Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.62 no.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00197
GENERAL SURGERY
The rate of iatrogenic injuries in surgical patients appears resistant to multiple interventions: what can we learn from aviation safety?
H Wain; DL Clarke; S Wall
Department of Surgery, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: This project analyses all iatrogenic injuries from our department over the last decade and tracks their rate against several interventions
METHODS: All patients who sustained an iatrogenic injury between 2012 and 2022 were reviewed
RESULTS: A total of 946 iatrogenic injuries occurred in 731 patients. Sixty per cent of these patients were male; the median age was 39 years. Of 946 injuries, 574 (60.7%) occurred during an operation, and 372 (39.3%) were not related to an operation. Of the operative injuries 412 (71.8%) were enteric injuries. Of the 372 non-operative iatrogenic injuries 304 (82%) were due to indwelling devices (ID), and 34 (10%) occurred during flexible endoscopy. Fifty-five per cent of the injuries due to ID were due to central venous catheters (CVC) and urinary catheters (UC). CVC contributed toward 31% of all non-operation related iatrogenic injuries. One in 54 admissions (946/51 178) and one in 47 (574 /27 342) patients undergoing an operation sustained an iatrogenic injury. The annual rate of iatrogenic injuries did not decrease over the decade despite a multifaceted approach to reduce them. Interventions included electronic database development, procedural standardisation, and checklist implementation
CONCLUSION: Despite multiple interventions over a decade, our rate of iatrogenic injury remains constant. Ongoing multifaceted efforts to reduce this rate must focus on engendering a culture of safety at all levels of healthcare if we hope to match the enviable safety record of the aeronautics industry
Keywords: iatrogenic injury, patient safety, safety
Introduction
The publication of "To err is human" some 20 years ago highlighted the impact of human error on patient safety and outcomes.1 This stimulated the patient safety movement, which set out to improve outcomes by reducing both the incidence of human error and its impact on patients. The patient safety movement has pointed to the aeronautical industry as a model for reducing and limiting the impact of human error. The aeronautical industry has developed an enviable safety record over the last five decades. A major component of the success of the aeronautical industry in achieving a high level of safety has been the collection of routine data on all safety related events for analysis. This data has then been used to develop and support multifaceted interventions designed to limit and reduce the rate of error and the impact of error in the aeronautical industry. These interventions include sustained, highly regulated multi-factorial approaches consisting of standardised procedures, along with closed loop feedback systems, checklists, and the ubiquitous use of simulators to train pilots. Healthcare has tried to adopt some of these strategies with variable results. The healthcare system has lagged many other industries in terms of developing electronic records, which are capable of capturing and collating data on patient care for analysis.
Our unit has developed a hybrid electronic medical registry (HEMR), which has allowed for the capture of clinical data on all surgical admissions. In tandem with the implementation of the HEMR over the last decade has been the roll out of several interventions in our institution designed to provide structure and guidance and to hopefully reduce the rate of error, and to limit the impact of these errors when they do occur.
This study analyses all iatrogenic injuries over the last decade. It seeks to classify these injuries, to identify trends in the rate of these injuries and attempts to assess the impact of these multifaceted interventions on the incidence of iatrogenic injury. In so doing, we aim to strengthen the evidence which informs our ongoing efforts to develop and implement strategies and algorithms designed to reduce the incidence and impact of iatrogenic injury. The primary aim of this study was to identify and categorise all iatrogenic injuries documented in our department over the last decade. The secondary aim was to assess the impact of the numerous quality improvement and error reduction interventions implemented over the same period.
Clinical setting
The department of surgery at Greys Hospital in Pietermaritzburg, South Africa, has implemented and maintained the HEMR since December 2012.2 The HEMR captures multiple data points on all surgical admissions and discharges in real time. These include basic demographics, admission characteristics, medical or surgical history, allergies, investigation results, admission diagnosis, and the initial management plan. It also allows for reports to be generated following an operation or endoscopic evaluation. Discharge information captured includes a summary of care, trends in blood results, discharge disposition, intensive care unit (ICU) duration, and patient outcome. Staff enter clinical data into the system, and this data then populates the patient record, which is printed. The data entered is also captured directly into a relational database where it is available for analysis. The HEMR has a dedicated module for the reporting of adverse events.3,4 The information in this module is used for monthly morbidity conferences.56 The data for this study was drawn from data captured in the adverse events module of the HEMR.
