Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.62 no.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00202
SURVEY
Post-traumatic stress disorder in international surgeons undertaking trauma electives in a South African trauma centre
V ThirayanI; VY KongII, III; H UchinoIV; DL ClarkeII, III
IMental Health and Addictions, Waikato Hospital, New Zealand
IIDepartment of Surgery, University of KwaZulu-Natal, South Africa
IIIDepartment of Surgery, University of the Witwatersrand, South Africa
IVTrauma Centre, Montreal General Hospital, Canada
ABSTRACT
BACKGROUND: Post-traumatic stress disorder (PTSD) is a well-documented psychiatric outcome in patients who experience physical trauma. The phenomenon is less studied in the staff involved in caring for such patients. The aim was to investigate the prevalence of PTSD in visiting international surgeons undergoing elective trauma training and to compare to local and international rates
METHODS: A trauma screening questionnaire (TSQ) survey was conducted among surgeons completing their elective trauma service placements in the Pietermaritzburg Metropolitan Trauma Service
RESULTS: Nineteen surveys were completed (32% response rate). Mean age was 38.9 (SD 6.5). Median postgraduate working experience was 5 (2-10) years. Median time of stay in South Africa was 6 (1-72) months. Compared to pre-elective experience, there was a five-fold increase in the level of trauma resuscitation experience reported during elective placement. 10.5% of surgeons scored > 5 in the TSQ suggesting probable PTSD. No statistical differences in age, years of prior experience, prior trauma rotation, number of major resuscitations, or length of stay in South Africa were observed in those scoring positive versus negative screening in the TSQ questionnaire
CONCLUSION: Despite being exposed to increased levels of trauma related injury, we observed low rates of positive screening for PTSD in our cohort of visiting international surgeons involved in elective trauma service placements. Investigation of potential protective factors against PTSD in this South African tertiary trauma centre is warranted
Keywords: post-traumatic stress disorder, PTSD, healthcare staff, surgeons, South Africa, mental health
Introduction
Post-traumatic stress disorder (PTSD) is a psychiatric condition in which the individual who has experienced a traumatic event develops several psychological symptoms, which persist for a month or longer following the initiating event. These symptoms include involuntary intrusion symptoms, avoidance behaviours, negative cognitions and mood, and hyperarousal symptoms. The triggering event can include directly experiencing or witnessing the traumatic event, learning it occurred to a close friend or family, or experiencing repeated exposure to aversive details of the event. The latter exposure may be work related. The symptoms of PTSD results in the patient experiencing functional impairment in both social and occupational life.1-3 Studies based on a national survey of general surgeons in the United States (US) recorded a PTSD rate of up to 17%, increasing to 40% among trauma specialists.4,5 Rates are significantly lower in gynaecologists (1.5%) and orthopaedic surgeons (0.3%).3,4 This suggests there is an association between PTSD and trauma work exposure. This is in keeping with the higher rates of PTSD observed in paramedics (4-21.5%) and firefighters (6-37%).6-8 These healthcare and emergency staff are frequently exposed to situations in which they will either be exposed to physical risk or repeatedly witness the effects of physical trauma. This is a risk factor for the development of PTSD.6,7,9
South Africa experiences a high burden of physical trauma and both the homicide and road traffic accident rates are much higher than those reported globally.10,11 In the general population, the South African Stress and Health Study identified a lifetime prevalence of PTSD of 2.3%, increasing to 3.5% following exposure to trauma.12 Among 1099 South African prehospital emergency service personal, rates of PTSD were 28%, 30%, 25% among surveyed ambulance, fire and traffic personnel, respectively. Approximately 30% of these staff had experienced an assault whilst on duty and 88.4% had experienced a critical event in the prior two months to the survey.13 A survey of 1859 South African anaesthetists following the death of a patient on the table identified a 28.8% probable diagnosis of PTSD.14 There is little data on the prevalence of PTSD amongst South African surgeons.
