Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.62 no.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00196
CASE REPORT
A rare case of adult intussusception
D RattrayI; H BrinkII
IDepartment of Surgery, Edenvale Hospital, South Africa
IIDepartment of Diagnostic Radiology, Chris Hani Baragwanath Academic Hospital, South Africa
SUMMARY
Adult intussusception is rare, and its non-specific symptoms make the diagnosis particularly difficult. Imaging modalities such as X-ray, abdominal ultrasound and multidetector computed tomography (MDCT) may improve preoperative detection. In this report, we present a 53-year-old male with an ileocaecal intussusception. The patient underwent an extended right hemicolectomy and double barrel ileocolostomy. Histopathological review of the specimen identified the lead point as an intramural caecal lymph node which, as far as we are aware, is the first time this type of lead point has been reported.
Keywords: adult intussusception, ileocaecal intussusception, lymph-node lead points
Case report
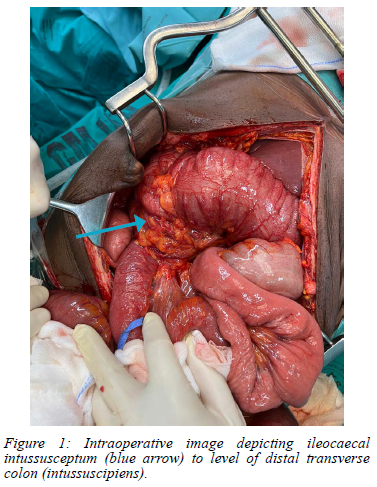
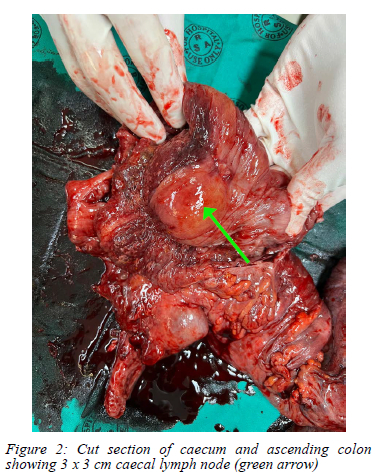
A 53-year-old male with no comorbid conditions presented with a two-week history of intermittent epigastric pain radiating to the back. The pain was associated with nausea and two episodes of vomiting consisting of normal gastric content. There was a vague history of constipation, with the passage of less frequent and smaller volume stools. He denied recent alcohol intake but admitted to consulting a traditional healer at the onset of his symptoms, who prescribed herbal medication of an unknown composition. After ingesting the herbal medication, his symptoms worsened, leading to his current presentation. On examination he did not appear acutely unwell. His vital signs were normal with a blood pressure of 117/81, heart rate of 90 beats/minute, respiratory rate of 20 breaths/minute and a temperature of 37.9°C. There was no gross distention of the abdomen which was soft with moderate tenderness in the epigastrium, right hypochondrium and right lumbar zones, and no clinical evidence of peritonism. Digital rectal examination demonstrated minimal soft brown stool and no other abnormalities. Initial venous blood gas sampling revealed a respiratory alkalosis with a pH of 7.580 (7.350-7.450), pCO2 of 25.6 mmHg (35.0-45.0) and HCO3- of 26 mmol/L ((22-29). The lactate was raised at 3.3 mmol/L (0.4-0.8) and he had multiple electrolyte abnormalities; notably hyponatraemia of 131mmol/L (136-145), hypochloraemia of 89mmol/L (98-107), hypocalcaemia of 1.10mmol/L (1.15-1.33) and mild pre-renal dysfunction with a urea of 8.9 mmol/L (2.1-7.1). He was biochemically jaundiced with a total bilirubin of 24 umol/L (5-21) and a conjugated fraction of 7 umol/L (0-3). The CRP was raised at 46 mg/L (< 10) but the remainder of the laboratory profile, including amylase, lipase, full blood count, paracetamol and salicylate levels were all within normal limits. The abdominal X-ray showed a non-specific bowel gas pattern with no radiographic features to suggest bowel obstruction. The patient was subsequently admitted under medical gastroenterology with a diagnosis of herbal intoxication. Over the next 24 hours worsening abdominal pain and distention developed. An abdominal CT scan demonstrated a longitudinal tubular structure with enhancing internal layers in the epigastrium, continuous with the ascending and descending colon and showing significantly thickened and oedematous bowel wall. No soft tissue lead point could be appreciated but the overall features were in keeping with an adult colo-colonic intussusception. A surgical consult was obtained after, which the patient was immediately consented and scheduled for an exploratory laparotomy. Intraoperatively, an ileocaecal intussusception was found, with the caecum and terminal ileum intussuscepted to the level of the distal transverse colon (Figure 