Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.62 no.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00200
GENERAL SURGERY
Adult surgical admissions at a Botswana tertiary teaching hospital - spectrum, comorbidity profile, and outcomes
AG BedadaI; MJ MpaphoI; SG HamdaII
IDepartment of Surgery, Faculty of Medicine, University of Botswana, Botswana
IIDepartment of Family Medicine and Public Health, Faculty of Medicine, University of Botswana, Botswana
ABSTRACT
BACKGROUND: Documentation on the spectrum, comorbidities, profile, and outcomes of adult surgical admissions in Botswana is limited. This information may guide manpower distribution for proposed rotations in the new general surgery training programmes
METHODS: The medical records of adult surgical admissions for a period of one year (August 2017 - July 2018) were reviewed retrospectively. Demographics, types of admissions, dates of admission and discharge, and known comorbidities were captured and the outcomes were analysed
RESULTS: Of the 2610 admissions the mean age was 44.4 years and 60.8% were male. Gastrointestinal tract (GIT), neurosurgical, and cardiothoracic admissions constituted 60.7%. Emergency admissions constituted 50.1%. Comorbidities were found in 45.6% of the admissions, and HIV-prevalence was 697/1822 (38.3%) among known HIV-status patients. Elective admissions underwent more surgical procedures, 776/1303 (59.6%), p = 0.001 (COR 1.9, 95% CI:1.7-2.3). A total of 220/2610 complications (8.4%) were documented, including 42/1355 (3.1%) superficial surgical site infections and 159/2610 deaths (6.1%). Hypertension and diabetes mellitus were associated with higher mortality, p = 0.002 (COR 1.8, 95% CI:1.2-2.6) and p = 0.031 (COR 1.9, 95% CI:1.1-3.4) respectively. HIV-positive patients had longer hospital stays than HIV-negative patients, p = 0.001 (COR 1.03, 95% CI:1.02-1.04). HIV-positive admissions with CD4 count < 200 had significantly higher composite complication and mortality rate than those with > 200, p = 0.002 (COR 3.03, 95% CI:1.52-6.04) and p = 0.001 (COR 4.34, 95% CI:2.08-9.05) respectively
CONCLUSION: Contributions of emergency and elective admissions were even. A higher burden of diseases was found in gastroenterology. The higher mortalities associated with hypertension, diabetes, and CD4 count < 200 warrant further study
Keywords: comorbidities, outcomes, pattern, spectrum, surgical admissions
Introduction
Surgical care is an essential component of a functional health system that improves the health of the individuals and, hence, the economic productivity of the country.1-3 Surgical services are required in all disease categories, in all age groups, and within all levels of healthcare.1-3 One-third of the global burden of disease can be attributed to surgically-treatable conditions.1,4,5 The limited resources and capacity, economic pressure, and the burden of various illnesses increasingly challenge the health systems resulting in difficulty in the provision of safe surgical care.6 Surgical care is disproportionately scarce in regions such as sub-Saharan Africa where 93% of the population has no access to surgical care in comparison to 3.6% in high human development index countries (HHDICs).1
In HHDICs the volume of surgery and outcome are well documented.2,3 However, the spectrum and burden of surgical diseases are not well investigated in some medium-and-low human development index countries (MLHDICs).4 This includes emergency admissions and mortalities.4,7 Mortality can result from various causes including the disease process itself, some comorbidities, and complications of the procedures and anesthesia.2,3
Understanding the surgical disease spectrum, burdens, comorbidities, and outcomes helps to fill the gaps in surgical care delivery systems.7 Areas which require improvements that can be addressed by education, better practice, and policy modification can be identified in such studies.6 Hospital admission studies provide background data for surgical diseases requiring in-patient surgical care.8 The surgical care needs in MLHDICs are immense, but not well quantified.9,10 Some epidemiological research in surgical practice is based on operative data rather than surgical admissions.9
In Botswana the healthcare system includes public and private sector, catering for 85% and 15% of the population respectively. In 2018, the health budget was 4.1% of Botswana's GDP and the physician to population ratio was 3:10 000.11,12 The specialist surgical workforce in 2014 was 4 per 100 000 population. An article search conducted on 14 July 2022 returned only one paper that documented the characteristics and outcomes of trauma admissions to a hospital in Botswana.13 The aim of this study is to determine the spectrum, comorbidity, profile, and outcomes of adult surgical admissions to Princess Marina Hospital (PMH) to provide information to guide manpower distribution for proposed general surgery training programme rotations.
