Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.62 n.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00214
TRAUMA
Biochemical markers in emergency thoracic surgery in penetrating trauma
M Lubout; J Goosen; D Kruger; P Fru; S Makhadi; MS Moeng
Department of Surgery, School of Clinical Medicine, Faculty of Health sciences, University of the Witwatersrand, South Africa
ABSTRACT
BACKGROUND: Violent interpersonal acts account for a large proportion of unnatural deaths in South Africa. A significant proportion of unnatural deaths are due to penetrating thoracic trauma and preventable haemorrhage. Current indications for emergent thoracotomy are unreliable. We propose the use of lactate, shock index (SI) and base deficit (BD) as a triage tool in patients with penetrating thoracic injuries to identify those requiring surgical intervention
METHODS: A review of the trauma registry of the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) was carried out between March 2011 and March 2016. Four hundred and ninety (490) patients were collected consisting of a non-operative group of 246 patients and an operative group of 244 patients. We compared lactate, SI and BD independently and within panels to ascertain which would best predict the need for operative intervention in these patients. Abnormal was defined as lactate > 4 mmol/l, SI > 0.8 and BD < -4 mmol/l
RESULTS: Of the 490 patients, lactate (p < 0.001), SI (p < 0.001) and BD (p < 0.001) differed significantly between operative and non-operative groups. Statistical significance was lost (p = 0.34) once BD was analysed in combination with lactate and SI. Lactate alone was a strong predictor of the need for intervention (area under the curve (AUC) = 0.814). The strongest predictor was a combined panel of lactate and SI (AUC = 0.8308, p < 0.001
CONCLUSION: Lactate and SI in combination are useful as triage tools, and could assist in decision making, by predicting which patients are more likely to require surgical intervention
Keywords: biomarkers, emergency thoracic surgery, penetrating trauma
Introduction
Trauma is one of the leading causes of death and disability internationally.1 Penetrating thoracic trauma has a mortality rate that ranges from 20-25%. Although most penetrating chest trauma can be managed non-operatively by the insertion of an intercostal drain (ICD),23 penetrating chest trauma is responsible for approximately half of all traumatic deaths secondary to penetrating trauma.2 Approximately 10-30% of thoracic trauma patients require an immediate thoracotomy to control haemorrhage.3-6 Various controversies exist regarding operative intervention versus observation of these patients.4-7
This study sought to investigate whether the use of biomarkers, specifically lactate levels of > 4mmol/L and base deficit (BD) < -4 mmol/L together with a shock index (SI) of > 0.8 could predict the need for surgical intervention in penetrating thoracic trauma patients. These cut-off values were chosen after scrutiny of the literature.8-22 Predicting surgical intervention early would decrease the time to intervention and reduce delays.
Methods
The study was a quantitative retrospective analysis of a prospectively collected database at the trauma unit at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), South Africa. Patients presenting to the unit between 1 March 2011 and 31 March 2016 with penetrating thoracic injuries who were classified as priority 1 (P1) patients (including those who died before and after intervention) were included. Patients were grouped according to those requiring surgical intervention and those managed non-operatively with an ICD or suturing. All patients with significant penetrating chest injuries who required resuscitation were included.
Standard protocol in the unit dictates that all penetrating thoracic trauma with haemodynamic instability or evidence of chest wall penetration be admitted to the resuscitation area as P1. Hemodynamic instability was defined as systolic blood pressure (SBP) less than 90 mmHg. Demographic characteristics and vital signs, including SBP, pulse rate, respiratory rate (RR), Glasgow Coma Scale (GCS), and arterial blood gas findings, including pH, lactate, BD, and haemoglobin level, were recorded. These vital signs and blood samples were taken on arrival in the resuscitation area. From these, SI was calculated by dividing heart rate (HR) by SBP. Obvious cardiac injuries as in cardiac tamponade, air embolism and major tracheobronchial injuries were excluded as they required urgent surgical intervention. Thoracoabdominal injuries with abdominal visceral injuries and patients with significant incomplete data were also excluded.
