Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.62 no.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00215
TRAUMA
Outcomes of non-operative management of penetrating abdominal trauma
N AlmglaI, II; M Raul RiskIII; S EduI; A NicolI; P NavsariaI
IDepartment of General Surgery, Trauma Centre, University of Cape Town, South Africa
IIDepartment of Surgery, University of Tripoli, Libya
IIIInstituto de Medicina Traslacional e Ingenieria Biomedica (IMTIB), CONICET, Instituto Universitario del Hospital Italiano, Hospital Italiano de Buenos Aires, Argentina
ABSTRACT
BACKGROUND: Selective non-operative management (SNOM) of penetrating abdominal trauma (PAT) is routinely practised in our trauma centre. This study aims to report the outcomes of patients who have failed SNOM
METHODS: Patients presenting with PAT from 1 May 2015 - 31 January 2018 were reviewed. They were categorised into immediate laparotomy and delayed operative management (DOM) groups. Outcomes compared were postoperative complications, length of hospital stay and mortality
RESULTS: A total of 944 patients with PAT were reviewed. After excluding 100 patients undergoing damage control surgery, 402 (47.6%) and 542 (52.4%) were managed non-operatively and operatively, respectively. In the SNOM cohort, 359 (89.3%) were managed successfully without laparotomy. Thirty-seven (86.0%) patients in the DOM group had a therapeutic laparotomy, and six (14.0%) had an unnecessary laparotomy. Nine (20.9%) patients in the DOM group developed complications. The DOM group had lesser complications. However, the two groups had no difference in hospital length of stay (LOS). There was no mortality in the non-operative management (NOM) group
CONCLUSION: In this study, we demonstrated no mortality and less morbidity in the DOM group when appropriately selected compared to the immediate laparotomy group. This supports the selective NOM approach for PAT in high volume trauma centres
Keywords: penetrating abdominal trauma, failed non-operative management, delayed operative management
Introduction
The management of trauma in general and specifically penetrating abdominal trauma (PAT) continues to represent a considerable burden on the local healthcare system. The management of PAT has evolved over the last five decades from routine mandatory laparotomy to selective non-operative management (SNOM). SNOM has been embraced as a safe alternative for stab wounds (SW) to the abdomen since the initial reports by Shaftan and Stein.1-3 More recently, large studies from South Africa by Muckart et al. and Demetriades et al. suggested that using repeated clinical abdominal examination, SNOM can be applied safely to a specific group of patients with gunshot wounds (GSWs) to the abdomen.45 Since then, the SNOM of GSW has gained momentum as an acceptable treatment strategy. Despite accepting SNOM as a routine practice for PAT in highvolume trauma centres, there is a lack of reporting of the outcomes of unsuccessful SNOM. A better understanding of this particular group is required to guide an effective and safe approach for patients with PAT, especially those selected for non-operative management (NOM). This study aims to investigate the outcomes of unsuccessful SNOM, or more appropriately labelled delayed operative management (DOM) with patients undergoing immediate laparotomy.6,7
Materials and methods
This was a single-centre observational study of all patients presenting with PAT to the Groote Schuur Hospital Trauma Centre (GSHTC) in Cape Town, South Africa, from 1 May 2015 to 31 January 2018. Patients were managed according to established GSHTC protocols for PAT.6-9 The study was approved by the Human Research Ethics Committee of the University of Cape Town (HREC 770/2017). Only patients excluded were those undergoing an index damage control laparotomy.
Patient demographics, vital signs, clinical findings and trauma severity scores were recorded. The indications for immediate laparotomy include hemodynamic instability and peritonism (tenderness, rebound, guarding, rigidity, and diminished or absent bowel sounds). The protocol is modified for patients presenting with blood per rectum, evisceration (omentum - if no indication for immediate laparotomy, for SNOM; organ evisceration - immediate laparotomy), and computed tomography (CT) findings suggestive of hollow visceral injury (free/loculated air, free fluid, bowel wall oedema and mesenteric stranding).9,10 CT scans were indicated in stable patients without peritonitis presenting with haematuria or right upper quadrant missile trajectory to exclude urinary tract and liver injury, respectively. A CT cystogram was performed in the presence of haematuria, where trajectory traversed the pelvis. CT scan is also indicated when there is uncertainty about whether a clinically suspected tangential bullet trajectory has breached the peritoneal cavity. CT scans of the abdomen were done in the radiology department using 128 channel scanner with a high-power injection of 100 mL of intravenous contrast at 5 mL/second. Arterial, portovenous, and delayed phases were routinely acquired. Patients presenting with PAT who did not satisfy the above indications for immediate laparotomy were selected for a trial of NOM.