Materials and methods
We conducted a retrospective medical record review of all admissions to PMH from 1 August 2017 to 31 July 2018. PMH is the largest tertiary and the only teaching hospital in Botswana. The department of surgery provides surgical care in the following specialities - general surgery, urology, cardiothoracic, neurosurgery, plastic and reconstructive, and otolaryngology. All patients 13 years and older were included. The admissions were classified based on the surgical speciality and in general surgery on the sub-disciplines of breast, thyroid, gastrointestinal, hernia, skin and subcutaneous, and vascular surgery. Burn patients were included under plastics and reconstructive surgery. Eight general surgeons, three otolaryngologists, three neurosurgeons, one urologist, plastic surgeon, surgical oncologist, and cardiothoracic surgeon provided surgical care during the study period.
Data on patient demographics, type of admission, diagnosis, comorbidity, date of admission and discharge, mode of treatment, and outcomes that include complications - infections and mortality, hospital stays, discharges, and readmissions were captured. CD4 count < 200 is considered as a cutoff point for immunodeficiency. Continuous variables were described using percentages, ratios, and means. Bivariate and multivariate logistic regression analyses were employed to determine the association between independent and outcome variables - age, gender, HIV-status (HIV-negative, HIV-positive and HIV-unknown), mode of admission (emergency vs elective), comorbidities (HIV-infection, hypertension, and diabetes mellitus), and complications (infection and mortality), and CD4 counts (< 200 and > 200). Significant associations, p-value < 0.05, in bivariate logistic regression analysis were taken to multivariate analysis. Crude odds ratio (COR) and adjusted odds ratio (AOR) and 95% confidence-interval (CI) were calculated. P-value < 0.05 indicates statistical significance. The data were analysed using IBM SPSS Statistics version 27.
Results
Socio-demographics
A total of 2610 admissions were made. Males contributed 60.8% of the admissions, with a male-to-female ratio of 1.6:1. The mean average age of admission was 44.4 years - for gender specific means it was 43.5 and 45.8 years for males and females respectively. Figure 1 shows gender and age distributions of the admissions. Among females the age group 30-39 years dominated the admission, 196/1022 (19.2%), while among males the age group 20-29 years dominated the admission, 349/1588 (20.3%).
Surgical diseases pattern and burden, procedures, and comorbidities
Figure 2 shows the spectrum and burden of surgical admissions - gastrointestinal tract (GIT) admissions were the most common, 36.4%, followed by neurosurgery, 13.4%, and cardiothoracic surgery, 10.9%. Emergency admissions contributed 1307 (50.1%). The most common emergency admissions were head injury 240/1307 (18.4%), appendicitis 206/1307 (15.8%), gastrointestinal bleeding 83/1307 (6.4%), intestinal obstructions 81/1307 (6.2%), and soft tissue injuries 72/1307 (5.5%), in decreasing order of frequency.
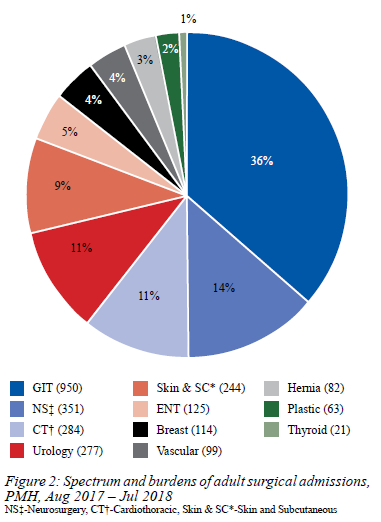
Table I shows the logistic regression analysis results of age, gender, modes of admissions, procedures, hospital stay, comorbidities, and mortality. Younger patients and male patients dominate in emergency admissions, p = 0.001 each and p = 0.001. Males contributed 683/1303 (52.4%) of elective admissions. A total of 1340 (51.3%) patients underwent procedures. Elective admissions had significantly higher rate of procedures, p = 0.001; younger patients underwent a significantly higher number of procedures, p = 0.019. There was no statistically significant difference in mortality when HIV-negative patients were compared to HIV-positive patients. In bivariate logistic regression both hypertension and diabetes were associated with higher mortality, p = 0.002 and p = 0.031 respectively, but in multivariate analysis only hypertension is significantly associated with mortality, p = 0.008.
