Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.62 n.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00213
TRAUMA
The sensitivity of a neck CT scan in detecting pneumothoraces in nonpenetrating trauma
R ByebwaI; EE NwekeI; MS MoengI, II
IDepartment of Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, South Africa
IICharlotte Maxeke Johannesburg Academic Hospital, South Africa
ABSTRACT
BACKGROUND: The trauma-related pneumothorax is a common intrathoracic injury and can go undetected with detrimental outcomes. Chest computed tomography (CT) investigation in low- to middle-income countries (LMIC) is not always readily available during emergency situations and increased workloads. However, alternative investigations all have limitations in including pneumothoraces. Patients may have trauma indications for CT of the head and neck. The neck CT scan may hold an extra potential advantage in pneumothorax detection. This study aimed to assess its sensitivity in pneumothorax detection in nonpenetrating trauma
METHODS: A retrospective study was conducted from 1 January 2016 to 31 December 2021. All adult patients sustaining nonpenetrating injuries, and investigated with chest and neck CT scans were included. The chest CT scan was the gold standard against,which the neck CT scan was compared to determine the accuracy of pneumothorax detection. Stata version 16 was used for descriptive statistical analysis, and a _p-value of 0.05 was considered statistically significant
RESULTS: One thousand ninety three were eligible for evaluation; 204 (18.66%) pneumothoraces were detected on chest CT scans, 200 (98.0%) of which were also detected on the neck CT scan, producing a sensitivity of 98.0% (95% CI 95.1-99.5%) and a specificity of 100% (95% CI 99.6-100%). Most pneumothoraces were detected at T1 level (45.09%), followed by T2 (43.62%
CONCLUSION: The neck CT scan has demonstrated high sensitivity and specificity in pneumothorax detection. Thus, it may be used as an additional tool for those who could not receive or do not need a formal chest CT but have an indication for neck CT scans
Keywords: trauma, nonpenetrating, CT Chest, neck CT, C-spine CT, sensitivity
Introduction
Trauma-related morbidity and mortality are important contributors to the mortality afflicting many individuals during the most productive years of their lives,1-3 contributing to a significant loss of income while adding to health expenditure and reducing productive capacity. As much as 25% of polytrauma deaths are attributable to chest injuries, and 10-13.6% of these patients have pneumothoraces.4-8 An audit of trauma deaths in Scottish emergency units revealed that misdiagnosis of thoracic injuries and delays in instituting appropriate treatment were the most common errors contributing to death.
The erect chest x-ray (CXR) is an inexpensive and sensitive investigation used to detect pneumothoraces;10 however, most trauma victims are relegated to the supine position due to therapeutic necessity.9 The supine CXR has a sensitivity between 30-50% in pneumothorax detection.10,11 Additionally, identifying the subtleties of pneumothoraces can be challenging. An occult pneumothorax is a pneumothorax missed during initial plain radiological studies and identified on cross-sectional imaging of the chest.12 Since most trauma patients are investigated with supine CXRs, which have a low sensitivity in detecting pneumothoraces, which are then later detected on cross-sectional imaging, one can surmise that some of the pneumothoraces are occult.
The CXRs at this facility are not reported on by the radiologist but are interpreted by the treating clinician. In this study the CXRs were interpreted by a registrar supervised by an in-house trauma consultant.
Ultrasound scan is a more sensitive investigation than the supine CXR;4,13 it can be performed serially and without relocating the patient from the safety of the resuscitation room. However, the image evaluation is subjective, is often difficult to corroborate on retrospective evaluation, and may give irreproducible results, particularly with subtle pathology.14 High healthcare turnover units may have challenges with the repeatability of findings utilising this modality.
The chest computed tomography (CT) scan is the gold standard investigation for pneumothorax detection, with a sensitivity and specificity approaching 100%.5,15 The CT scan produces objective and reproducible results and has the distinct advantage of identifying other thoracic and upper abdominal injuries. Appropriate use of chest CT scans in trauma patients has increased, partly due to the low sensitivity of the supine CXR and the subjectivity of the bedside ultrasound scan. However, the chest CT scan is associated with relatively high-doses of radiation and higher costs,16,17 with minimal benefit in those who do not require a chest CT scan.