Patients selected for NOM were admitted to the trauma high-care ward. These patients underwent continuous monitoring of vital signs and serial clinical examinations. Oral intake was introduced after 24 hours of uneventful observation. A patient was discharged once tolerating normal diet with an abdominal injury form indicating the warning signs for immediate return. Patients selected for NOM with increasing abdominal tenderness, haemodynamic instability, or features of sepsis underwent DOM. Delayed operative management refers to any surgical intervention after an initial decision for NOM, regardless of time. The present study defines a laparotomy as therapeutic if intraoperative injuries identified required intervention. Where no intraabdominal injuries were identified, laparotomies were considered negative laparotomies (NL). Non-therapeutic laparotomies (NTL) refer to injuries confirmed on laparotomy, but not requiring any intervention. Unnecessary laparotomy includes both NTL and NL.
Statistical computations were made using RStudio (RStudio Team, 2021. RStudio: Integrated Development Environment for R, Boston, MA).11 Statistical significance was set at p < 0.05. Categorical data were reported as numbers and percentages, and groups were compared using Pearson's chi-square test. Fisher's exact test was used for 2 x 2 contingency tables. Continuous data were reported as the median and interquartile range (IQR) and mean with 95% confidence interval, with groups compared using the Wilcoxon rank-sum test and student t-test, respectively.
Results
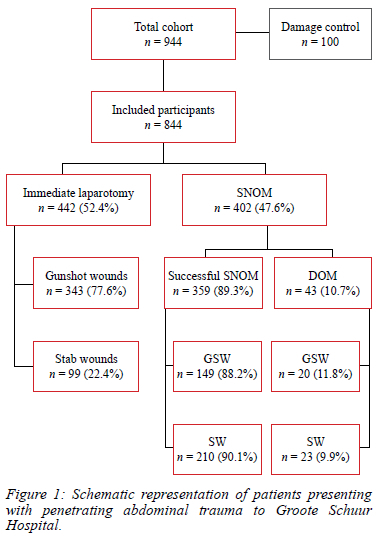
After excluding 100 haemodynamically unstable patients who underwent damage control surgery at the index laparotomy, the records of 844 clinically evaluable and haemodynamically stable patients were analysed. Of these, 402 (47.6%) were initially selected for NOM, and the remaining 442 (52.4%) underwent immediate laparotomy. Of the 402 patients selected for NOM, 359 (89.3%) were managed successfully without laparotomy, and the remaining 43 (10.7%) underwent DOM. Of 442 patients who underwent immediate laparotomy, 399 (90.3%) experienced a therapeutic laparotomy, and 43 (9.7%) patients had either a NL or NTL; 20 (4.5%) and 23 (5.2%), respectively. The treatment pathways and mechanism of injury are illustrated in Figure 1.
The immediate laparotomy and DOM groups were compared for patient demographics, mechanism of injury, trauma severity scores, admission vital signs, biochemistry results, and abdominal clinical findings (Table I). There were no differences in the patient's age, demographics, and haemoglobin levels in the emergency department between the two groups. However, more patients became haemodynamically unstable (p < 0.001) and required blood transfusion (p < 0.001) in the immediate laparotomy group. As expected, the mechanism of injury was more distributed towards GSW in the immediate laparotomy group. The patients in the immediate laparotomy group presented to the emergency centre with higher trauma scores than the NOM group. However, there was no significant difference in the number of patients presenting with GSW and SW in the DOM group, 20 (46.5%) with GSW and 23 (53.5%) with SW.