South Africa is a popular destination for international surgeons to obtain trauma experience not otherwise available in their home country. Uchino et al. demonstrated that a one-year trauma elective at their institution allowed international surgeons to gain experience that would otherwise require a much longer period of time to acquire in their countries of domicile.15 Gaining such clinical experience may be associated with an increased risk to mental health secondary to witnessing trauma-related physical injury in conjunction with new training and organisational demands in a foreign social environment during these elective placements.
There has been no literature on the extent of PTSD among surgeons in South Africa, let alone the specific subgroup of international visiting surgeons who are training and providing essential clinical service to South African public hospitals. Our study aims to add to this literature base by identifying the prevalence of PTSD among visiting international surgeons who completed their trauma electives at a major trauma centre in South Africa.
Methods
This was a cross-sectional study utilising an online survey for all international surgeons who had completed their fixed term trauma electives during the period of 2010-2014 at the Pietermaritzburg Metropolitan Trauma Service (PMTS) in South Africa. PMTS is one of the largest academic trauma centres in the western part of the province and covers a population of over three million people. The trauma elective placement includes a mixture of ward, clinic, emergency department, acute and elective surgical experience.
We defined international surgeon as any international medical graduates (IMG) who completed their surgical training outside of South Africa. An online survey was sent to the international surgeon cohort at the end of the completion of their training at our institution. The trauma screening questionnaire (TSQ) is a 10-item self-reported screening instrument to detect a probable diagnosis of PTSD according to the DSM-IV, with a sensitivity of 0.94 and specificity of 0.56 when using a cut-off of equal to six or higher. It is based on the 24-item PTSD Symptom Scale - Self Report (PSS-SR).16 Permission to use TSQ was obtained from its author. The primary focus of the end of placement survey is on clinical experience so the TSQ was chosen for its brevity. The survey was provided in English only which all international surgeons spoke as a requirement for the elective placement. Details of local mental health services was provided for participants in the event that they screened positive. Participants could withdraw consent by not completing the survey.
Ethical approval for this study was formally endorsed by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal, Durban, South Africa (ref. no. BE427/17). Data was stored on password protected databases.
Statistical analysis
Data was captured electronically, exported to an excel spreadsheet and descriptive statistics performed using Microsoft excel, Version 16. Parametricity was assessed via the Shapiro-Wilk test. Continuous variables with normal and non-normal distributions were compared using independent samples t-test and Kruskal Wallis test, respectively, then reported using mean with standard deviation (SD) and median (range), respectively. Categorical variables were compared using chi-squared test. Statistical significance is achieved when p < 0.05.
Results
Overview
Sixty TSQ questionnaires were sent out between 2010 and 2014, of which 19 were completed and returned (32%). Two participants selectively did not answer the TSQ while answering other questions on their training and therefore were excluded from the study.
Demographics
There were 13 male and six female respondents. The mean age was 39 years (SD 6.5). The country of origin of each surgeon includes five from Japan, four from Sweden, three from Africa, three from the United Kingdom, one from Belgium, one from India, one from the Netherlands and one from New Zealand. Median postgraduate working experience was 5 (2-10) years. Of the respondents, 3 had undertaken a formal trauma rotation prior to their elective in South Africa at a level one trauma centre, as defined by the American College of Surgeons (ACS), for a median 4.5 (range 3-6) months; 12 respondents had ICU experience for a median 2 (range 1-12) months.
Median time of stay in South Africa was 6 (1-72) months. The median number of major resuscitations managed before their SA rotation was 20 (range 0-1000), and the median number managed during their placement in South Africa was 100 (4-500).
PTSD
Five (26%) respondents reported situations where there were concerns that their personal safety was at risk, of which two screened positive for probable PTSD. One respondent was robbed at gunpoint (TSQ score 1) and another reported intrusive thoughts related to a young patient's death (TSQ 3). No comments specified traumatic events related to the hospital environment.
Median TSQ score was 0.5 (0-10). Two (10.5%) respondents scored > 5. The most frequently scored for questions were - heightened awareness of potential dangers (6), irritability or outbursts of anger (4), being jumpy or startled at something unexpected (4), feeling upset by reminders of the event (3), difficulty falling or staying asleep (3), difficulty concentrating (3), upsetting dreams about the event (1), acting or feeling as though the event were happening again (1), and bodily reactions when reminded of the event (1).