The most common elective admissions were oesophageal cancer 95/1303 (7.3%), hernia 78/1303 (6.0%), cholelithiasis 62/1303(4.8%), and breast cancer 55/1303 (4.2%), in decreasing order of frequency. A total of 372 (14.3%) cancer admissions were made. The top four cancer admissions were oesophageal cancer 95/372 (25.5%), breast cancer 55/372 (14.8%), colorectal cancer 40/372 (10.8%), and brain cancer 33/372 (8.9%). Among the cancer patients, 155/1125 (13.8%) were HIV-negative; while 127/697 (18.2%) were HIV-positive patients; the HIV-status was unknown in the remaining 90/788 (11.4%). The three most common cancers in HIV-negative patients were oesophageal cancer 49/155 (31.6%), breast cancer 31/155 (20.0%), and colorectal cancer 17/155 (11.0%); the top four cancers in HIV-positive patients were oesophageal cancer 29/127 (22.8%), colorectal and penile cancers each 16/127 (12.6%), and breast cancer 11/127 (8.7%).
Gastrointestinal, urology, cardiothoracic, skin and subcutaneous, and neurosurgical admissions together contributed 1010/1340 (75.4%) of all procedures performed. Most patients admitted under breast, hernia, thyroid, urology, and plastic and reconstructive surgery had a higher proportion of procedures, 97/114 (85.1%), 66/82 (80.5%), 15/21 (71.4%), 173/277 (62.5%), and 35/63 (55.6%), respectively. The lowest procedure rate was for neurosurgical patients, 107/352 (30.5%).
Many of the patients had one or more pre-existing morbid conditions 1191 (45.6%) - vascular 77/99 (77.8%); thyroid 15/21 (71.4%); breast 61/114 (53.5%); plastic and reconstructive 30/63 (47.6%); and cardiothoracic 134/284 (47.2%). In the remaining 1191 patients, 1423 co-morbidities were identified. Of these, 989/1191 (83.0%) patients had one comorbidity, while 173/1191 (14.5%) had two, 28/1191 (2.4%) had three, and 1/1191 (0.1%) had four comorbidities. HIV-status was known for 1822 (69.8%) patients - 1125 (43.1%) HIV-negative and 697 (26.7%) HIV-positive.
HIV-unknown contributed 788 (30.2%). Hypertension accounted for 466/1423 (32.7%) of the comorbidities; other comorbidities include 133/1423 (9.3%) diabetes mellitus, 42/1423 (3.0%) asthma, 23/1423 (1.3%) epilepsy, 9/1423 (0.6%) psychiatric illnesses, 3/1423 (0.2%) anaemia, and 50/1423 (3.5%) others. The prevalence of hypertension in our admissions was 466 (17.9%); diabetes mellitus had a prevalence of 133 (5.1%), asthma 42 (1.6%), and anaemia 3 (0.1%).
Complications, hospital stay, discharge, and readmissions
A total of 220/2610 (8.4%) complications were documented - 159/2610 (6.1%) deaths; 42/1340 (3.1%) superficial surgical site infections; 3/1340 (2.2%) wound dehiscences, 3/2610 (0.1%) bed sores; 3/1340 (2.2%) skin flap necrosis, 3/2610 (0.1%) pneumonias; and one each acute kidney injury (0.04%), anastomotic leak 1/474 (0.2%), cholangitis 1/2610 (0.04%), hematoma 1/1340 (0.1%), necrotising fasciitis 1/2610 (0.04%), stump gangrene 1/1340 (0.1%), and hoarseness of voice following thyroidectomy1/1340 (0.1%). Surgical site infection (SSI) was documented in 6/199 (0.6%) of clean operations; while clean contaminated, contaminated, and dirty operations had SSI rates of 7/182 (3.8%), 13/133 (9.8%), and 9/32 (28.1%) respectively.