The sample size of 491 patients consisted of 246 requiring an emergency operative intervention and a matching non-operative group of 245 consecutive patients with penetrating thoracic injuries managed conservatively. Non-operative interventions included ICD insertion, suturing of wounds in the emergency department and observation with a repeat chest x-ray after six hours. Other parameters captured included the need for and type of surgical and non-surgical intervention, time to surgical intervention, and operative findings at outcome.
Statistical analysis
An estimated sample size of 207 participants per group was calculated to be sufficient for a significance level (alpha) of 0.05 and power of 90% (ratio control vs experiment of 1) to show a 20% difference between the groups for a two-sample t-test.
The study variables were captured into a Microsoft Excel spreadsheet and imported into STATA Version 14.2 suit of analytics software. Descriptive statistics were conducted, and the Shapiro-Wilk test was performed to determine the normality of distribution of the data. Non-parametric Mann-Whitney U tests were performed, as appropriate, to determine differences in continuous variables between the groups (Table I) and mean (±SD) or median and range reported. The Fisher's exact tests were conducted to analyse categorical variables between the groups (Table II), and the results are expressed as absolute and relative frequencies. Significance was set at 5%. Univariate and multivariate logistical regression analyses were conducted for prediction model building in Table III, and only variables with p-values < 0.20 in the univariate analyses were included in multivariate model building.
The Hosmer-Lemeshow (HL) test was applied to determine the goodness-of-fit of the combined marker panels in multivariate models, with the highest p-value and lowest HL chi2 indicating the best-fit model for this dataset. Receiver operating characteristic (ROC) curve analysis was conducted, and the area under the curve (AUC) was reported to determine the ability of the individual variables or combined variable panels to predict surgical intervention accurately.
Results
Table I shows demographic and biochemical data collected from the non-intervention (n = 245) and intervention groups (n = 246). The mean age of the study population was 29.1 years (15-64 years), with no significant age differences between the two groups. A marked male predominance was noted (468/491, 95.1%).
Despite significant differences in the mean SBP and HR values between the intervention and non-intervention groups (110 mmHg vs 133 mmHg and 95 bpm vs 87 bpm, respectively), these levels still fell within what is considered the "normal" range for these vital signs. Moreover, these parameters were well above the cut-off levels where vital signs alone would prompt immediate surgical intervention according to current guidelines, i.e., SBP < 90 mmHg and HR > 120 bpm.3
Statistically significant differences between the nonintervention and intervention groups were also noted for GCS, haemoglobin, lactate, BD, pH and SI. Furthermore, when these parameters were categorised according to internationally recognised cut-off values in trauma patients, significant differences between the groups remained very strong (p-values < 0.0001; Table I).
When the types of penetrating injuries sustained were further classified into stab or gunshot wounds (GSW), most traumatic thoracic injuries encountered were found to result from stab wounds, a trend seen in both groups. However, the intervention group had a significantly higher proportion of GSW (20.8%) compared to the non-intervention group (6.9%), most likely due to the higher kinetic energy transfer involved with GSW causing more significant injury.12,22
The surgical intervention rate was 22% yearly, which is similar to international averages of approximately 10-30%.6,23 Table IV outlines the surgical interventions undertaken.
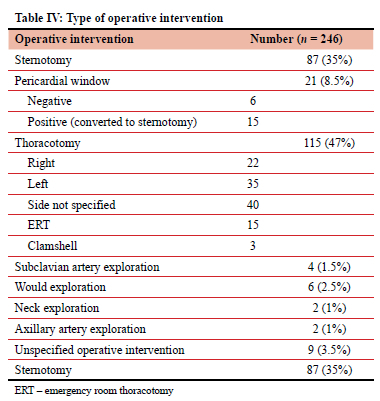
Sternotomies (n = 102, 42%) and thoracotomies (n = 97, 40%) formed the bulk of the procedures. Patients who underwent a pericardial window were subdivided into those with a positive window who went on to have a sternotomy and those with a negative pericardial window who did not.
Of the 246 patients who underwent an operative intervention, 159 (65%) were operated within two hours of presentation, 61 (25%) within two to four hours, 11 (4%) within four to six hours, 13 (5%) more than six hours after presentation and two (1%) patients had no recorded time to intervention.
