Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.62 n.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00203
CASE REPORT
Breast cysticercosis - a case report
C Mabaso; W Ngwisanyi; S Nayler; C Nyatsambo; CA Benn
Department of Surgery, University of the Witwatersrand, South Africa
SUMMARY
Isolated incidences of human cysticercosis have been reported world-wide, but it remains a major public health concern in endemic areas such as Mexico, Africa, South-East Asia, Eastern Europe, and South America. Cysticercosis most commonly involves the skeletal muscle, subcutaneous tissue, brain, and eyes. The breast is an uncommon site of presentation for cysticercosis. Due to its rare occurrence, breast cysticercosis is often initially mistaken for other common breast lesions such as cysts, abscess, malignant tumours and fibroadenomas. We report a case of breast cysticercosis in a young South African woman.
Keywords: breast cysticercosis, tape worm, parasitic, rare
Case report
A 38-year-old female presented with a history of a painless lump in the left breast that she had discovered three weeks prior. She had no constitutional symptoms such as fever, weight loss and/or night sweats. There was no history of nipple discharge, but she reported skin changes over and around the lump. She had no comorbid conditions, was not pregnant at the time and had no family history of breast cancer. On examination, a non-tender mobile lump was noted in the lower inner quadrant of the left breast measuring approximately 3 cm. The mass was tethered to the overlying skin, but free from the underlying chest wall. She had an enlarged lymph node in the left axilla and a clinical working diagnosis of breast cancer was made.
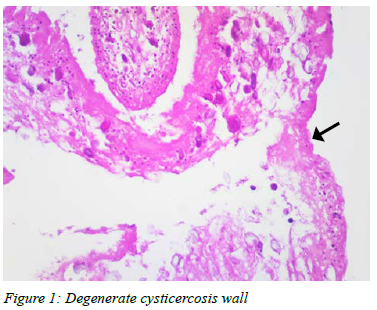
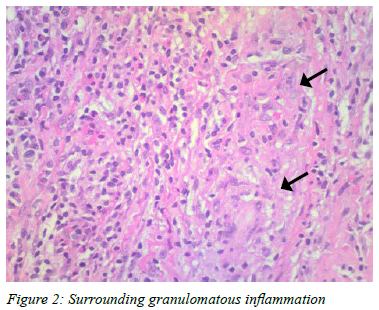
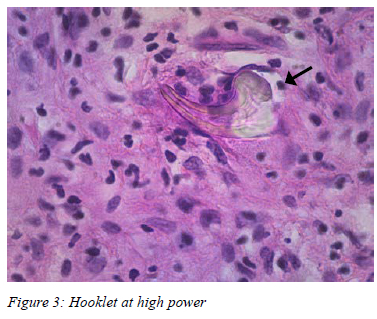
Mammogram and ultrasound of the breast showed an oval hypoechoic lesion with irregular shadowing and central necrosis in the lower inner quadrant, measuring 9.5 mm x 6.5 mm and assessed as a Breast Imaging-Reporting and Data Systems (BI-RADS) 4 lesion. Medial to this lesion, there was a smaller lesion with a cystic appearance and a thick wall measuring 6.6 mm x 6.5 mm. There was a large node in the left axillary tail measuring 18 mm with a 6 mm cortex, suspicious for infiltration. An ultrasound guided core biopsy of the breast mass and lymph node was performed. The histological examination of the breast mass showed a fragment representative of a tapeworm (cysticercal organism) in one of the cores. No evidence of malignancy was noted. The histology of the lymph node showed a reactive node. The patient underwent a wide local excision of the two lesions, which were removed as one specimen. On gross examination, the specimen was a portion of fibroadipose tissue measuring 35 x 25 x 20 mm with a central unilocular cyst containing gelatinous material. Microscopic histological examination showed a central parasitic cyst, with degenerate cysticercosis membrane (Figure 1), and a marked adjacent foreign body granulomatous response (Figure 2). Occasional hooklets consistent with cysticercosis were also noted in the wall (Figure 3). The patient was discharged postoperatively and followed up at the breast clinic where she was noted to have a completely healed wound. No anti-helminthic treatment was prescribed, and no follow-up visit was scheduled thereafter.
Discussion
Cysticercosis is caused by the larval stage of the pork tapeworm, taenia solium, which is transmitted via the faeco-oral route.1 Humans are the only definitive hosts while pigs are the intermediate hosts,2 although other domestic animals, such as cats, dogs and sheep may harbour the larvae.1 Humans usually get infected following ingestion of raw or undercooked pork that has been infected with larvae, and rarely due to consumption of food and water contaminated by the taenia solium eggs.3 The eggs make their way into the intestines where they develop into larvae. The larvae enter the bloodstream and invade host tissues, where they then complete their development into larvae called cysticerci.1 Cysticercosis poses a serious public health challenge in developing countries where there is a prevalence of poor sanitary conditions and free-ranging pigs that have access to human faeces.