Over the last decade, the department has introduced several interventions, apart from the HEMR, intended to reduce the incidence and limit the impact of error. These include the new format morbidity and mortality meeting focused on the data captured in the morbidity component of the HEMR, and the employment of an attending in trauma who is directly charged with supervising the HEMR in 2014.6 In 2013 and 2019, handbooks were developed for general surgery and trauma surgery, respectively, to clarify policies for common conditions, and to standardise common procedures. In 2015, "weekend handover forms", intended to bolster the existing person-to-person handovers to the on-call team, were introduced. In conjunction with a formal handover ward round, these handover forms clarify details about each patient and highlight potential risks for adverse events as anticipated by the managing team. The World Health Organization (WHO) Surgical Safety Checklist was introduced in conjunction with the anaesthesiology service in 2009. In addition to these interventions, the department provides ongoing guidance for trainees as events arise and fosters an ethos of honesty regarding reporting of adverse events. When an adverse event is noted, the resultant discussion is a learning experience rather than a punitive one. The advanced trauma life support (ATLS) course has been conducted locally since 2009, and multiple senior staff members are instructors. The ATLS contains dedicated modules that standardise insertion techniques for intercostal chest drains and central venous catheters (CVC). For patients in the ICU or the general ward, care bundles have been introduced and undergo frequent review and revision.
Methods
An iatrogenic injury was defined as any unintentional harm to a patient resulting from an investigation, intervention, or use of a medical device. Following ethical approval from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (BCA 221/13 and BREC/00004792/2022), all captured adverse events from December 2012 to November 2022 were extracted for analysis. Categorisation of this data identified all iatrogenic injuries, which were further analysed for this study. We included records for all inpatients. This includes all ages, genders, admitting units (general surgery, trauma surgery, paediatric surgery, and admission type (elective or emergency). Outpatients were not included in analysis. Duplicate entries were excluded.
Once identified, iatrogenic injuries were categorised into two domains - intraoperative or non-operative injuries. The intraoperative injuries were further divided according to the organ injured. Non-operative injuries were divided into the intervention or investigation during which they occurred, including endoscopy, endoscopic retrograde cholangio pancreatography (ERCP), due to an indwelling device (ID), or other miscellaneous causes. Miscellaneous entries included events, which we defined as an iatrogenic injury but that did not occur during a specified intervention, e.g. a patient injured due to improper sharps disposal in a ward.
Results
During the study period, a total of 946 iatrogenic injuries occurred in 731 patients. In some cases, more than one injury was sustained by a single patient. Sixty per cent (512/731) of these patients were male. The median age of the patients who sustained an iatrogenic injury was 39 years. Of the 731 patients, 513 (70.2%) were general surgical, 146 (20%) trauma patients, and 63(8.6%) paediatric surgical patients. In nine patients, the admitting service was not clear.
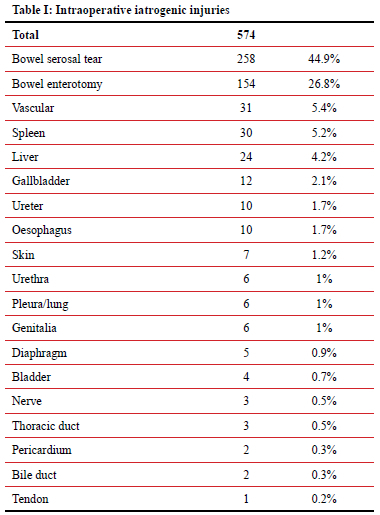
A total of 946 injuries were captured, of which 574 (60.7%) occurred during an operation, and 372 (39.3%) were not related to an operation. Of 574 iatrogenic injuries, which occurred during an operation, 412 (71.8%) were enteric injuries. These included 258 (45%) serosal tears and 154 (27%) enterotomies. The majority of the remaining injuries were to vascular structures, the spleen, and the liver. A detailed breakdown is provided in Table I.