A CT scan of the head and neck is performed in many patients sustaining blunt trauma to the head, neck, and chest to evaluate the bony structures and assess for blunt cerebral vascular injury, thus requiring visualisation of the aortic arch. The axial slices of the neck CT scan conventionally extend to T4 level18 at the level of the aortic arch. They could be used to evaluate the cephalad portion of the thorax for pneumothoraces with more sensitivity and specificity than a supine CXR or a cervical spine CT scan and more objectivity than an ultrasound scan, but without extending to a chest CT scan in patients not requiring the additional imaging. The outcome of this investigation may prompt an intervention, such as insertion of an intercostal drain, further investigations or cautious observation.
Ball et al. noted that most pneumothoraces in supine patients were located in the anterior pleural space.7,11 Logically, air would accumulate in the most anterior part of the pleural space due to its density relative to the adjacent pleural contents. However, when assessing hundreds of chest CT scans in our trauma unit, we observed that nearly all pneumothoraces were detected in the cephalad portion of the thorax at levels T1-T2 and not usually in the anterior pleural space (Figure 1). Most of the pneumothoraces we detected could be seen in the standard protocol neck CT scan, which extends to the aortic arch (Figure 1).
The availability of radiologists is not always guaranteed, and clinicians have had to learn to interpret basic radiology to provide therapeutic interventions during emergencies.
We hypothesised that the neck CT scan could be an accurate modality of diagnosing pneumothoraces, thus adding an extra window to evaluate the injured. The study aims to evaluate the sensitivity of neck CT in assessing pneumothoraces in nonpenetrating trauma patients presenting at a busy trauma unit in Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) in South Africa.
The primary objective was to compare the detection of pneumothoraces on neck CT with chest CT. A secondary objective was to evaluate the detection of pneumothorax of neck CT with supine CXR.
Methods
A descriptive retrospective study was conducted at CMJAH between 1 January 2016 and 31 December 2021.
The chosen facility houses an equivalent Level 1 trauma centre, seeing more than 16 000 trauma patients annually.19 The data was gathered from the IntelliSpace PACS (Picture archiving and communication system) Enterprise version 4.4 radiological database. All patients aged over 18 years sustaining nonpenetrating trauma to the head, neck, or torso, investigated with a neck CT scan and a separate chest CT scan, and with images reported on by a consultant radiologist were included. Demographics (including age and sex) and the mechanism of the blunt trauma were documented. The "other" category was created to encompass infrequently encountered blunt injury mechanisms, such as a gate or boulder falling on a patient, train surfing or motorbike collisions.
The radiology reports were evaluated to identify the trauma mechanism and to obtain patient demographics. These reports additionally provided independent confirmation of a pneumothorax in the chest CT scan. We then compared the radiological images of the neck CT scans with those of the chest CT scans in the group of patients confirmed to have pneumothorax in the radiologist's report. We compared whether the pneumothorax observed on the chest CT scan could be detected on the independent neck CT scan. Neck CT scans that extended below the T4 level were excluded from further analysis as they would overestimate the findings. Our protocol allows neck scans for the spine or soft tissues to extend past T1 towards the T4 level.
Using the axial, coronal, and sagittal views of the neck and chest CT scans, as well as the marking tools available on the IntelliSpace PACS Enterprise version 4.4 radiological software, we confirmed the presence of a pneumothorax using the lung window. We marked the most cephalad portion of the collapsed lung. By alternating with the bone window while maintaining the location of the pneumothorax, we identified the thoracic vertebral level at which most pneumothoraces could be detected.
The secondary objective was to compare the neck CT with spine scan findings to the CXR. To achieve this, we reviewed the CXR images performed on the same day as the neck CT scan. In the group of patients, in which the CT scan demonstrated a pneumothorax, we assessed the CXR to confirm whether the pneumothorax detected on the neck CT scan was also detected on the CXR (Figure 2).
