Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.62 no.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00205
CASE SERIES
Tuberculous mastoiditis - a case series
TK SuttleI; T ElsI; I ButlerII
IOtorhinolaryngology Department, Port Elizabeth Provincial Hospital, South Africa
IISt Georges Hospital, South Africa
SUMMARY
Tuberculous mastoiditis (TBM) is a rare form of extrapulmonary tuberculosis (TB), which may result in catastrophic complications, including mastoid and ossicle destruction, hearing loss and intracranial spread if untreated. Diagnosis is challenging due to the paucibacillary nature of extrapulmonary TB, compounded by limited theatre access for specimen retrieval, resulting in delayed diagnosis and treatment initiation. In this case series, we discuss three cases of TBM (one paediatric and two adults) who presented to the public and private healthcare sectors in the Eastern Cape in 2022, underscoring that TB does not respect socioeconomic status.
Keywords: tuberculous mastoiditis, South Africa, extrapulmonary tuberculosis
Case reports
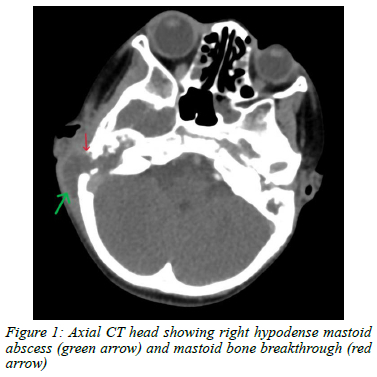
Case 1 - A 5-year-old boy presented with a 10-day history of right mastoid swelling resembling acute bacterial mastoiditis (Figure 1). Emergency abscess drainage and cortical mastoidectomy were performed, followed by definitive tympanomastoidectomy within 72 hours. Intraoperative findings included inflammatory tissue, pus, pale granulation tissue, a mesotympanic polyp and destruction of the tympanic membrane (TM), malleus and incus. Microscopy, TB and bacteriologic culture, and histology confirmed necrotising granulomatous inflammation with acid fast bacilli consistent with Mycobacterium tuberculosis. GeneXpert confirmed rifampicin sensitivity and anti-TB treatment was initiated. Within 4 months of treatment his ear was dry, the temporalis fascia tympanoplasty appeared successful, and his hearing improved from profound conductive hearing loss (CHL) to moderate CHL.
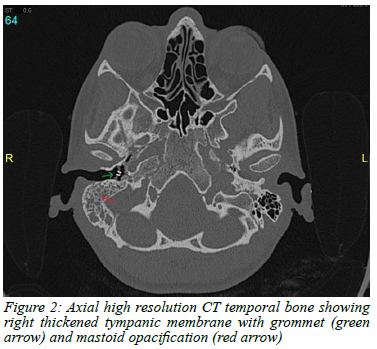
Case 2- A female in her early 20s presented with a 5-month history of right ear blockage, intermittent tinnitus and dizziness, and ipsilateral mild-to-moderate CHL (50 dB) confirmed on pure-tone audiometry (PTA). On initial presentation she had right-sided otitis media with an effusion (OME) with no symptoms suggestive of pulmonary TB and a clear chest X-ray. Her OME was treated with myringotomy and grommet insertion through a markedly thickened TM. High-resolution CT (HRCT) imaging revealed soft tissue opacification of the middle-ear cavity and mastoid antrum with slight erosion of the mastoid tegmen and a thickened, retracted TM (Figure 2). Both the ossicular chain and Prussak space appeared preserved. These findings were in keeping with chronic right otomastoiditis, rather than a cholesteatoma, and she required an exploratory tympanotomy and cortical mastoidectomy.
In theatre, pale granulation tissue and purulent secretions were found filling the middle-ear. Specimens taken confirmed Pseudomonas oryzihabitans but were negative for TB. She was treated with directed antibiotics resulting in some symptom improvement followed by worsening CHL and suppurative otitis media over the next few months.
She required a tympanomastoidectomy, which demonstrated pale granulation tissue in the antrum, epitympanum and middle-ear. This was removed and resent for bacterial, fungal and TB studies. Rifampicin sensitive TB was confirmed on polymerase chain reaction (PCR) testing, and she was initiated on a 9-month TB treatment regimen resulting in symptom improvement.