Males accounted for 113 (71.1%) of the 159 mortalities. Emergency admissions contributed 91/159 (57.2%). Emergency and elective admissions contributed 7.0% and 5.2% of the mortality, p = 0.063. Emergency admissions had a higher 24 hours mortality than elective admissions, 11/1307 (0.8%) vs 4/1303 (0.3%), p = 0.071. Gastroenterology 63 (39.6%), neurosurgery 39 (24.5%), and cardiothoracic 30 (18.9%) patients were the major contributors to mortalities. Among the mortalities 55/159 (34.6%) underwent at least one procedure. HIV, hypertension, diabetes mellitus, and epilepsy were found in 48/159 (30.2%), 43/159 (27.0%), 14/159 (8.8%), and 3/159 (1.9%) of the mortalities, respectively.
The overall mean hospital stay was 9.2 days. There was no significant difference in hospital stay among emergency and elective admissions, p = 0.276 (COR 1.0, 95% CI:0.9-1.0). The mean hospital stays were longer for burns, 28 days, and vascular admissions, 15.9 days. A total of 19 (0.7%) patients refused hospital treatment - 8 neurosurgical, 7 gastrointestinal (GIT), 2 vascular, and 1 cardiothoracic and urology each. A total of 196 (7.5%) readmissions were documented.
HIV-status known patients - HIV-negative and positive patients
Table II shows the burden of HIV-infection. Among the 1822 HIV-status known patients, HIV-positive patients constitute 697 (38.3%) - 317/797 (39.8%) females and 380/1025 (37.1%) males. The three age groups that had the highest HIV-infection rates were 41-50 years, 208/336 (61.9%), 51-60 years, 128/268 (47.8%), and 31-40 years, 159/363 (43.8%), in decreasing order.
Table III shows bivariate logistic regression analysis of known HIV-status patients and mortalities, comorbidities, and complications. Younger patients (13-65) were significantly affected by HIV-infection, p = 0.001. A significant number of HIV-negative patients were admitted on emergency bases and they had significantly higher number of procedures, p = 0.002 and p = 0.039, respectively.
In HIV-negative patients GIT, neurosurgery, and cardiothoracic pathologies contributed 37.8%, 12.4%, and 11.8%; while in HIV-positive patients GIT, cardiothoracic, and skin and subcutaneous pathologies contributed 39.7%, 12.5%, and 11.3% of the admissions. There was no significant difference in mortality among HIV-negative and HIV-positive patients, p = 0.173. HIV-positive patients had a longer hospital stay than HIV-negative patients, p = 0.001.
HIV-positive patients and CD4 counts
Table IV shows bivariate logistic regression analysis in HIV-positive patients. CD4 count was retrieved for 575/697 (82.5%) of HIV-positive patients. In 518/575 (90.1%) patients the CD4 count was >200. Among the mortalities, CD4 count was found for 42/48 (87.5%) of HIV-positive patients. HIV-positive patients with CD4 count < 200 had higher composite complication and mortality rates than those with CD4 count > 200, p = 0.002 and p = 0.001 respectively. Otherwise, no statistically significant difference was observed in the two groups regarding age, gender, mode of admissions, procedures, comorbidities (hypertension and diabetes mellitus), infectious complications, and hospital stay.