Statistical analysis
Key data points were analysed using the Stata statistical package edition 16.0, which included specificity, sensitivity, and positive and negative predictive values. Normally distributed data were reported as means and compared using the Shapiro-Wilk test. Categorical variables were analysed with Fisher's exact test. A comparison of positive and negative outcomes was performed using the chi-square test. The accepted level of significance was a p-value of < 0.05.
Results
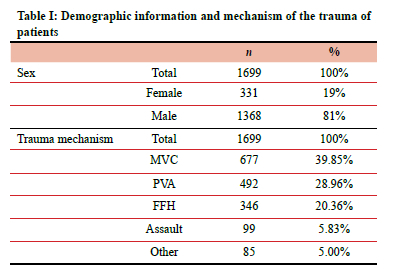
A total of 1699 patient reports and radiological studies were reviewed. Ofthese patients, mostwere male (81%, 1368/1699; Table I). The median age was 33 years (96% confidence interval [CI] 28-39); this median age is representative of the study population.19,20 The most common trauma mechanism was motor vehicle collisions (MVC), accounting for 39.85% of all trauma mechanisms, followed by pedestrian-vehicle accidents (PVA), accounting for 28.96% of injuries and fall from heights (FFH), accounting for 20.36% of injuries. Blunt assault comprised 5.83% of all trauma mechanisms. All patients were investigated with chest and neck CT scans. These investigations were performed simultaneously as part of a pan CT scan and uploaded as individual components; the neck CT scan was separately uploaded to the chest CT scan (Table I).
Of the 1699 patients assessed in this data series, 606 (35.6%) had neck CT scans that extended beyond the T4 level (Figure 3). We believed these CT scans were unrepresentative of the standard neck CT scan guidelines18 and would skew the results, so this data was excluded from the study. Of the 1093 patients who could be evaluated, most neck CT scans extended to the T4 level (52.61%), followed by the T3 level (40.35%); 6.22% of neck CT scans extended to the T2 level and 0.64% to the T1 level.
On chest CT scans, 204 (18.66%) pneumothoraces were detected. Of the 204 pneumothoraces observed on chest CT scans, 200 (98.0%) were also detected on neck CT scans. The neck CT scan had a sensitivity of 98.0% (95% CI 95.199.5%), a specificity of 100% (95% CI 99.6-100%; Table II), and a p-value of 0.1250, indicating no significant difference between chest and neck CT scans in pneumothorax detection.
Most pneumothoraces were detected at T1 level (45.09%), followed by T2 (43.62%), and a small fraction of pneumothoraces was detected at levels T3 (7.84%) and T4 (1.96%).
The secondary objective of this study was to determine how the neck CT scan compared to the supine CXR in pneumothorax detection. Of the 1093 patients evaluated, all had CXRs. Of the 200 pneumothoraces detected on CT, all had CXRs performed in the supine position. Of the 200 patients with pneumothoraces on neck CT scans, 17 also had pneumothoraces on supine CXRs, producing a sensitivity of 23% (95% CI 20.1-26.1%). Notably the CXR had a positive predictive value of 91.5% (95% CI 86.7-95%; Table II). This data supports the hypothesis that the CT scan of the neck is a sensitive and specific tool in detecting pneumothoraces and demonstrates the positive predictive value of the supine CXR in detecting pneumothoraces.
Discussion
While evaluating the utility of the neck CT scan in pneumothorax detection, Ball et al. concluded that this modality was sufficiently accurate to confidently exclude all pneumothoraces, not only occult ones.7,11 However, this finding was disputed by Akoglu et al., whose data revealed that the neck CT scan, which conventionally extends to the T1 level, can miss up to 26% of patients with trauma-related occult pneumothoraces.18,20 The data from this research revealed that a CT scan performed to the T1 level could detect as much as 45.09% but miss the remaining 54.91%.
Based on our preliminary analysis of chest CT scans in trauma victims, our hypothesis confirmed that most pneumothoraces were detected cephalad to T4 level. Akoglu et al. highlighted that institutions use different CT scan protocols when performing CT scans of the C-spine. Ensuring that the protocol extends to the T4 level would enhance the detection rate of pneumothoraces. This is true for contrast neck CT scans where the aortic arch must be included to allow visualisation of the origin of the cerebral circulation; therefore, most scans will extend caudally to but should not extend cephalad to the T4 level.