Two hundred and fifty-two (62.7%) patients in the SNOM group had a CT scan on admission. Of these, 29 (11.5%) patients with negative scans failed abdominal observations and underwent a delayed laparotomy. The indications for surgical interventions in the DOM group were increasing abdominal tenderness in 37.2% (4 GSW, 12 SW), concern of sepsis in 25.6% (3 GSW, 8 SW), and either repeat or delayed first time CT study results in 32.6% (11 GSW, 3 SW). In contrast, peritonitis was the most common indication for surgery in the immediate laparotomy group, followed by radiological findings and development of haemodynamic instability (Table II). However, two patients in the NOM group became haemodynamically unstable. The first patient was referred with a single GSW to his lower back (left side). CT scan demonstrated a grade IV splenic laceration with minor haemoperitoneum. The patient dropped his haemoglobin from 10 g/dl to 7 g/dl with compensated shock a day later. The patient went for an emergency laparotomy and had a splenectomy. The second patient presented with GSW to the right flank. CT scan showed grade II liver and right kidney injuries. The patient underwent DOM after a significant drop in the haemoglobin to 8 g/dl with compensated shock. He had a NTL with findings consistent with the CT findings, and no hollow organ injury was identified.
Time in hours from admission to surgery was significantly longer in the DOM patients (Table II). The median time from admission to surgery in the DOM group was 32 (IQR 25-61) hours. This time interval was significantly longer than the immediate laparotomy group, where most patients went to the theatre within five hours of admission (p = 0.001).
Three hundred and ninety-nine (90.3%) patients underwent immediate laparotomy with therapeutic interventions. The remaining 43 (9.7%) had a NL or NTL, 4.5% and 5.2%, respectively. Thirty-seven (86.0%) patients in the DOM group had a therapeutic laparotomy, and six (14.0%) had an unnecessary laparotomy, of which three (7.0%) were negative, and three (7.0%) were non-therapeutic. Hollow viscus perforation was found in 355 (79.8%) patients in the immediate laparotomy group and 24 (55.8%) in the DOM group. The small bowel was the most frequently injured organ in the immediate laparotomy group, followed by the colon. Ten (23.3%) patients in the DOM group had colon injuries as the most frequently injured organ. A detailed description of the intraoperative finding is summarised in Table III.
The distribution of the wound location between the two groups was insignificant (p = 0.39). Most immediate laparotomy patients sustained a penetrating injury to the anterior abdomen or left flank, 28.1% and 21.8%, respectively. Most DOM patients sustained a penetrating injury to the left flank region, 28.6%. The wound location and detailed description for both groups are shown in Table IV There were fewer complications according to the Clavien-Dindo classification (CD) in the DOM groups. Major complications (CD III and IV) were observed in three patients, and minor complications (CD I and II) in six patients. The secondary outcome of mortality showed 6.3% deaths in the immediate laparotomy group and no deaths in the DOM group. Table V summarises the outcomes, including deaths, complications and ICU and hospital LOS. A detailed description of the complications in the nine patients undergoing DOM is presented in Table VI.
Discussion
The management of PAT has evolved and undergone substantial paradigm shifts over the last century. In view of the low mortality rate associated with unnecessary laparotomies and the perceived potential morbid outcomes related to DOM, the opponents of SNOM swear by a philosophy of "look and see" rather than "wait and see" for PAT.1,12,13 Despite the low mortality rate associated with the unnecessary laparotomy, it is not a benign intervention. Reported complication rates between 2.5-41.0% include sepsis, postoperative ileus, and pneumonia, with long-term complications such as incisional hernia and small bowel obstruction also documented. 2,14-18 The emergence of SNOM has been a ground-breaking change in the management of civilian PAT.1,2,12,19,20 SNOM has been reported not to be associated with increased mortality and morbidity.21 In the current study, 70.2% of the patients with SW to the abdomen were selected for NOM with a 90.1% success rate, and 9.9% underwent DOM.22
Unlike abdominal SW, SNOM for abdominal GSW has not gained full acceptance and has faced initial resistance due to the higher rate of intra-abdominal injuries.23,24 The concept of mandatory laparotomy for GSWs to the abdomen has become less dogmatic. Demetriades et al. and Velmahos et al. published a series of prospective studies that showed that GSW to the abdomen could be managed safely without operative exploration in selected patients. Their figures suggest that SNOM would be successful in one-third of patients with GSW to the anterior abdomen and two-thirds of patients with GSW to the back.25,26 Similarly, in this study, 33.0% of patients presenting with GSW to the abdomen were selected for NOM. The success rate was 88.2%, and the delayed operative rate was 11.8%, within the range observed in the literature.27-29 Navsaria et al. had previously demonstrated that SNOM of GSW to solid organs (liver and kidneys) is a feasible and safe option in selected patients with no peritoneal signs and after a careful evaluation with CT scan.8,28,30,31
Despite the undeniable benefits of SNOM, DOM is perceived to be associated with increased morbidity and mortality. NOM is found to have reduced negative laparotomy rates, overall complications, reduced LOS and lowered costs in both SW and GSW to the abdomen.22,32,33 There is considerable divergence of opinions between different authors. Zafar et al. reviewed the outcome of NOM of PAT from the North America national trauma database and found that NOM is generally successful; however, its failure is associated with increased mortality compared to the successful non-operative group.27 On the other hand, a systematic review by Lamb et al. in 2014 included more than 18 000 patients with abdominal GSW; 32.2% of the patients underwent NOM. Of these patients, 15% underwent delayed laparotomy. They observed that the delayed laparotomy group had similar outcomes to the immediate laparotomy group.34 Similarly, Peev et al. stated that delayed surgical treatment in patients who failed SNOM for PAT does not cause unnecessary mortality or morbidity if performed in a structured protocol.35 Furthermore, a more recent systematic review in 2018 by Al Rawahi et al. analysed 6 777 patients who underwent SNOM after GSW to the abdomen and concluded that non-operative management is safe.29 Table VII summarises the most recent large series of PAT.