A logistical regression analysis (summarised in Table III) was performed to further establish, which parameters would be more reliable when predicting the need for surgical intervention in penetrating thoracic trauma.
Haemoglobin and GCS were unreliable as early predictors of surgical intervention (Table III) when the AUC are compared (3-7, 22-25). BD, lactate, and SI showed the strongest statistical significance individually, with good AUC and good fitting of the data between the groups. According to the Hosmer-Lemeshow test, lactate was the only parameter to achieve an AUC of > 0.8 and the best goodness-of-fit (AUC = 0.814; HL chi2 = 5.98, p = 0.65).
Lactate, BD and SI were then grouped in different combinations to ascertain which panel would best predict operative intervention using multivariate logistic regression (Table V, Figure 1). When BD was grouped with lactate and SI or lactate alone, its statistical significance within the panel deteriorated significantly (p = 0.34 and 0.23, respectively).
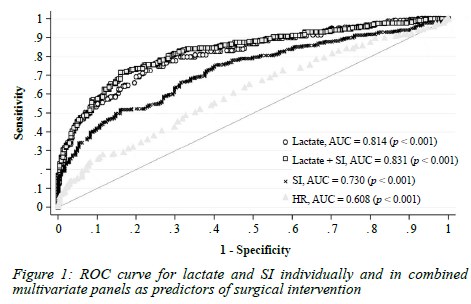
Although the panel of lactate-BD-SI achieved the highest AUC of 0.833, the Hosmer-Lemeshow test showed it was a relatively poor fit to the data (HL chi2 = 7.55, p = 0.48). Furthermore, when BD was combined with SI alone, the AUC dropped below 0.8. With BD excluded, the lactate-SI panel was found to be the most reliable combination of parameters for the prediction of operative intervention (AUC = 0.831; HL chi2 = 5.91, p = 0.66) with a sensitivity of 68.8%, a specificity of 84.1%, a positive predictive value of 80.9% and a negative predictive value of 72.37%, overall, correctly classifying 76.5% of patients.
Assuming the other markers in the panel remained constant, the effect of the odds (of operative intervention) of a single-unit increase in lactate is 1.73, meaning the odds of having an operative intervention increase of 73%. The effect of the odds of a 1-unit increase in SI is 7.45, meaning the odds of an operative intervention are approximately seven times more likely.
When specific cut-off values of lactate > 4mmol/L and SI > 0.8 were introduced, a sensitivity and specificity of 57.50% and 86.94%, respectively, and positive and negative predictive values of 81.18% and 67.62%, respectively, were calculated, correctly classifying 72.4% of patients. Analysis of the odds ratio revealed that lactate > 4 and SI > 0.8 increased the odds of operative intervention by eight times compared to patients with values within normal limits (Table VI).
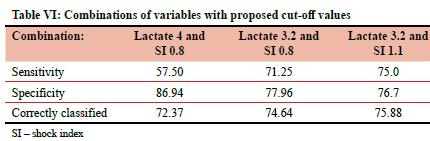
By scrutinising the ROC analysis, cut-off values of lactate >3.2 and SI of> 1.1 (sensitivity = 75.0%, specificity = 76.7%, negative predictive value = 75.81%, positive predictive value = 75.9%) provided the highest overall predictive value of operative intervention and in combination correctly identify 75.88% of patients requiring surgery.
Even so, using clinical judgement and previously prescribed indications, 65% of patients underwent surgical intervention within the first two hours of presentation. Using the above cut-off values, which are easily at hand and available within minutes, would have increased the identification of patients needing surgical intervention.
Additionally, all patients in the non-operative group survived. Our data suggest that patients who met any two or all three specified criteria were also more likely to succumb to their injuries despite intervention, whether early or late, compared to those who met one or fewer criteria (p < 0.001). Further study of this aspect is required as the number of patients whose outcomes were recorded was not sufficient to comment on this reliably.