Discussion
Understanding the burden and pattern of diseases among in-patient population is important. It provides significant information that includes resource allocation.9 The age, genetics, environment, social classes, and occupations are some of the factors that determine the spectrum and burden of diseases in a given population.14 Bindroo et al. reported a 75.3% acute surgical admissions to a government teaching hospital in India over a year period;15 our emergency and elective admissions were even. The mean age in our study, 44.3 years, is close to the 43.3 years reported from a regional hospital in South Africa over a four-year period.9 The overall male-to-female ratio in our study was 1.6:1, and this is consistent with the reported 1.2-2.7:1 from MLHDICs.2,8,9,14-16 In our study males were more predominant in emergency than elective admissions, 2.3:1 and 1.1:1 respectively, while Adem et al. reported a higher male proportion 3.1:1 and 1.4:1 respectively.8 The male dominance in our study could be related to the higher rate of male admissions, 79.3%, in trauma admissions previously reported from the same hospital.13 Ryan et al. reported a marginal female dominance in their emergency admission, 51.0%, in three rural hospitals in Mozambique.6
Most of our admissions were in the 20-40-years age group, and this is similar to a report by Mensur et al. from a regional teaching hospital in Ethiopia.16 The three top emergency admissions in our study were head injury (18.6%), appendicitis (15.9%), and gastrointestinal bleeding (6.4%). This is in comparison to a study from Worcester Hospital, a regional public healthcare facility care in the Western Cape province of South Africa, where appendicitis (23.8%), peripheral vascular disease (16.8%), and peptic ulcer disease (13.3%) were the most common surgical admissions.9 In our elective admissions oesophageal cancer (8.8%), hernia (7.2%), and cholelithiasis (5.7%) were the top three admissions while cholelithiasis (23.1%), inguinal hernia (21.8%), and fistula and fissure in ano (10.2%) were the common admissions at Worcester hospital.9 Among cancer admissions in our study, the top three were oesophageal (25.5%), breast (14.8%), and colorectal (8.9%), which were the same as at Worcester hospital, but the order was more evenly distributed - colorectal (17.6%), oesophageal (16.4%), and breast (14.0%).9 These differences can be partly explained by the difference in their population - fewer Africans of African ancestry or more mixed ancestry population in the Western Cape. Surgical procedures were performed in 51.3% of our admissions; this falls in the range of previous studies, 49.6-56.0% from Mozambique and Kenya.5,17
In MLHDICs, there is a very wide variation (21.0-90.0%) in the frequency of emergency admissions that undergo a surgical procedure.2,4,14,15 In our study, emergency admissions received a surgical procedure in 42.1% of the cases. Most of the operations in MLHDICs were reported in younger patients and female patients.4 We performed 66.7% of the operations in younger patients, but 59.8% of the procedures were among our male patients. This could be partly due to a male dominance in our elective and emergency admissions. Similar to a previous study from Mozambique,5 we found a lower rate of surgical procedures in GIT and neurosurgical admissions.
Our patients had pre-existing diabetes, hypertension, anaemia, and asthma in 5.1%, 17.9%, 0.1%, and 1.6% of the cases respectively, while Jawaid et al. reported 12.0%, 10.8%, 7.9%, and 2.2% respectively for the same comorbidities from a tertiary care public hospital in Pakistan.14 We found a SSI and an anastomotic leak in 3.1% and 0.2% of our patients who had operations and intestinal anastomosis respectively; while Watters et al. reported in 0.9% SSI and 1.6% anastomotic leak in a five-year review of publications, reports, and audits in Papua New Guinea.18 These differences could be partly due to the differences in prophylactic antibiotic use, patient population, and the level of surgical experience.
Our overall mortality rate of 6.1% was in the range reported from MLHDICs, 1.8-9.14%.2,5-9,14-19 Mortalities in MLHDICs are reported in emergency admissions to range from 3.6-21.1% and in elective admissions in 0.3-5.3%.2,8,15,17 In our study we found a mortality of 7.0% and 5.2% in our emergency and elective admissions respectively. Among our mortalities, 57.2% were in emergency admissions; while Onyemaechi et al. found 67.5% for the same.2 As expected, we found a higher overall mortality rate in the first 24 hours of admission in emergency admissions than in elective admissions, 0.8% vs 0.3%, though not statistically significant. Our overall male-to-female mortality ratio of 2.4:1 is higher than one previous study, 1.6:1 in a tertiary hospital in Nigeria.2 A number of studies showed that most of the mortalities, 62.3-65.6% were among males in MLHDICs;2,6,7,15 this is consistent with our report, 71.1%. Mortalities related to plastic and reconstructive, GIT, neurosurgery, urology, and cardiothoracic surgeries were reported from previous studies from MLHDICs in 23.1%,7 5.5-7.3%,7,8 7.9%,7 6.0%,7 and 11.9%,7 respectively, while we found 4.4%, 39.6%, 24.5%, 3.1%, and 18.9%, for the same respectively. The higher mortality in plastic and reconstructive surgery in our hospital could be related to the admission of burn patients under plastic and reconstructive surgery. Among our mortalities, 51.3% underwent surgical procedures, and this is similar to the report from Nigeria, 50.3%.2
We found comorbidities in 59.1% of our mortalities, which is lower than the 31.1% that Onyemaechi et al. reported from Nigeria.2 This could be attributable to the 44.4% HIV prevalence amongst out mortalities in our population in comparison to 5.3% prevalence from Nigeria.2 In our study we found hypertension, diabetes mellitus, epilepsy, and anaemia in 27.0%, 8.8%, 1.9% and 0.0% of our mortalities respectively; while others from MLHDICs found similar comorbidities in their mortalities in 2.4-8.6%,2,20 2.9-9.3%,2,20 0.7%,2 and 4.1%20 respectively.