NOM is a dynamic process; it starts with the appropriate selection of the patient for NOM, followed by specialised radiology, close observation and serial clinical examination. Should the patient develop a change in abdominal signs or features suggestive of intra-abdominal sepsis or haemodynamic instability, the patient should be considered for a delayed laparotomy.36 A negative CT scan does not exclude intra-abdominal injuries. We observed that 29 patients with negative CT scan subsequently had a delayed laparotomy. This emphasises the absolute need for admission and serial clinical examination. In the current study, the DOM rate was 10.7%, with 7.0% negative and 7.0% NTL rates, similar to previous studies.17,22 Conversely, the therapeutic laparotomy rate following DOM was 86.0% in this study, which compares with the calculated mean therapeutic laparotomy rate of 75% (R 36.0-100) in the recent literature.
This study showed that outcomes, including complications and mortality, are less in the DOM when compared with the immediate laparotomy group. The LOS in patients with PAT is no different in patients undergoing DOM than in those undergoing immediate laparotomy (Tables V and VI). We included both SW and GSW in our analysis as we believe that the principles of selective conservative management hold in both GSW and SW to the abdomen, and the treatment algorithm should be the same as we have demonstrated in our recent study.7
Conclusion
In this study, we demonstrated no mortality and less morbidity in the DOM group when appropriately selected compared to the immediate laparotomy group. This supports the selective NOM approach for PAT in high-volume trauma centres.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
University of Cape Town Human Ethics Research Committee approval no. (UCT/HREC: 770/2017).
ORCID
N Almgla https://orcid.org/0000-0001-5505-6894
M Raul Risk https://orcid.org/0000-0003-0107-2551
A Nicol https://orcid.org/0000-0001-5181-1151
P Navsaria https://orcid.org/0000-0002-5152-3317
S Edu https://orcid.org/0000-0002-1851-4021
REFERENCES
1. Stein A, Lissoos I. Selective management of penetrating wounds of the abdomen. J Trauma. 1968;8(6):1014-25. https://doi.org/10.1097/00005373-196811000-00003. [ Links ]
2. Shaftan GW. Indications for operation in abdominal trauma. Am J Surg. 1960;99:657-64. https://doi.org/10.1016/0002-9610(60)90010-6. [ Links ]
3. Shaftan GW. Selective conservatism in penetrating abdominal trauma. J Trauma. 1969;9(12):1026-8. https://doi.org/10.1097/00005373-196912000-00014. [ Links ]
4. Muckart DJ, Abdool-Carrim AT, King B. Selective conservative management of abdominal gunshot woundS: a prospective study. Br J Surg. 1990;77(6):652-5. https://doi.org/10.1002/bjs.1800770620. [ Links ]
5. Demetriades D, Charalambides D, Lakhoo M, et al. Gunshot wound of the abdomen: role of selective conservative management. Br J Surg. 1991;78(2):220-2. https://doi.org/10.1002/bjs.1800780230. [ Links ]
6. Sander A, Spence R, Ellsmere J, et al. Penetrating abdominal trauma in the era of selective conservatism: a prospective cohort study in a level 1 trauma center. Eur J Trauma Emerg Surg. 2022;48(2):881-9. https://doi.org/10.1007/s00068-020-01478-y. [ Links ]
7. Sander A, Spence RT, McPherson D, et al. A prospective audit of 805 consecutive patients with penetrating abdominal trauma: evolving beyond injury mechanism dictating management. Ann Surg. 2022;275(2):e527-e33. https://doi.org/10.1097/SLA.0000000000004045. [ Links ]