1). Although the bowel was viable, the absence of an apparent lead point and the high risk of an underlying malignancy necessitated an extended right hemicolectomy and double barrel ileocolostomy. Cut section of the specimen revealed a 3 x 3 cm lipomatous-appearing lesion in the wall of the caecum (Figure 2). Subsequent histopathological review revealed a lymph node not associated with any underlying malignancy. While multiple cases of adult intussusception due to lymphoid hyperplasia have been documented in the literature, as far as we are aware, this is the only case of adult intussusception due to a single intramural lymph node.
Discussion
Intussusception refers to a condition where a proximal segment of bowel (intussusceptum) telescopes into the lumen of an adjacent distal segment (intussuscipiens). Most cases of intussusception (95%) occur in the paediatric population, where it is also the leading cause of bowel obstruction. Adult intussusception is exceedingly rare, accounting for only 5% of all cases of intussusception and 1% of adult bowel obstructions. While paediatric intussusception is typically idiopathic and usually secondary to enlarged lymphoid tissue following an infection, in adults almost 90% are due to a pathological lead point.1 Intussusception may occur anywhere along the gastrointestinal tract. The majority occur between mobile segments of bowel and those which are fixed retroperitoneally. It is classified into four separate sub-types according to anatomical location - entero-enteric, colo-colonic, ileocolic or ileocaecal, where the ileocaecal valve is the lead point of the intussusceptum.2,3 Entero-enteric and ileocolic intussusceptions are the most common types; approximately 80% are secondary to benign lesions such as lipomas, inflammatory lesions, Meckel's diverticula, and duplication cysts. In contrast, 65-70% of large bowel intussusceptions are due to a malignancy, usually adenocarcinoma (60%). Lipomas are the most common benign cause of colonic intussusception.1,2,4 In adults the clinical presentation is highly variable, with abdominal pain, nausea, vomiting, diarrhoea and rectal bleeding the most common acute, intermittent or chronic symptoms. Occasionally patients present with features of acute intestinal obstruction. The classic triad of colicky abdominal pain, palpable mass and red currant jelly stools commonly seen in the paediatric population is rarely seen in adults. Due to the non-specific symptoms of adult intussusception, a clinical diagnosis beyond bowel obstruction is rarely made prior to surgery.57 Plain abdominal X-rays may show signs of intestinal obstruction, while also providing information on the possible site of the obstruction. In experienced hands, abdominal ultrasound has both a high sensitivity and specificity in the detection of intussusception. Classic features include the "target" and "doughnut" signs in the transverse view and the "pseudo-kidney" sign in the longitudinal view. Limitations of ultrasound include obscuring of images by gas-filled loops of bowel and operator dependency.7,8 Multidetector computed tomography (MDCT) has a reported accuracy of 58-100% and is now considered the imaging modality of choice in the assessment of adult intussusception. MDCT accurately confirms the presence of intussusception and provides information on the site, segments of bowel involved, extent of intussusception, as well as the presence or absence of a lead point. Furthermore, MDCT is able to detect potential complications of intussusception, such as bowel wall ischaemia with or without perforation, which may prompt expedited referral for surgical intervention. Intussusception appears as a complex soft tissue mass on MDCT - this consists of the central intussusceptum and the outer intussuscipiens separated by a layer of mesenteric fat. Image patterns vary according to the site of the intussusception, axis of the section being