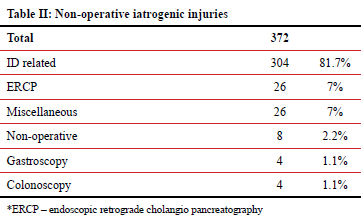
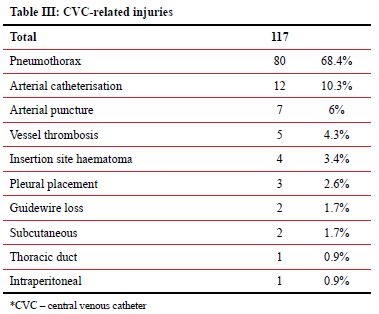
Of the three hundred and seventy-two iatrogenic injuries not related to a surgical procedure, 304 (82%) were due to ID, and 34 (10%) occurred during flexible endoscopy. Subgroup analysis of the 304 injuries related to an ID showed that just over half (55%) were associated with two devices - CVC, and urinary catheters (UC). A detailed breakdown is provided in Table II. CVCs contributed toward 36% of iatrogenic injuries associated with IDs (117/330), and 32% of all non-operation related iatrogenic injuries. Of 117 CVC-related injuries, 80 were pneumothoraxes (68%), and 19 (16%) were arterial injuries. Table III expands on this.
During the study period there were 51 178 distinct patient admissions, and 27 342 surgical procedures. This translates to one patient in every 54 admissions (946/51 178) sustaining an iatrogenic injury and one patient in every 47 operations sustaining an iatrogenic injury (574 /27 342). Similarly, one out of every 720 flexible endoscopies (34/24 481) were associated with an iatrogenic injury.
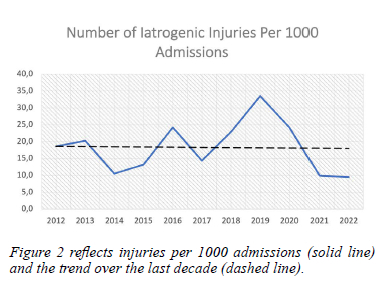
Analysis of iatrogenic injuries by year revealed a wide variation. There was an increase in the reported rate of iatrogenic injury following the employment of an attending with a dedicated commitment to the maintenance of the HEMR in 2014. The year, in which the fewest injuries were documented was 2021 (49 injuries), and the greatest number was in 2019 (181 injuries). No discernible sustained decrease was noted over the study period when expressed per 1000 admissions. Figures 1 and 2 attempt to plot the rate of iatrogenic injury against the various interventions implemented over the last decade.
Discussion
Error in healthcare is an ongoing challenge.7 The focus of this study has been iatrogenic injuries, which remain a concern in modern healthcare despite myriad advances. The incidence of iatrogenic injuries remains high, and the impact significant. Despite a sustained effort to reduce the incidence and impact of iatrogenic injury, the rate remains high. This data highlights several lessons. The first is the need to collect information on iatrogenic injury. Without an accurate overview of the extent of problem, it is impossible to manage the situation. The HEMR has helped with this. Prior to the development of the HEMR it was impossible to accurately track iatrogenic injuries. The increase in incidence between 2014 and 2015 likely reflects improved reporting with a dedicated attending focusing on the HEMR.
Secondly, our data suggests that it is difficult to entirely eliminate iatrogenic injury. Variations with patient anatomy, clinical setting and experience, and stage of pathology make it difficult to completely standardise procedures. Our institution has run a multifaceted programme designed to improve patient care and outcomes for over a decade. This programme has included educational efforts such as the ATLS, safety nets like the surgical checklist, as well as attempts to standardise procedures with bundles of care, and handbooks. Despite these efforts, the rate of iatrogenic injury in our institution appears to be consistent.
The healthcare system has attempted to emulate the aviation industry with regards to safety.8-13 The introduction of procedural standardisation and checklists, feedback systems, and simulation-based training have been taken from aviation. With these interventions, the aviation industry has developed an enviable safety record. However, the same success has not been enjoyed in healthcare. Some authors have challenged the comparison between healthcare and aeronautics and feel that the two systems, whilst both highly complex, are not directly comparable.