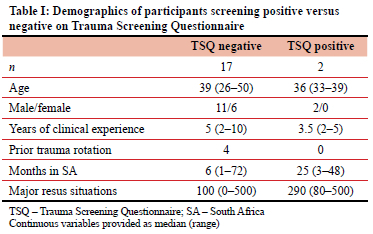
No statistical differences in age, years of prior experience, prior trauma rotation, number of major resuscitations, or length of stay in South Africa were observed in those scoring > 5 compared to < 6 in the TSQ questionnaire (Table I).
Discussion
We observed a 10.5% prevalence of probable PTSD among visiting international surgeons completing elective trauma placements in a major trauma centre in South Africa. This is lower than rates observed among general surgeons and trauma surgeons in the US and lower than local emergency service personnel. Importantly, only respondents who reported their personal safety was at risk scored for probable PTSD. No comments associated with clinical events or hospital environments were cited as stressors in this group.
Local South African populations have comparatively lower rates of PTSD (3.5%) than our study cohort despite a 73.8% lifetime prevalence of a traumatic event, suggesting a resilience to uncertain personal safety that international visitors may not be accustomed to. Orientation to local customs and culture is likely to be important for international staff.
Our survey response rate of 32% is higher than the response rate of local emergency service personnel (7-24%) and anaesthetists (24%), potentially due to the shorter 10-item questionnaire we chose for brevity. Although our rate of probable PTSD is lower, variations in screening questionnaires are acknowledged, which make comparisons difficult. For example, the 22-item Impact of Event Scale - Revised (IES-R) tool used by the latter two studies had improved specificity and sensitivity compared to the TSQ questionnaire (0.91 and 0.82, respectively).14
In our study, we observed age, workplace experience and level of trauma exposure were not significantly associated with incidence of PTSD. This is similar to some4,14 but not all studies.1,17 The relatively low rate of probable PTSD in this cohort may be related to the elective role of these surgeons as the clinical responsibility is ultimately held by a local consultant surgeon. Similarly, lower rates of PTSD were observed in US year-1 postgraduate doctors compared to senior consultant surgeons suggesting level of responsibility may be a factor of relevance.4,17 Our elective programme includes full time work that is closely supervised by attending trauma surgeons.
Among international surgeons, factors associated with higher rates of PTSD are - those operating more than 15 trauma cases per month, having more than seven call duties per month, having less than four hours of relaxation per day, those working in a poor hospital culture with less access to hospital support and those with lower salaries.4,5 Less than ten years of clinical experience was associated with PTSD in one survey; however, others found no association.1,4 Bullying has been cited as most common stressor among a cohort of postgraduate US surgical residents who screened positive for PTSD.17 Such stress-related risk factors cited among international surgeons suggest burnout may potentially be the underlying precipitant of the symptoms of PTSD rather than repeated witnessing of trauma-related physical injuries. The latter of which may be relatively benign under supervised controlled training environments and may be akin to practices utilised during exposure therapies. Burnout can be viewed as a syndrome developing in response to chronically adverse working conditions. Components of burnout include emotional exhaustion, depersonalisation, and reduced personal accomplishment.18 These symptoms may overlap with those observed in PTSD such as avoidance, negative cognitions, intrusions and hyperarousal. Kim et al. observed trauma to be associated with burnout but not PTSD in a cohort of firefighters, and that burnout mediated the relationship between trauma exposure and the development of PTSD.19 This is in keeping with our finding that two of our participants who described traumatic events scored low on the TSQ. This suggests optimising working conditions could be fundamental to reducing the rates of PTSD.
