly, women with flush toilets, used as a proxy for socio-economic status, were also more likely to use condoms. The finding that older women were more likely to use condoms suggests that appropriate health messages about dual contraception should be designed to target younger age groups.
Many studies examining contraceptive use are cross-sectional. Strengths of this study include longitudinal follow-up of a large cohort of rural women in the postpartum period, and data on their HIV status. Limitations of this study include a lack of detailed information on the date of resumption of sexual intercourse after delivery, and no information on their current partners' HIV status. Nevertheless, it is of concern that condom use was low in all women, but particularly HIV-negative breastfeeding women. It is clear that more creative ways of promoting the use of condoms and dual contraception need to be found if postnatal HIV transmission is to be reduced and new HIV infections are to be prevented in this community.
Grant support: Wellcome Trust supported this study (Grant #063009/Z/00/2) and the Africa Centre (Grant #050534).
References
1. Pettifor A. Young people's sexual health in South Africa. HIV prevalence from nationally representative household survey. AIDS 2005; 19: 1525-1534. [ Links ]
2. Department of Health Report. National HIV and Syphilis Antenatal Sero-Prevalence Survey in Soufh Africa. 2005. http://www.doh.gov.za/docs/reports/2005/hiv.pdf (last accessed 21 September 2007). [ Links ]
3. Guay LA, Musoke P, Fleming T, ef al. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancef 1999; 354: 795-802. [ Links ]
4. Shaffer N, Chuachoowong R, Mock PA, ef al. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: a randomised controlled trial. Bangkok Collaborative Perinatal HIV Transmission Study Group. Lancef 1999; 353: 773-780. [ Links ]
5. WHO, UNICEF, UNAIDS, UNFPA. HIV Transmission through Breastfeeding: A Review of Available Evidence. Geveva: World Health Organization, 2004. [ Links ]
6. Bland R, Rollins N, Coovadia H, Coutsoudis A, Newell M. Infant feeding counselling for HIV-infected and uninfected women: appropriateness of choice and practice. Bull World Healfh Organ 2007; 85: 289-296. [ Links ]
7. De Bruin M. Living with HIV: challenges in reproductive health care in South Africa. Afr J Reprod Health 2004; 8: 92-98. [ Links ]
8. Maharaj P. Reasons for condom use among young people in KwaZulu Natal: Prevention of HIV pregnancy or both? Int Fam Plan Perspect 2006; 32(1): 28-34. [ Links ]
9. Morroni C, Smit J, McFadyen L, Mqhayi M, Beksinska M. Dual protection against sexually transmitted infections and pregnancy in South Africa. Afr J Reprod Healfh 2003; 7(2): 13-19. [ Links ]
10. Coovadia H, Rollins N, Bland R, ef al. Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding: the first six months of life. Lancef 2007; 369: 1607-1616. [ Links ]
11. Bland RM, Little KE, Coovadia HM, Coutsoudis A, Rollins NC, Newell ML. Intervention to promote exclusive breastfeeding for the first 6 months of life in a high HIV prevalence area. AIDS 2008 (in press). [ Links ]
12. Morroni C, Tibazarwa K, Myer L. Combined condom and contraceptive use among South African women. S Afr Med J 2006; 96: 620-622. [ Links ]
13. Rehle T, Shisana O, Pillay V, Zuma K, Puren A, Parker W. National HIV incidence measures - new insights into the South African epidemic. S Afr Med J 2007; 97: 194-197. [ Links ]