Our study used the standard radiology recommendation for a CT scan of the neck and soft tissue extending through the aortic arch, usually at thoracic level T4. Contrary to the report by Akoglu et al., we found that most pneumothoraces occurred in the most cephalad portion of the thorax and not in the anterior pleural space in supine patients.20 We discovered that most pneumothoraces could be detected with a CT scan extending to the T4 level with a sensitivity approaching 100%.
The data additionally confirmed previous data revealing the inaccuracy of supine CXR in pneumothorax detection. This investigation confirmed the superiority of the neck CT scans extending to the T4 level in pneumothorax detection compared to supine CXR and CT scans performed to the T1 level. The data revealed that supine x-ray has a high positive predictive value but low sensitivity in pneumothorax detection. This is in keeping with trauma studies and emphasises the challenges of getting erect CXR in trauma patients.21,22 Occult pneumothoraces were in 77% of those evaluated with CXR which was lower than reported by Omar.10
There is a disproportionate amount of penetrating trauma in South Africa, however this study focused on nonpenetrating head neck and torso trauma, with the objective to assess whether a CT scan of the neck, which would be done as part of an investigation for blunt cerebral vascular injury, could also identify most pneumothoraces. This hypothesis was based on the preliminary evaluation of CT scans, during which it was noted that most of the pneumothoraces that were detected were seen proximal to T4 level. The study findings are unlikely to alter management protocols because the CT scan chest provides additional important information with relatively little additional cost and is performed as part of a panscan.
The strength of this study lies in the simplicity of its methodology. It is easily reproducible, and future studies can be performed to expand further the clinical utility of all our current radiological studies. Future research can be conducted using a similar methodology to corroborate the findings of this research and explore the accuracy of the neck CT scan in detecting other pathologies traditionally investigated with a chest CT scan, such as haemothoraces.
Limitations of the study
This is a retrospective study from a single institution with the potential for bias. The ability and ease to view CT scanners on a monitor in this unit may not be transferrable to other units. Access to a functional PACS may not be available to all units. The findings may not apply to patients with extensive chest adhesions, as adhesions may hamper the pneumothorax distribution.
Conclusion
The neck CT scan is a sensitive investigation for detecting pneumothoraces; 98% of pneumothoraces can be detected using this investigation, provided that the neck CT protocol extends to T4. Although the supine CXR has low sensitivity in pneumothorax detection, it may still have a role as an adjunct due to its high positive predictive value. In patients sustaining nonpenetrating trauma and investigated with a neck CT scan, this investigation could minimise the possibility of a missed pneumothorax. The findings, however, should not negate the need for a chest CT scan in cases where it is clinically indicated.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The University of the Witwatersrand Human Ethics Committee reviewed the study protocol and approved (Ref: M211193).
ORCID
R Byebwa https://orcid.org/0009-0000-8609-6784
EE Nweke https://orcid.org/0000-0003-4026-1697
MS Moeng https://orcid.org/0000-0001-7459-3388
REFERENCES
1. Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health. 2000;90(4):523-6. https://doi.org/10.2105/AJPH.90.4.523. [ Links ]
2. Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;85(9):696-702. https://doi.org/10.2471/BLT.06.037184. [ Links ]
3. Moran CG, Lecky F, Bouamra O, et al. Changing the system - major trauma patients and their outcomes in the NHS (England) 2008-17. EClinicalMedicine. 2018;2(3):13-21. https://doi.org/10.1016/j.eclinm.2018.07.001. [ Links ]