In general, half of adults with PTSD recover within three months, however it can become a chronic condition with recurrence and intensification of symptoms occurring in response to reminders of trauma.2 This is of concern to healthcare staff particularly due to the nature of work and risk of re-exposure. PTSD left untreated is believed to be associated with adverse decision making and is a potential clinical safety concern.14 Responses to prevent such adverse decision making have been limited in our local populations. For example, only 7% of local anaesthetists involved in a perioperative catastrophe received time off work despite 67% believing their ability to provide patient care was compromised in the first four hours after an event.20 Furthermore, only 15% received post-event debriefing despite 92.6% believing it would have been useful.14 Guidelines on dealing with patient death focus on medicolegal aspects and dealing with the patient's family rather than on the mental health of the staff. Debriefing, time off work, post-event mentorship and simulation-based training have been recommended as tools to support and aid resilience in staff involved in workplace trauma such as an unexpected patient death.14 Organisational factors and social support should be considered.6
The National Institute for Health and Care Excellence (NICE) guidelines for management of PTSD recommend peer support groups, involving family and carers, trauma-focused cognitive behavioural therapy (TF-CBT) and medications (specifically fluoxetine, paroxetine, sertraline or venlafaxine) for those with pharmacological preference.21 Benzodiazepines are contraindicated and have been reported to interfere with the extinction of fear conditioning.21,22 Eye movement desensitisation and reprocessing (EMDR) therapy may also be considered. 3,4-Methylenedioxy-methamphetamine (MDMA) and psychedelic drugs also show promise and are currently under investigation.23
Limitations of this study include the small sample size. It is unclear if PTSD was a pre-existing condition among the participants. Although the TSQ survey has high sensitivity, it has low specificity. The tool does not quantify other mood disorders or stress-related disorders such as burnout which may contribute to the responses. Future mental health screening should consider including wider conditions such as depression, anxiety, substance dependence, burnout and personality traits.
Conclusion
Despite exposure to high levels of witnessed physical injury, we observed low rates of probable PTSD in our cohort of international surgeons involved in trauma elective placements compared to local emergency service personnel and also surgeons working in international centres. This supplements the reputation of South Africa as an area to pursue elective trauma training. However, the literature of mental health and wellbeing among South African surgeons is sparse; further study to determine the scale of problem and potential protective factors is urgently required.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethical approval for this study was formally endorsed by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal, Durban, SA (ref. no. BE427/17).
ORCID
V Thirayan https://orcid.org/0000-0002-4528-8445
VY Kong https://orcid.org/0000-0003-2291-2572
DL Clarke https://orcid.org/0000-0002-8467-1455
REFERENCES
1. Jackson TN, Jackson DL, Nelson PR, et al. Traumatised attendings - when the doctor has the disease. Am J Surg. 2022;223(4):626-32. https://doi.org/10.1016/j.amjsurg.2021.05.010. [ Links ]
2. American Psychiatric Association, American Psychiatric Association, editors. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association; 2013. p. 947. https://doi.org/10.1176/appi.books.9780890425596. [ Links ]
3. Scheepstra KWF, Pauw HS, van Steijn ME, et al. Potential traumatic events in the workplace and depression, anxiety and posttraumatic stress: a cross-sectional study among Dutch gynaecologists, paediatricians and orthopaedic surgeons. BMJ Open. 2020;10(9):e033816. https://doi.org/10.1136/bmjopen-2019-033816. [ Links ]
4. Joseph B, Pandit V, Hadeed G, et al. Unveiling posttraumatic stress disorder in trauma surgeons - a national survey. J Trauma Acute Care Surg. 2014;77(1):148-54. https://doi.org/10.1097/TA.0000000000000271. [ Links ]