Our overall mean hospital stay of 9.2 days was in the reported range, 4.9-12.6 days, from MLHDICs,2,5,9,17 but is higher than a report from Worcester Hospital, 4.9 days.9 In our study the overall hospital stays for emergency and elective admissions were not statistically different. Our mean hospital stay, 9.4 days, for our emergency patients was longer than 4.8 days reported previously from three rural hospitals in Mozambique.5 The length of hospital stay was highest among our plastic and reconstructive surgical admissions where burn patients were treated; this is similar to previous studies that reported longer hospital stay in burn patients from Mozambique and South Africa.5,9
The readmission rate is a well-recognised quality measure that has been analysed and widely used in certain countries.9,21 In our study the readmission rate for GIT was 8.8%, which is lower than the reported 11.3% from France, a HHDIC.21 The higher rate in the study from France is probably multifactorial due to differences in the study population, higher number of day-case procedures, and their inclusion of any readmission within 30-days after the operation. The most important preventive measure to reduce readmission is by providing adequate and appropriate education and information to the patient and close family members prior to discharge.21 Our discharge against medical advice, 0.7%, is lower than the 2.2% reported by Jawaid et al. from Pakistan.14 The retrospective design of this study and not including the impact of antiretroviral treatment on the outcome in HIV-positive patients, and absence of follow-up after discharge, referral to other hospitals, and refusal of hospital treatment are the major limitations of this study.
Conclusion
This study documented the spectrum, burden, and comorbidities of surgical diseases at our hospital. GIT diseases dominated our admissions. HIV infection was the major comorbid condition. Vascular patients had the highest number of comorbidities. HIV-positive patients with CD4 count < 200 had a higher mortality rate than those with > 200. A prospective study to investigate the effect of HIV-infection (CD4 count and viral load) and the impact of antiretroviral treatment on the outcomes of individual surgical conditions is warranted. The relatively higher mortality rates among patients with hypertension, diabetes, and HIV-positive patients with CD4 count < 200 in our study warrants further investigation.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval was granted by The Research and Ethics Committee (REC) of Princess Marina Hospital (PMH
5/79(406-1-2017)).