4. Rowan KR, Kirkpatrick AW, Liu D, et al. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT - initial experience. Radiology. 2002;225(1):210-4. https://doi.org/10.1148/radiol.2251011102. [ Links ]
5. Tœkker M, Kristjánsdóttir B, Graumann O, Laursen CB, Pietersen PI. Diagnostic accuracy of low-dose and ultra-low-dose CT in detection of chest pathology: A systematic review. Clin Imaging. 2021;74:139-48. https://doi.org/10.1016/j.clinimag.2020.12.041. [ Links ]
6. Ball CG, Kirkpatrick AW, Laupland KB, et al. Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J Trauma. 2005;59(4):917-24. https://doi.org/10.1097/01.ta.0000174663.46453.86. [ Links ]
7. Ball CG, KirkpatrickAW, Laupland KB, et al. Factors related to the failure of radiographic recognition of occult posttraumatic pneumothoraces. Am J Surg. 2005;189(5):541-6; discussion 546. https://doi.org/10.1016/j.amjsurg.2005.01.018. [ Links ]
8. Bruce DA. Imaging after head trauma: why, when and which. Childs Nerv Syst. 2000;16(10):755-9. https://doi.org/10.1007/PL00013720. [ Links ]
9. Gordon MWG, Luke C, Robertson CE, Busuttil A. An audit of trauma deaths occurring in the accident and emergency department. Arch Emerg Med. 1989;6(2):107-15. https://doi.org/10.1136/emj.6.2.107. [ Links ]
10. Omar HR, Abdelmalak H, Mangar D, et al. Occult pneumothorax, revisited. J Trauma Manag Outcomes. 2010;4(1):2-7. https://doi.org/10.1186/1752-2897-4-12. [ Links ]
11. Ball CG, Kirkpatrick AW, Feliciano DV. The occult pneumothorax: What have we learned? Can J Surg. 2009;52(5):173-9. [ Links ]
12. De Moya MA, Seaver C, Spaniolas K, et al. Occult pneumothorax in trauma patients - development of an objective scoring system. J Trauma. 2007;63(1):13-7. https://doi.org/10.1097/TA.0b013e31806864fc. [ Links ]
13. Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5(1):76-81. https://doi.org/10.4103/0974-2700.93116. [ Links ]
14. lrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: A systematic review and meta-analysis. Chest. 2012;141(3):703-8. https://doi.org/10.1378/chest.11-0131. [ Links ]
15. Bhoil R, Kumar R, Kaur J, Attri PK, Thakur R. Diagnosis of traumatic pneumothorax: A comparison between lung ultrasound and supine chest radiographs. Indian J Crit Care Med. 2021;25(2):176-80. https://doi.org/10.5005/jp-journals-10071-23729. [ Links ]
16. American College of Radiology, Radiological Society of North America. Radiation dose to adults from common imaging examinations. Am Coll Radiol [Internet]. 2018;18. Available from: https://www.acr.org/-/media/ACR/Files/Radiology-Safety/Radiation-Safety/Dose-Reference-Card.pdf?la=en. [ Links ]
17. Proto AV. Radiology price list for imaging studies. Radiology. 2007;245(3):619-21. https://doi.org/10.1148/radiol.2453071685. [ Links ]
18. Vrad Standard Imaging Protocols - Radiologic. 2016;18. Available from: www.vrad.comhttps://www.scribd.com/document/440674686/vRad-Standard-Imaging-Protocols-pdf. [ Links ]
19. Bruce JC, Schmollgruber S, Eales J, Gassiep J, Doubell V. Injury surveillance at a level 1 trauma centre in Johannesburg, South Africa. Heal SA Gesondheid. 2003;8(3). https://doi.org/10.4102/hsag.v8i3.130. [ Links ]
20. Akoglu H, Akoglu EU, Evman S, et al. Utility of cervical spinal and abdominal computed tomography in diagnosing occult pneumothorax in patients with blunt trauma: Computed tomographic imaging protocol matters. J Trauma Acute Care Surg. 2012;73(4):874-9. https://doi.org/10.1097/TA.0b013e3182569ff2. [ Links ]
21. Brar MS, Bains I, Brunet G, et al. Occult pneumothoraces truly occult or simply missed: Redux. J Trauma. 2010;69(6):1335-7. https://doi.org/10.1097/TA.0b013e3181f6f525. [ Links ]
22. Platz J, Fabricant L, Norotsky M. Thoracic trauma: Injuries, evaluation, and treatment. Surg Clin N Am. 2017;97:783-99. https://doi.org/10.1016/j.suc.2017.03.004. [ Links ]
 Correspondence:
Correspondence:
MS Moeng
Email: maeyane.moeng@wits.ac.za