Discussion
Listed below are the current indications for thoracotomy as stated by Advanced Trauma Life Support (ATLS)®.3 These include the ongoing haemodynamic instability, immediate significant drainage and ongoing evidence of bleeding as well as specified organ injuries that may threaten the life. Surgery is required in 30% of penetrating thoracic injuries compared to 10% in blunt trauma.3-6
The premise of the above indications is based on observations made during the Vietnam War in the early 1970s.4-6 Findings showed that the risk of death increases linearly with total chest haemorrhage after thoracic injury and that mortality was three times higher with an output of >1500 mL of blood compared to that of 500 mL.6 Early performance of emergency thoracotomy resulted in a decrease in mortality.4-6,22
Considering the many controversies regarding operative intervention versus observation of patients who have sustained penetrating thoracic trauma, the absolute volume of intra-pleural drainage as an indication for thoracotomy is unreliable.4-6 Multiple factors may influence the volume of drainage. Abnormal vital signs signifying haemodynamic instability are late shock indicators.22-26
Much of the earlier literature surrounding the use of biomarkers in trauma focused on their use to predict endpoints such as death, admission to ICU or the need for massive transfusion.11,13,15-19
Although several studies have analysed the use of biomarkers such as lactate and BD as predictors of high-risk trauma patients and to assist with the diagnosis of occult shock,8-18 only a few refer to the use of lactate and BD in decision-making regarding operative intervention.8,18,20
Caputo et al. in 2013 noted no difference in vital signs and BD between operative and non-operative trauma patients but a significant difference in lactate levels.8 Patients with elevated lactate were more likely to require operative intervention.8 In a study consisting of patients with blunt and penetrating thoracic trauma, Parsikia et al. reported that lactate was a better predictor of operative intervention than vital signs with a p = 0.033 and AUC of 0.608.27 Caputo et al. evaluated serum lactate, anion gap and base deficit's predictive value for massive transfusion and operative intervention.10 Lactate and BD were comparable for the prediction of surgical intervention with an AUC of 0.62 and 0.67, respectively. As with their 2013 study, the study group included trauma patients with blunt and penetrating injuries to multiple body regions, including the chest and abdomen.
Our study supports the above studies regarding the use of lactate as a tool to assist in identifying the need for operative intervention in penetrating thoracic trauma. It provides compelling evidence of its predictive value, which is improved further when combined with the shock index.
Despite reported reliability issues from lactate and BD as predictive tools in the diagnosis of shock resulting from alcohol consumption,21,28-30 the study showed a statistically significant difference between the non-intervention group and the intervention group with both lactate and BD individually (p < 0.001).
While lactate proved to be a strong parameter both alone and in combination with SI, the same could not be said for BD. Given that up to 66% of our trauma population are under the influence of alcohol on presentation, the possibility of alcohol influencing reliability cannot be ruled.28
Limitations
Considering that this was a retrospective study, there are limitations such as selection bias and the fact that the value of the data relies upon the accuracy of its collection in the past. Additionally, the single centre may not be illustrative of the more general population. The exclusion of some cases that required emergency room thoracotomy (ERT) may have skewed the findings. Furthermore, the study only included penetrating thoracic trauma; therefore, no inferences can be made for blunt trauma or trauma involving other body regions. Development and validation samples could have been used to evaluate the derived models.
Conclusion
This study highlights the usefulness of lactate and SI as triage tools in P1 patients with penetrating thoracic trauma. Although strict universal cut-off values of lactate and SI do not identify those patients requiring surgical intervention with 100% certainty, they improve the accuracy in identifying those patients at higher risk in a timely manner.
Future studies
A prospective multicentre study should be conducted to validate our findings. With no consensus regarding the effect of alcohol on lactate and whether this influences its reliability as a triage tool, further investigation into the effect of alcohol on blood gas parameters, such as lactate and BD, is needed.31
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval was obtained from the University of the Witwatersrand Hurman Research Ethics Committee (M160463).