ORCID
AG Bedada https://orcid.org/0000-0002-5576-4409
MJ Mpapho https://orcid.org/0000-0003-4340-0824
SG Hamda https://orcid.org/0000-0003-4003-6916
REFERENCES
1. Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030 evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-624. [ Links ]
2. Onyemaechi NO, Popoola SO, Schuh A, et al. Mortality pattern of hospitalised surgical patients in a Nigerian tertiary hospital. Indian J Surg. 2015;77:881-5. https://doi.org/10.1007/s12262-014-1048-z. [ Links ]
3. Hider P, Wilson L, Rose J, et al. The role of facility-based surgical services in addressing the national burden of disease in New Zealand: An index of surgical incidence based on country-specific disease prevalence. Surgery. 2015;158(1):44-54. https://doi.org/10.1016/j.surg.2015.04.005. [ Links ]
4. Chichom Mefire A, Atashili J, Mbuagbaw J. Pattern of surgical practice in a regional hospital in Cameroon and implications for training. World J Surg. 2013;37:2101-8. https://doi.org/10.1007/s00268-013-2116-4. [ Links ]
5. Anderson JE, Erickson A, Funzamo C, et al. Surgical conditions account for the majority of admissions to three primary referral hospitals in rural Mozambique. World J Surgery. 2014;38:823-9. https://doi.org/10.1007/s00268-013-2366-1. [ Links ]
6. Ryan M, Kelliher G, Mealy K, Keane F. Characteristics of patients who are acutely admitted to hospital under surgical care and do not have a surgical procedure - Is there an alternative to admission? Surgeon. 2017;15(5):259-66. https://doi.org/10.1016/j.surge.2015.07.004. [ Links ]
7. Ekeke ON, Okonta KE, Igwe PO. Surgical inpatient mortality in a Nigerian tertiary hospital. Niger Clin Pract. 2016;19(3):308-12. https://doi.org/10.4103/1119-3077.179286. [ Links ]
8. Adem A, Abebe A, Abdurahman M. Pattern of surgical admissions to Tikur Anbessa Hospital, Addis Ababa, Ethiopia. East Cent Afr J Surg. 2001;6(1). [ Links ]
9. Pape J, Swart O, Duvenage R. Four-year review of admissions to a South African regional hospital general surgery department. S Afr Med J. 2019;109(2):122-6. https://doi.org/10.7196/SAMJ.2019.v109i2.13433. [ Links ]
10. Lavy C, Sauven K, Mkandawire N, et al. State of surgery in tropical Africa a review. World J Surg. 2011;35:262-71. https://doi.org/10.1007/s00268-010-0885-6. [ Links ]
11. The World Bank IBRD-IDA Data. Available from: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=BW. Accessed 14 July 2022. [ Links ]
12. UNICEF-Botswana-2018-Health-Budget-Brief.pdf. Available from: https://www.unicef.org/esa/media/2456/file/UNICEF-Botswana-2018-Health-Budget-Brief.pdf. Accessed 14 July 2022. [ Links ]
13. Bedada AG, Tarpley MJ, Tarpley JL. The characteristics and outcomes of trauma admissions to an adult general surgery ward in a tertiary teaching hospital. Afr J Emerg Med. 2021;11(2):303-8. https://doi.org/10.1016/j.afjem.2021.04.002. [ Links ]
14. Jawaid M. The pattern of diseases in a surgical unit at a tertiary care public hospital of Karachi. Pak J Med Sci. 2004;20(4):311-4. [ Links ]
15. Bindroo S, Saraf R. Surgical mortality audit - lessons learned in a developing nation. Int Surg. 2015;100(6):1026-32. https://doi.org/10.9738/INTSURG-D-14-00212.1. [ Links ]
16. Mensur Y, Gebretsadik B, Gashaw M, Johnstone JM. One year audit of surgical admissions at Gondar University Medical College. East Cent Afr J Surg. 2007;12(1):12-8. [ Links ]
17. Masiira-Mukasa N, Ombito BR. Surgical admissions to the Rift Valley provincial general hospital, Kenya. East Afr Med J. 2002;79(7):373-8. https://doi.org/10.4314/eamj.v79i7.8842. [ Links ]
18. Watters DA, Kapitgau WM, Kaminiel P, et al. Surgical capability and surgical pathology in Papua New Guinea in the year 2000. ANZ J Surg. 2001;71(5):274-80. https://doi.org/10.1046/j.1440-1622.2001.02101.x. [ Links ]
19. Guy S, Lisec C. Emergency laparotomy outcomes before and after the introduction of an acute surgical unit. Int J Surg Open. 2018;10:61-5. https://doi.org/10.1016/j.ijso.2017.12.001. [ Links ]
20. Ayoade BA, Thanni LO, Shonoiki-Oladipupo O. Mortality pattern in surgical wards of a university teaching hospital in southwest Nigeria: A review. World J Surg. 2013;37:504-9. https://doi.org/10.1007/s00268-012-1877-5. [ Links ]
21. Gauduchon L, Sabbagh C, Regimbeau JM. Re-admission after gastro-intestinal surgery. J Visc Surg. 2015;152(6):S97-104. https://doi.org/10.1016/j.jviscsurg.2015.09.013. [ Links ]
 Correspondence:
Correspondence:
AG Bedada
Email: bedaleQ0@yahoo.co.uk