viewed, thickness of the bowel wall and patency of the lumen. The appearance is described as a "target" when the CT beam is perpendicular to the longitudinal axis of the intussusception, and a "sausage" when the beam is parallel or oblique. While able to distinguish the presence or absence of a lead point, due to surrounding bowel wall oedema it is often difficult to delineate distinct anatomical features of the lead point, or differentiate between a malignant or benign neoplasm.2 Surgery is considered the standard management for adult intussusception, although there is controversy regarding the exact procedure.1 While most literature supports primary en bloc resection, initial reduction and a more limited resection has also been proposed.1,7 Primary en bloc resection is indicated due to the higher incidence of malignant lead points in adult intussusception, especially in the colon, where en bloc resection is almost universally practiced.1,5,7 This approach is supported even in small bowel intussusceptions due to the difficulty in differentiating benign and malignant aetiologies preoperatively and intraoperatively as well as the increased risk of anastomotic complications due to the potential weakening and perforation of the bowel during manipulation.7
Reduction carries the theoretical risk of tumour seeding.1,7 In patients who present with small bowel intussusception post laparotomy where the lead point is due to adhesions or a suture line from a previous enterotomy, some authors advocate reduction alone, as long as the bowel is viable.5
This case report highlights the rarity of and challenges associated with the management of adult intussusception. Due to the high incidence of a malignant aetiology, en bloc resection remains the surgical management of choice; however, in very select circumstances, reduction and then resection, or even reduction alone may be considered.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Permission for the write-up and publication of this case report has been granted by the patient in the form of written and signed consent.
ORCID
D Rattray https://orcid.org/0000-0002-1597-3097
H Brink https://orcid.org/0000-0002-8359-6393
REFERENCES
1. Wang Y, Gowing S, Arena G. Adult colo-colonic intussusception caused by congenital bands: A case report and literature review. Int J Surg Case Rep. 2016;26:88-92. https://doi.org/10.1016/j.ijscr.2016.07.019. [ Links ]
2. Valentini V, Buquicchio GL, Galluzzo M, et al. Intussusception in adults: The role of MDCT in the identification of the site and cause of obstruction. Gastroenterol Res Pract [Internet]. 2016 [cited 2023 Aug 1];2016:5623718. https://doi.org/10.1155/2016/5623718. [ Links ]
3. Amoruso M, D'Abbicco D, Praino S, Conversano A, Margari A. Idiopathic adult colo-colonic intussusception: Case report and review of the literature. Int J Surg Case Rep. 2013;4(4):416-8. https://doi.org/10.1016/jijscr.2013.01.010 [ Links ]
4. Howard N, Pranesh N, Carter P. Colo-colonic intusussception secondary to a lipoma. Int J Surg Case Rep. 2012;3(2):52-4. https://doi.org/10.1016/j.ijscr.2011.10.011. [ Links ]
5. Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226(2):134-8. https://doi.org/10.1097/00000658-199708000-00003. [ Links ]
6. Khan MN, Agrawal A, Strauss P. Ileocolic Intussusception: A rare cause of acute intestinal obstruction in adults; case report and literature review. World J Emerg Surg. 2008;3(1):26. https://doi.org/10.1186/1749-7922-3-26. [ Links ]
7. Yakan S, Caliskan C, Makay O, Denecli AG, Korkut MA. Intussusception in adults: Clinical characteristics, diagnosis and operative strategies. World J Gastroenterol. 2009;15(16):1985-9. https://doi.org/10.3748/wjg.15.1985. [ Links ]
8. Kim JH, Lee KM, Yun SH, et al. Ileocaecal intussusception in an adult: a case report. Turk J Gastroenterol. 2007;18(1):50-2. [ Links ]
 Correspondence:
Correspondence:
D Rattray
Email: darren.rattray@gmail.com