ORCID
M Lubout https://orcid.org/0009-0004-2485-4235
J Goosen https://orcid.org/0000-0003-1297-7110
D Kruger https://orcid.org/0000-0002-3604-7682
P Fru https://orcid.org/0000-0002-3631-1893
S Makhadi https://orcid.org/0000-0003-3381-5866
MS Moeng https://orcid.org/0000-0001-7459-3388
REFERENCES
1. Sakran JV, Greer SE, Werlin E, McCunn M. Care of the injured worldwide: trauma still the neglected disease of modern society. Scand J Trauma Resusc Emerg Med. 2012;20(1):1-1. https://doi.org/10.1186/1757-7241-20-64. [ Links ]
2. Van Waes OJF, Van Riet PA, Van Lieshout EMM, Hartog DD. Immediate thoracotomy for penetrating injuries: ten years' experience at a Dutch level I trauma centre. Eur J Trauma Emerg Surg. 2012;38(5):543-51. https://doi.org/10.1007/s00068-012-0198-6. [ Links ]
3. Kithuka CM, Ntola VC, Sibanda W. An audit of traumatic haemothoraces in a regional hospital in KwaZulu-Natal, South Africa. S Afr J Surg. 2023;61(3):12-16. https://doi.org/10.36303/SAJS.3986. [ Links ]
4. Degiannis E, Loogna P, Doll D, et al. Penetrating cardiac injuries: recent experience in South Africa. World J Surg. 2006;30(7):1258-64. https://doi.org/10.1007/s00268-005-0463-5. [ Links ]
5. Makhadi S, Moeng MS, Ede C, Jassat F, Palweni ST. Penetrating cardiac injuries: outcome of treatment from a level 1 trauma centre in South Africa. Trauma Care. 2022;2(2):251-9. https://doi.org/10.3390/traumacare2020021. [ Links ]
6. Karmy-Jones R, Jurkovich GJ, Nathens AB, et al. Timing of urgent thoracotomy for haemorrhage after trauma: a multicentre study. Arch Surg. 2001;136(5):513-8. https://doi.org/10.1001/archsurg.136.5.513. [ Links ]
7. Demetriades D, Velmahos GC. Penetrating injuries of the chest: indications for operation. Scand J Surg. 2002;91(1):41-5. https://doi.org/10.1177/145749690209100107. [ Links ]
8. Caputo N, Fraser R, Paliga A, et al. Triage vital signs do not correlate with serum lactate or base deficit and are less predictive of operative intervention in penetrating trauma patients - a prospective cohort study. Emerg Med J. 2013;30(7):546-50. https://doi.org/10.1136/emermed-2012-201343. [ Links ]
9. Caputo ND, Kanter M. A proposed novel algorithmic approach to the evaluation of the acutely injured trauma patient: should advanced trauma life support incorporate biomarkers? Am J Emerg Med. 2014;32(3):282-4. https://doi.org/10.1016/j.ajem.2013.11.048. [ Links ]
10. Caputo ND, Kanter M, Fraser R, Simon R. Comparing biomarkers of traumatic shock - the utility of anion gap, base excess, and serum lactate in the ED. Am J Emerg Med. 2015;33(9):1134-9. https://doi.org/10.1016/j.ajem.2015.04.085. [ Links ]
11. Choi JY, Lee WH, Yoo TK, Park I, Kim DW. A new severity predicting index for haemorrhagic shock using lactate concentration and peripheral perfusion in a rat model. Shock. 2012;38(6):635-41. https://doi.org/10.1097/SHK.0b013e318273299f. [ Links ]
12. Remick K, Dickerson JA, Cronk D, Topolski R, Nessen SC. Defining and predicting surgeon utilisation at forward surgical teams in Afghanistan. J Surg Res. 2012;177(2):282-7. https://doi.org/10.1016/j.jss.2012.07.022. [ Links ]
13. Kruse O, Grunnet N, Barfod C. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: a systematic review. Scand J Trauma Resusc Emerg Med. 2011;19(1):74. https://doi.org/10.1186/1757-7241-19-74. [ Links ]
14. Guyette FX, Meier EN, Newgard C, et al. A comparison of prehospital lactate and systolic blood pressure for predicting the need for resuscitative care in trauma transported by ground. J Trauma Acute Care Surg. 2015;78(3):600-6. https://doi.org/10.1097/TA.0000000000000549. [ Links ]