8. Navsaria PH, Nicol AJ, Krige JE, et al. Selective nonoperative management of liver gunshot injuries. Ann Surg. 2009;249(4):653-6. https://doi.org/10.1097/SLA.0b013e31819ed98d. [ Links ]
9. Navsaria PH, Edu S, Nicol AJ. Civilian extraperitoneal rectal gunshot wounds: surgical management made simpler. World J Surg. 2007;31(6):1345-51. https://doi.org/10.1007/s00268-007-9045-z. [ Links ]
10. Da Silva M, Navsaria PH, Edu S, et al. Evisceration following abdominal stab wounds - analysis of 66 cases. World J Surg. 2009;33(2):215-9. https://doi.org/10.1007/s00268-008-9819-y. [ Links ]
11. RStudio Team. RStudio - Integrated Development for R. RStudio. Boston, MA: PBC; 2021. [ Links ]
12. Goldman LI, De Laurentis DA, Rosemond GP. Penetrating abdominal wounds in a civilian population. Am J Surg. 1962;104:46-51. https://doi.org/10.1016/0002-9610(62)90293-3. [ Links ]
13. Klickstein GD, Edmunds RT, Allen PD. Immediate laparotomy in penetrating wounds of the abdomen. NY State J Med. 1962;62:3923-6. [ Links ]
14. Nance FC, Cohn I, Jr. Surgical judgment in the management of stab wounds of the abdomen: a retrospective and prospective analysis based on a study of 600 stabbed patients. Ann Surg. 1969;170(4):569-80. https://doi.org/10.1097/00000658-196910000-00008. [ Links ]
15. Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma. 1995;38(3):350-6. https://doi.org/10.1097/00005373-199503000-00007. [ Links ]
16. Leppâniemi AK, Haapiainen RK. Selective nonoperative management of abdominal stab wounds: prospective, randomised study. World J Surg. 1996;20(8):1101-5; discussion 5-6. https://doi.org/10.1007/s002689900168. [ Links ]
17. Demetriades D, Vandenbossche P, Ritz M, et al. Nontherapeutic operations for penetrating trauma: early morbidity and mortality. Br J Surg. 1993;80(7):860-1. https://doi.org/10.1002/bjs.1800800716. [ Links ]
18. Weigelt JA, Kingman RG. Complications of negative laparotomy for trauma. Am J Surg. 1988;156(6):544-7. https://doi.org/10.1016/S0002-9610(88)80549-X. [ Links ]
19. Hopson WB, Sherman RT, Sanders JW. Stab wounds of the abdomen: 5-year review of 297 cases. Am Surg. 1966;32(3):213-8. [ Links ]
20. Loria FL. Historical aspects of penetrating wounds of the abdomen. Surg Gynecol Obstet. 1948;87(6):521-49. [ Links ]
21. Friedmann P. Selective management of stab wounds of the abdomen. Arch Surg. 1968;96(2):292-5. https://doi.org/10.1001/archsurg.1968.01330200130028. [ Links ]
22. Navsaria PH, Berli JU, Edu S, et al. Nonoperative management of abdominal stab wounds: an analysis of 186 patients. S Afr J Surg. 2007;45(4):128-30, 32. [ Links ]
23. Dawidson I, Miller E, Litwin MS. Gunshot wounds of the abdomen. A review of 277 cases. Arch Surg. 1976;111(8):862-5. https://doi.org/10.1001/archsurg.1976.01360260030006. [ Links ]
24. Lowe RJ, Boyd DR, Folk FA, et al. The negative laparotomy for abdominal trauma. J Trauma. 1972;12(10):853-61. https://doi.org/10.1097/00005373-197210000-00004. [ Links ]
25. Demetriades D, Velmahos G, Cornwell E, et al. Selective nonoperative management of gunshot wounds of the anterior abdomen. Arch Surg. 1997;132(2):178-83. https://doi.org/10.1001/archsurg.1997.01430260076017. [ Links ]
26. Velmahos GC, Demetriades D, Foianini E, et al. A selective approach to the management of gunshot wounds to the back. Am J Surg. 1997;174(3):342-6. https://doi.org/10.1016/S0002-9610(97)00098-6. [ Links ]