Case 3 - A woman in her late 20s presented with subacute right ear blockage and conductive hearing loss, unresponsive to multiple courses of antibiotics, steroids and nasal decongestants. On examination she had a right serous OME with an inflamed TM, which was treated with myringotomy and grommet insertion and topical fluoroquinolone ear drops. Despite topical antibiotic therapy, she had persistent suppurative otitis media. An aural pus swab was taken, and oral antibiotics were initiated. HRCT showed opacification of the right mastoid air cells, epitympanum and middle-ear suggestive of chronic otomastoiditis.
The pus swab cultured Staphylococcus aureus, which was treated successfully initially, however recurrent purulent otorrhoea and TM perforation prompted repeat sampling which confirmed rifampicin resistant TB. Pulmonary TB was excluded, and she was initiated on appropriate medical treatment. After 1 month of medical treatment, she had persistent low frequency mild to moderate (60 dB) CHL and a large TM perforation requiring a tympanomastoidectomy. Her symptoms and CHL improved with TB treatment.
Discussion
Tuberculous otitis media (TOM) and TBM account for 2.4-4% of head and neck TB cases worldwide.13 TBM is challenging to diagnose due to its paucibacillary nature and difficulty in obtaining adequate microbiologic and histologic samples.4,5 Untreated, it has potential catastrophic locoregional complications; thus requiring a high level of clinical suspicion in cases of persistent otorrhoea.3,5,6 Delayed diagnosis, particularly in paediatric patients, may result in neurodevelopmental setbacks for language, speech, hearing and social skills development.37
Despite its rarity, TOM and TBM should be considered in patients presenting with chronic otomastoiditis in both the private and public healthcare settings. Its presentation may be indistinguishable from other causes of chronic suppurative otitis media, and as TB accounts for 0.05-0.9% of chronic otitis media, diagnosis may be delayed due to a lack of suspicion.3,7,8
TOM may arise from haematogenous or lymphatic spread, direct transmission through the eustachian tube (specifically in infants consuming Mycobacterium bovis-infected milk), or direct transmission through a perforated tympanic membrane.24,7 Middle-ear infection can lead to various complications including mastoiditis, hearing loss, cranial nerve VII fallout, labyrinthine fistulas, and intracranial spread.2,3,5,7,9
Diagnosis relies on using a combination of microbiological (acid fast bacilli on Ziehl-Neelsen stains), histological and PCR testing of tissue samples, supported by HRCT imaging of the temporal bone. Typical findings of HRCT in TBM include petromastoid opacification, denuded ossicles, and bony erosion (mastoid, tegmen, facial canal, sigmoid sinus, bony labyrinth).3,5,6 Additionally, there is earlier bony erosion and intracranial spread (extradural abscess, meningitis, venous sinus thrombosis) in TBM when compared to cholesteatoma.3,5,6
According to literature, 10-50% of cases of extra-pulmonary TB have accompanying pulmonary TB, therefore part of the work-up should include plain chest X-ray and sputum testing for TB culture and PCR, which may aid in the diagnosis.10 HIV testing should also be considered as extrapulmonary TB accounts for over 50% of new TB cases in the HIV positive population.1,10 In this case series, all 3 cases were HIV negative.
A definitive TBM diagnosis requires Mycobacterium tuberculosis growth on culture, a positive PCR result or acid fast bacilli visualisation on tissue samples. In our institution, GeneXpert (PCR) has the fastest turnaround time of between 2 and 5 days, although sensitivity is only about 77%. This was evident in cases 1 and 3 where the GeneXpert was only positive on repeated tissue specimens. TB cultures have a sensitivity of 30-80%, however results take up to 8 weeks, which delays treatment.10 Diagnosis can also be made on histology showing granulomatous inflammation in association with positive Ziehl-Neelsen staining.3,10 Up to 19% of individuals with TB have negative bacteriology testing, highlighting the importance of combining clinical suspicion, laboratory testing and radiological work-up for cases of suspected TB.2
Clinical presentations may be acute (as seen in case 1) or chronic (as seen in cases 2 and 3). TBM presenting as acute mastoiditis with mastoid abscess, fistula or intracranial complications has been described mainly in paediatric cases.3,9 Similarly, our paediatric case of TBM presented with acute onset mastoiditis complicated by destruction of the posterior ear canal and ossicles. Contrary to this, our adult patients both presented with the more 'classic' persistent suppurative otitis media. This may suggest that the presentation of TOM and TBM in adults differs from that in children, however more research is needed in this area.