15. Okello M, Makobore P, Wangoda R, Upoki A, Galukande M. Serum lactate as a predictor of early outcomes among trauma patients in Uganda. 2014;1-9. https://doi.org/10.1186/s12245-014-0020-9. [ Links ]
16. Kotanen CN, Guiseppi-Elie A. Monitoring systems and quantitative measurement ofbiomolecules for the management of trauma. Biomed Microdevices. 2013;15(3):561-77. https://doi.org/10.1007/s10544-013-9756-x. [ Links ]
17. Okorie ON, Dellinger P. Lactate: biomarker and potential therapeutic target. Critical Care Clinics. 2011;27(2):299-326. https://doi.org/10.1016/j.ccc.2010.12.013. [ Links ]
18. Vandromme MJ, Griffin RL, Weinberg JA, Rue LW, Kerby JD. Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg. 2010;210(5):861-7. https://doi.org/10.1016/j.jamcollsurg.2010.01.012. [ Links ]
19. Barfod C, Lundstram LH, Lauritzen MMP, et al. Venous blood lactate on admission is a predictor for in-hospital cardiac arrest: an observational cohort study. Resuscitation. 2012;83:e27-8. https://doi.org/10.1016/j.resuscitation.2012.08.069. [ Links ]
20. Paladino L, Sinert R, Wallace D, ET AL. The utility of base deficit and arterial lactate in differentiating major from minor injury in trauma patients with normal vital signs. Resuscitation. 2008;77(3):363-8. https://doi.org/10.1016/j.resuscitation.2008.01.022. [ Links ]
21. Davis JW, Kaups KL, Parks SN. Effect of alcohol on the utility of base deficit in trauma. J Trauma. 1997;43(3):507-10. https://doi.org/10.1097/00005373-199709000-00020. [ Links ]
22. Clarke D, Quazi MA, Reddy K, Thompson SR. Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. Journal of Thoracic and Cardiovascular Surgery. 2011;142(3):563-8. https://doi.org/10.1016/j.jtcvs.2011.03.034. [ Links ]
23. Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma-a review. Injury. 2006;37(1):1-19. https://doi.org/10.1016/j.injury.2005.02.014. [ Links ]
24. Beattie R, Mhandu PCE, McManus K. Penetrating thoracic trauma. Surgery. 2014;32(5):249-53. https://doi.org/10.1016/j.mpsur.2014.02.008. [ Links ]
25. Bastos R, Baisden CE, Harker L, Calhoon JH. Penetrating thoracictrauma.SeminThoracCardiovascSurg.2008;20(1):19-25. https://doi.org/10.1053/j.semtcvs.2008.01.003. [ Links ]
26. Soller B, Zou F, Prince MD, Dubick MA, Sondeen JL. Comparison of noninvasive ph and blood lactate as predictors of mortality in a swine haemorrhagic shock with restricted volume resuscitation model. Shock. 2015;44:90-5. https://doi.org/10.1097/SHK.0000000000000307. [ Links ]
27. Parsikia A, Bones K, Kaplan M, et al. The predictive value of initial serum lactate in trauma patients. Shock. 2014;42(3):199-204. https://doi.org/10.1097/SHK.0000000000000208. [ Links ]
28. Gustafson ML, Hollosi S, Chumbe JT, Samanta D, Modak A, Bethea A. The effect of ethanol on lactate and base deficit as predictors of morbidity and mortality in trauma. Am J Emerg Med. 2015;33(5):607-13. https://doi.org/10.1016/j.ajem.2015.01.030. [ Links ]
29. Zehtabchi S, Baron BJ, Sinert R, Yadav K, Lucchesi M. Ethanol and illicit drugs do not affect the diagnostic utility of base deficit and lactate in differentiating minor from major injury in trauma patients. Acad Emerg Med. 2004;11(10):1014-20. https://doi.org/10.1111/j.1553-2712.2004.tb00669.x. [ Links ]
30. Dunne JR, Tracy JK, Scalea TM, Napolitano LM. Lactate and base deficit in trauma: does alcohol or drug use impair their predictive accuracy? J Trauma. 2005;58(5):959-66. https://doi.org/10.1097/01.TA.0000158508.84009.490 [ Links ]
 Correspondence:
Correspondence:
S Makhadi
Email: sm61459@gmail.com