27. Zafar SN, Rushing A, Haut ER, et al. Outcome of selective nonoperative management of penetrating abdominal injuries from the North American national trauma database. Br J Surg. 2012;99(Suppl 1):155-64. https://doi.org/10.1002/bjs.7735. [ Links ]
28. Navsaria PH, Nicol AJ, Edu S, et al. Selective nonoperative management in 1106 patients with abdominal gunshot wounds: Conclusions on safety, efficacy, and the role of selective CT imaging in a prospective single-center study. Ann Surg. 2015;261(4):760-4. https://doi.org/10.1097/SLA.0000000000000879. [ Links ]
29. Al Rawahi AN, Al Hinai FA, Boyd JM, et al. Outcomes of selective nonoperative management of civilian abdominal gunshot wounds: a systematic review and meta-analysis. World J Emerg Surg. 2018;13:55. https://doi.org/10.1186/s13017-018-0215-0. [ Links ]
30. Navsaria P, Nicol A, Krige J, Edu S, Chowdhary S. Selective nonoperative management of liver gunshot injuries. Eur J Trauma Emerg Surg. 2019;45(2):323-8. https://doi.org/10.1007/s00068-018-0913-z. [ Links ]
31. Navsaria PH, Nicol AJ. Selective nonoperative management of kidney gunshot injuries. World J Surg. 2009;33(3):553-7. https://doi.org/10.1007/s00268-008-9888-y. [ Links ]
32. Clarke DL, Allorto NL, Thomson SR. An audit of failed nonoperative management of abdominal stab wounds. Injury. 2010;41(5):488-91. https://doi.org/10.1016/j.injury.2009.10.022. [ Links ]
33. Velmahos GC, Demetriades D, Toutouzas KG, et al. Selective nonoperative management in 1856 patients with abdominal gunshot wounds: should routine laparotomy still be the standard of care? Ann Surg. 2001;234(3):395-402; discussion 3. https://doi.org/10.1097/00000658-200109000-00013. [ Links ]
34. Lamb CM, Garner JP. Selective nonoperative management of civilian gunshot wounds to the abdomen: a systematic review of the evidence. Injury. 2014;45(4):659-66. https://doi.org/10.1016/j.injury.2013.07.008. [ Links ]
35. Peev MP, Chang Y, King DR, et al. Delayed laparotomy after selective nonoperative management of penetrating abdominal injuries. World J Surg. 2015;39(2):380-6. https://doi.org/10.1007/s00268-014-2813-7. [ Links ]
36. Como JJ, Bokhari F, Chiu WC, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010;68(3):721-33. https://doi.org/10.1097/TA.0b013e3181cf7d07. [ Links ]
37. Inaba K, Barmparas G, Foster A, et al. Selective nonoperative management of torso gunshot wounds: when is it safe to discharge? J Trauma. 2010;68(6):1301-4. https://doi.org/10.1097/TA.0b013e3181bbc529. [ Links ]
38. Navsaria PH, Edu S, Nicol AJ. Nonoperative management of pelvic gunshot wounds. Am J Surg. 2011;201(6):784-8. https://doi.org/10.1016/j.amjsurg.2010.03.014. [ Links ]
39. Peponis T, Kasotakis G, Yu J, et al. Selective nonoperative management of abdominal gunshot wounds from heresy to adoption: a multicenter study of the research consortium of New England centers for trauma (ReCoNECT). J Am Coll Surg. 2017;224(6):1036-45. https://doi.org/10.1016/j.jamcollsurg.2016.12.055. [ Links ]
40. Saar S, Jorgensen J, Lemma AN, et al. Selective nonoperative management of penetrating abdominal injuries at Northern European trauma centers: the NordiPen Study. Eur J Trauma Emerg Surg. 2022;48(3):2023-7. https://doi.org/10.1007/s00068-021-01749-2. [ Links ]
 Correspondence:
Correspondence:
P Navsaria
Email: pradeep.navsaria@uct.ac.za