These failures may result from a misinterpretation of the message contained in the comparison between healthcare and aviation. The most important factor in achieving aeronautical safety has been the system-wide culture change in that industry. The emphasis on safety and error reduction centralised health and safety in aeronautics. This culture change has permeated the industry over the last 50 years. This is the central lesson in the comparison between healthcare and aeronautics. It is unlikely any single intervention will dramatically reduce the rate of iatrogenic injury. Rather, it is the cumulative effect of multiple endeavours which will place patient safety at the centre of clinical endeavours and help healthcare develop a safety record on a par with the aeronautical industry.
Conclusion
Despite multiple interventions introduced over a decade, the rate of iatrogenic injury in our institution remains constant. A culture change is required in healthcare, where patient safety is centralised. Ongoing efforts to reduce iatrogenic injury rates must focus on engendering a culture of safety at all levels of healthcare if we hope to match the enviable safety record of the aeronautics industry.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethics approval was obtained from the Biomedical Research Ethics Committee (BREC) of The University of KwaZulu-Natal (UKZN), number BREC/00004792/2022.
ORCID
H Wain https://orcid.org/0000-0002-6693-0062
DL Clarke https://orcid.org/0000-0002-8467-1455
S Wall https://orcid.org/0000-0002-3935-9139
REFERENCES
1. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human - Building a Safer Health System. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000. PMID: 25077248. [ Links ]
2. Laing GL, Bruce J, Clarke DL. Tick-box admission forms improve the quality of documentation of surgical emergencies, but have limited impact on clinical behaviour. S Afr Med J. 2014;104:435-8. https://doi.org/10.7196/SAMJ.7673. [ Links ]
3. Laing GL, Bruce J, Skinner D, et al. Using a hybrid electronic medical record system for the surveillance of adverse surgical events and human error in a developing world surgical service. World J Surg. 2015;39:70-9. https://doi.org/10.1007/s00268-014-2766-x. [ Links ]
4. Laing GL, Bruce J, Skinner D, et al. Development, implementation, and evaluation of a hybrid electronic medical record system specifically designed for a developing world surgical service. World J Surg. 2014;38:1388-97. https://doi.org/10.1007/s00268-013-2438-2. [ Links ]
5. Clarke DL, Furlong H, Laing GL, et al. Using a structured morbidity and mortality meeting to understand the contribution of human error to adverse surgical events in a South African regional hospital. S Afr J Surg. 2013;51:122-6. [ Links ]
6. Kong VY, Clarke DL. Analysis of 5 years of morbidity and mortality conferences in a metropolitan South African trauma service. S Afr Med J. 2016;106:695-8. https://doi.org/10.7196/SAMJ.2016.v106i7.10549. [ Links ]
7. Aldous CM, Searle R, Clarke DL. An educational programme for error awareness in acute trauma for junior doctors. Afr J Health Prof Educ. 2014;6:161-4. https://doi.org/10.7196/AJHPE.350. [ Links ]
8. Golemboski K. Improving patient safety: lessons from other disciplines. Clin Lab Sci. 2011;24:114. https://doi.org/10.29074/ascls.24.2.114. [ Links ]
9. Kapur N, Parand A, Soukup T, et al. Aviation and healthcare: a comparative review with implications for patient safety. JRSM Open 2015;7:2054270415616548. https://doi.org/10.1177/2054270415616548. [ Links ]
10. Milam DF. Improving patient safety in the operating room: lessons from the aviation industry. Nat Clin Pract Urol. 2008;5:289-9. https://doi.org/10.1038/ncpuro1134. [ Links ]
11. Salas E, Maurino D, Curtis M. Human factors in aviation: an overview. Human factors in aviation. 2010:3-19. https://doi.org/10.1016/B978-0-12-374518-7.00001-8. [ Links ]
12. Toff N. Human factors in anaesthesia: lessons from aviation. Br J Anaesth. 2010;105:21-5. https://doi.org/10.1093/bja/aeq127. [ Links ]
13. Singer SJ, Rosen A, Zhao S, et al. Comparing safety climate in naval aviation and hospitals: implications for improving patient safety. Health Care Manage Rev. 2010;35:134-46. https://doi.org/10.1097/HMR.0b013e3181c8b20c. [ Links ]
 Correspondence:
Correspondence:
H Wain
Email: howardwain@icloud.com