The duration of undiagnosed TBM is linked to the risk of intracranial spread and the severity of hearing loss, which can also result from anti-TB medications.3,5,7,10 Therefore, audiologic monitoring is important throughout TB treatment. The risk of drug-related ototoxicity further underscores the need for early confirmation of TBM and avoidance of unsolicited empiric treatment. However, in cases where the clinical and radiological suspicion is high, empiric treatment should not be withheld while awaiting microbiological confirmation.4,5,10
Most guidelines advocate 6 months of standard anti-TB medication for extrapulmonary TB; however, a prolonged course of 9-12 months is recommended for TB meningitis and TB involving bones and joints.10 Although guidelines recommend basing treatment duration on a negative PCR result, the PCR can remain positive for up to 1 year post successful treatment in certain cases.10
In the case of TOM and TBM, adequate tissue sampling to monitor response to medication would require repeated biopsies in theatre. More research is needed to confirm whether a prolonged treatment regimen is indicated in cases of TBM. Treatment for up to 9 months is recommended for rifampicin sensitive TBM due to the petromastoid bony involvement.10
Key learning points
• TBM is paucibacillary in nature and therefore tissue samples sent in a clinic setting have a low sensitivity. This is particularly challenging in the South African setting, where access to theatre may be limited.
• In cases of persistent suppurative otorrhoea and children presenting with acute bacterial mastoiditis, a high index of suspicion for underlying TOM and TBM is required in both the private and public healthcare settings.
• Up to 19% of individuals with TB have negative bacteriology testing, highlighting the importance of combining clinical suspicion, laboratory testing and radiological work-up for cases of suspected TB.
• The risk of locoregional complications, including hearing loss, are associated with the duration that TBM remains undiagnosed and untreated.
• Audiological monitoring throughout TB treatment is needed due to both the destructive nature of TBM, as well as the ototoxicity associated with anti-TB medication.
Consent
Informed consent for the publication of this case series, along with images, blood results and histological diagnosis was taken from the patients and primary caregiver when the patient was too young to give informed consent (< 18 years).
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
ORCID
TK Suttle https://orcid.org/0000-0002-4670-5562
T Els https://orcid.org/0000-0002-4558-8202
I Butler https://orcid.org/0000-0002-3139-4722
REFERENCES
1. World Health Organization. Global tuberculosis report [Internet]. Geneva; 2022 [cited 2023 Jan 3]. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022. [ Links ]
2. Hale RG, Tucker DI. Head and neck manifestations of tuberculosis. Oral Maxillofac Surg Clin North Am. 2008;20(4):635-42. https://doi.org/10.1016/j.coms.2008.06.006. [ Links ]
3. Din TF, Fagan JJ, Peer S. Profile of paediatric tuberculosis mastoiditis: a case series. S Afr J Surg. 2022;60(1):62-6. [ Links ]
4. Liktor B, Liktor B, Liktor B, et al. Primary tuberculosis of the middle ear cleft: diagnostic and therapeutic considerations. Eur Arch Otorhinolaryngol. 2014;271(7):2083-9. https://doi.org/10.1007/s00405-014-2977-7. [ Links ]
5. Jesic S, Stosic S, Milenkovic B, et al. Middle ear tuberculosis: Diagnostic criteria. Srp Arh Celok Lek. 2009;137(7-8):346-50. https://doi.org/10.2298/SARH0908346J [ Links ]
6. Kameswaran M, Natarajan K, Parthiban M, Krishnan PV, Raghunandhan S. Tuberculous otitis media: a resurgence? J Laryngol Otol. 2017;131(9):785-92. https://doi.org/10.1017/S0022215117001281. [ Links ]
7. Sebastian SK, Singhal A, Sharma A, Doloi P. Tuberculous otitis media - series of 10 cases. J Otol. 2020;15(3):95-8. https://doi.org/10.1016/jjoto.2019.12.001. [ Links ]
8. Nicolau Y, Northrop C, Eavey R. Tuberculous otitis in infants: Temporal bone histopathology and clinical extrapolation. Otol Neurotol. 2006;27(5):667-71. https://doi.org/10.1097/01.mao.0000224085.08344.50. [ Links ]
9. Jayakody N, Faoury M, Hellier W, et al. A rare presentation of a paediatric patient with acute otomastoiditis media caused by mycobacterium tuberculosis resulting in intracranial complications. J Surg Case Rep. 2019;2019(4):rjz093. https://doi.org/10.1093/jscr/rjz093. [ Links ]
10. Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015;78(2):47-55. https://doi.org/10.4046/trd.2015.78.2.47. [ Links ]
 Correspondence:
Correspondence:
TK Suttle
Email: tsuttle01@gmail.com