Cysticerci are commonly found in the skeletal muscles, subcutaneous tissue, and the central nervous system.4 Presentation in the breast, as in the case of our patient is a very rare finding and often made incidentally. There have been 19 case reports discussing cysticercosis of the breast; three case reports from Africa (Nigeria and Madagascar) and none from South Africa.2 Cysticercosis usually presents as a cyst, and the clinical features largely depend on the location of the cyst(s), number of cysts and the host immune response.5 Subcutaneous lesions often present as painless or painful nodules, while intramuscular cysts may present as myalgia, a mass, pseudo tumour or pseudohypertrophy.6 According to the limited literature pertaining to breast cysticercosis, these lesions, as in this case, usually present with a lump which can be either painful or painless.6 Typically, as illustrated by our case, there are no other clinical features on history or physical examination that point to cysticercosis as the diagnosis.
Thus, the clinical diagnosis of cysticercosis in unusual sites such as the breast is very difficult. In most cases a definitive diagnosis is made through histological examination of the surgically removed tissue, which typically shows features of parasitic infection.7 In our case, the final histopathological examination of the excised tissue demonstrated part of a parasitic cyst lined by marked foreign body granulomatous response with occasional degenerate hooklets which are diagnostic of cysticercosis. Other investigations such as ultrasound and fine needle aspirates have been reported to be useful in diagnosing breast parasitic infestation.8
Due to the rare occurrence of breast cysticercosis, treatment is not standardised. Treatment modalities include the use of anti-parasitic agents such as mebendazole and/or wide local excision of the lump with a clear margin around the pathology. Co-existence of cysticerci in other sites will guide the treatment choice, thus making it very important to exclude infestation in other parts of the body.
Therefore, when confronted with breast cysticercosis, it is prudent to perform a computed tomography (CT) scan of the brain, an ophthalmic examination and send stool for microscopic examination to ensure that the patient is not harbouring cysticerci in other parts of the body. In our case, there was no clinical evidence of infection elsewhere in the body, and as a result she was only offered wide local excision as definitive treatment of the lump.
This case reports serves to emphasise that not all painless breast lumps are due to breast cancer. After excluding malignancy, clinicians need to be cognizant that, although rare, infectious organisms may be the cause of a breast lump. The clinical setting and knowledge of the local water and sanitation situation allow the clinician to consider a condition such as breast cysticercosis as part of their differential diagnosis.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval was obtained from the Netcare Research Operations Committee (Approval number: TRIAL-2021-0048 Renewal letter for TRIAL-2017-0035S).
ORCID
C Mabasohttps://orcid.org/0000-0003-1942-3356
W Ngwisanyi https://orcid.org/0000-0002-7675-6360
SJ Nayler https://orcid.org/0000-0002-5041-7811
C Nyatsambo https://orcid.org/0000-0002-1462-0695
CA Benn https://orcid.org/0000-0002-4777-4316
REFERENCES
1. Agarwal A, Osman MT. Cysticercosis of breast presenting as fibroadenoma. Asian J Pharm Clin Res. 2016;9(2):9-10. https://doi.org/10.22159/ajpcr.2016.v9s2.13654. [ Links ]
2. Dalal S, Sattibabu V, Bakshi V, Bhatia C. Cysticercosis of breast mimicking fibroadenoma. J Case Rep. 2016;6(2):172-4. https://doi.org/10.17659/01.2016.0042. [ Links ]
3. Bhattacharjee HK, Ramman TR, Agarwal L, Nain M, Thomas 5. Isolated cysticercosis of the breast masquerading as a breast tumour: report of a case and review of literature. Ann Trop Med Parasitol. 2011;105(6):455-61. https://doi.org/10.1179/1364859411Y.0000000039. [ Links ]
4. Attri A, Kumari S. Cysticercosis of breast: A rare finding. JMSCR. 2019;7(8):ISSN (p)2455-0450. https://doi.org/10.18535/jmscr/v7i8.142. [ Links ]
5. Gupta NK, Panchonia A, Jain D. Cysticercosis of breast. Trop Parasitol. 2013;3(2):148-50. https://doi.org/10.4103/2229-5070.122146. [ Links ]
6. Parakh A, Arora J, Goel R. An interesting case of a parasite in the breast tissue. 2015. Available from: https://www.eurorad.org/case/12649. [ Links ]
7. Karthikeyan TM, Manimaran D, Mrinalini VR. Cysticercus of the breast which mimicked a fibroadenoma - a rare presentation. J Clin Diagn Res. 2012;6(9):1555-6. https://doi.org/10.7860/JCDR/2012/4184.2559. [ Links ]
8. Sawhney M, Bisht S. Cysticercosis breast with rare cytological finding. Int J Curr Res. 2017;9(04):49402-3. [ Links ]
 Correspondence:
Correspondence:
C Mabaso
Email: crymabaso@gmail.com