5. Jackson TN, Morgan JP, Jackson DL, et al. The crossroads of posttraumatic stress disorder and physician burnout: A national review of United States trauma and non-trauma surgeons. Am Surg. 2019;85(2):127-35. https://doi.org/10.1177/000313481908500217. [ Links ]
6. Hoell A, Kourmpeli E, Dressing H. Work-related posttraumatic stress disorder in paramedics in comparison to data from the general population of working age. A systematic review and meta-analysis. Front Public Health. 2023;11:1151248. https://doi.org/10.3389/fpubh.2023.1151248. [ Links ]
7. Cheng P, Wang L, Zhou Y, et al. Posttraumatic stress disorder and depressive symptoms among firefighters: a network analysis. Front Public Health. 2023;11:1096771. https://doi.org/10.3389/fpubh.2023.1096771. [ Links ]
8. Jitnarin N, Jahnke SA, Poston WSC, Haddock CK, Kaipust CM. Posttraumatic stress disorder (PTSD) and mental health comorbidity in firefighters. J Workplace Behav Health. 2022;37(3):147-68. https://doi.org/10.1080/15555240.2022.2081172. [ Links ]
9. Flannery RB. Psychological trauma and the trauma surgeon. Psychiatr Q [Internet]. 2020 Nov 21 [cited 2021 Oct 13]; Available from: http://link.springer.com/10.1007/s11126-020-09862-y. [ Links ]
10. Prinsloo M, Machisa M, Kassanjee R, et al. Estimating the changing burden of disease attributable to interpersonal violence in South Africa for 2000, 2006 and 2012. S Afr Med J. 2022;693-704. https://doi.org/10.7196/SAMJ.2022.v112i8b.16512. [ Links ]
11. Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;85(09):695-702. https://doi.org/10.2471/BLT.06.037184. [ Links ]
12. Atwoli L, Stein DJ, Williams DR, et al. Trauma and posttraumatic stress disorder in South Africa: analysis from the South African Stress and Health Study. BMC Psychiatry. 2013;13(1):182. https://doi.org/10.1186/1471-244X-13-182. [ Links ]
13. Ward CL, Lombard CJ, Gwebushe N. Critical incident exposure in South African emergency services personnel: prevalence and associated mental health issues. Emerg Med J. 2006;23(3):226-31. https://doi.org/10.1136/emj.2005.025908. [ Links ]
14. Van Niekerk JJS, Lemmer-Malherbe J, Nel M. PTSD in South African anaesthetists after experiencing a death on the theatre table. Southern Afr J Anaesth Analg. 2020;26(6):280-6. https://doi.org/10.36303/SAJAA.2020.26.6.2386. [ Links ]
15. Uchino H, Kong VY, Plani F, et al. Trauma electives in South Africa provide valuable training for international surgeons. S Afr Med J. 2019;109(3):182. https://doi.org/10.7196/SAMJ.2019.v109i3.13551. [ Links ]
16. Dekkers AMM, Olff M, Naring GWB. Identifying persons at risk for PTSD after trauma with TSQ in The Netherlands. Community Ment Health J. 2010;46(1):20-5. https://doi.org/10.1007/s10597-009-9195-6. [ Links ]
17. Jackson T, Provencio A, Bentley-Kumar K, et al. PTSD and surgical residents: Everybody hurts... sometimes. Am J Surg. 2017;7. https://doi.org/10.1016/j.amjsurg.2017.08.037. [ Links ]
18. Schonfeld IS, Bianchi R, Palazzi S. What is the difference between depression and burnout? An ongoing debate. Riv Psichiatr. 2018;53(4):218-19. [ Links ]
19. Kim W, Bae M, Chang SJ, et al. Effect of burnout on posttraumatic stress disorder symptoms among firefighters in Korea: Data from the Firefighter Research on Enhancement of Safety & Health (FRESH). J Prev Med Public Health. 2019;52(6):345-54. https://doi.org/10.3961/jpmph.19.116. [ Links ]
20. Gazoni FM, Amato PE, Malik ZM, Durieux ME. The impact of perioperative catastrophes on anaesthesiologists - results of a national survey. Anesth Analg. 2012;114(3):596-603. https://doi.org/10.1213/ANE.0b013e318227524e. [ Links ]
21. NICE guideline. Posttraumatic stress disorder [Internet]. 2018 [cited 2021 Oct 10]. Available from: www.nice.org.uk/guidance/ng116. [ Links ]
22. Ehret M. Treatment of posttraumatic stress disorder: Focus on pharmacotherapy. Ment Health Clin. 2019;9(6):373-82. https://doi.org/10.9740/mhc.2019.11.373. [ Links ]
23. Taylor D, Barnes T, Young A. The Maudsley Prescribing Guidelines in Psychiatry, 14th Edition. 14th ed. Wiley-Blackwell; 2021. https://doi.org/10.1002/9781119870203. [ Links ]
 Correspondence:
Correspondence:
V Thirayan
Email: varunthirayan@gmail.com














