Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.62 n.1 Cape Town 2024
http://dx.doi.org/10.36303/SAJS.00194
SURVEY
The academic progress of female general surgery and orthopaedic surgery trainees in South Africa
S GovenderI; R NaidooI; S EbrahimI, II; B SinghI
IDepartment of Surgery, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
IIHealth Systems Research Unit, South African Medical Research Council, South Africa
ABSTRACT
BACKGROUND: Globally, medical institutes have seen an increase in female graduates, however surgical disciplines remain male-dominated. An epidemiological shift towards non-communicable diseases and trauma may result in a shortage of surgical specialists. One strategy to improve the surgical workforce is the recruitment of female graduates
METHODS: A non-validated questionnaire was administered to females registered for the Master of Medicine (MMED) degree in General and Orthopaedic Surgery at the University of KwaZulu-Natal (UKZN) between 2000 and 2015. The study evaluated reasons for choice of surgery as a career, challenges faced on the domestic and work front, as well as factors that assisted with successful completion of training
RESULTS: Seventy-two female trainees in General Surgery and Orthopaedics were identified from the UKZN databases. The contact details for 62 of these trainees were available. The overall response rate was 71.0% (44/62). A total of 95.5% (42/44) of participants selected surgery due to a passion for the field. Major challenges identified were a poor home and work-life balance (72.1%, 31/43) and poor working conditions (62.8%, 27/43). Female trainees perceived that they were viewed as inferior by patients (65.9%, 29/44). Successful trainees had a good home support system (89.3%, 25/28) and mentorship during training (60.7%, 17/28), and 85.7% (24/28) did not regret their career choice
CONCLUSION: The recruitment and retention of females in surgery will contribute to maintaining an adequate surgical workforce. Training programmes need to improve work-life balance without compromising on producing competent surgeons. Improved visibility of female surgeons in leadership roles should be encouraged to promote mentorship and recruitment of trainees
Keywords: female general surgeons, female orthopaedic surgeons, academic progression of women in surgery
Introduction
Approximately five billion people lack access to safe and affordable surgical care globally.1 Many countries, including South Africa need to increase the number of specialist surgeons to reach the recommended 20 per 100 000 population.1 According to the Lancet Commission on Global Surgery 2030, the global health community has ignored building surgical capacity because surgery has been viewed as complex and resource intensive, pushing public health initiatives to favour vaccines and the treatment of infectious diseases.1 In a time of changing epidemiological trends, which show an increase in non-communicable disease and trauma, a severe shortage of surgeons is anticipated globally.24
It is well recognised that one way to build an adequate surgical workforce would be to expand the number of women in surgery.1 There has been a paradigm shift over the years in the gender of medical students such that we have reached a point where the graduating classes have equal male and female graduates or more females.58 This poses a unique problem to surgical departments who now need to attract, train and retain women surgeons.1 Traditionally, surgery has been seen as a career where it is difficult to balance home and work-life by both males and females.4
This balance seems even more difficult for women; given the increase in female medical students, this threatens the surgical disciplines even further.4
Most studies on this topic come from high-income countries (HICs).1 A recent scoping review looking at females in surgery globally showed that 89% of the articles reviewed were from HICs and only 4% studied populations in low- to middle-income countries (LMICs).1 Female surgeons from different countries have different perceptions of their career barriers.1 To our knowledge only one such study was published locally.9 This study interviewed trainees across many different surgical subspecialties.9 General surgery and orthopaedic surgery are two relatively large surgical disciplines that seem to lag behind in terms of gender transformation.10
The South African government has progressive gender equality employment policies. Males and females earn equal pay and mothers have a four-month paid maternity leave policy. The leave policy also allows for family responsibilities. This liberal mindset, however, needs to translate to the working environment. We aimed to survey women who were successful in completing the general surgery and orthopaedic surgery training programmes, as well as those who left the programme, to gain some perspective on their experiences and improve our programme or to dispel some myths that may perpetuate a negative perception of surgery.
Methods
Study design and setting
This was an observational cross-sectional survey conducted at the University of KwaZulu-Natal (UKZN), Durban, South Africa. The participants approached were registered at the UKZN for a specialisation in general surgery or orthopaedic surgery.
Participants
The women surveyed were registered for a Master of Medicine (MMED) degree in Surgery or Orthopaedics at the UKZN between the year 2000 and 2015. The participants were approached telephonically or via e-mail to participate in the survey. Only participants who provided written informed consent completed the survey.
Survey procedure
A survey was conducted during 2018 and 2021. A non-validated questionnaire was compiled after conducting a literature review and incorporating common themes from the existing literature. It comprised 55 items, including dichotomous, multiple-choice and open-ended questions. The survey instrument collected information on participant demographics and current employment, factors that influenced their choice of speciality, their experience during surgical training as well as their experience post qualification. It also looked at factors that influenced their successes as well as challenges that were experienced during training. It collected information on factors that influenced trainees to exit the programme prematurely and sought to find out if females regretted their career choice. The survey was anonymised. Participants who agreed to participate in this research were given the paper-based survey or an electronic survey and afforded up to one-month to complete it. Data from the returned surveys was transferred to a Microsoft Excel spreadsheet for the statistical analysis.
Statistical analysis
Quantitative data was captured onto a Microsoft Excel Spreadsheet and thereafter analysed using R Statistical Computing software, version 3.6.3 of the R Core Team. The data was categorical in nature and the descriptive statistics were presented in the form of counts and percentage frequencies. Some of the results were visually displayed in the form of pie charts. Thematic analysis was used to obtain the main points from the open-ended question responses.
Results
Seventy-two female trainees in general surgery and orthopaedics who commenced their training between 2000 and 2015 were identified from the UKZN databases. The contact details for 62 of these trainees were available. Of these, only 44 completed the survey and comprised the study cohort. The overall response rate was thus 71.0% (44/62). Of the 44 participants surveyed, 37 were general surgery trainees and seven were orthopaedic surgery trainees. A total of 37 participants completed their registrar training and seven participants exited the programme prior to completion of training. Of the 37 who completed their training time, 28 met all the requirements to register with the Health Professions Council of South Africa (HPCSA) in their chosen specialty, while nine were still in the process of doing so.
Over this period, the UKZN produced 172 qualified general surgeons: of these, 24 (14.0%) were female. Between 2000-2007, 2/24 females qualified, whilst subsequent to this in the years 2008 and 2015, 22 female surgeons qualified at the UKZN.
Twenty-six (59%) participants were between the ages of 30-39 years. Nineteen participants were single, and of those 68.4% (13/19) did not attribute this to their profession. Eighteen (40.9%) participants had children and 26 (59.1%) did not. Of the latter group, 73.1% (19/26) attributed not having children to the demands of their job. Table I summarises the demographic characteristics of all participants.
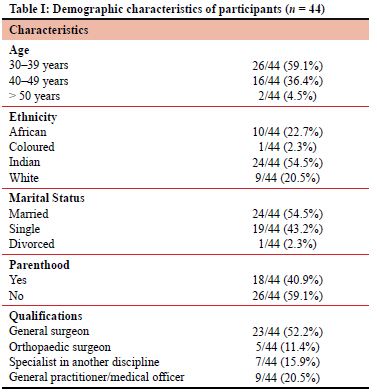
Table II describes the comments from participants on the registrar training programme. A total of 95.5% (42/44) of participants chose surgery as a career based on their passion for the field; 22.7% (10/44) were inspired by a role model to choose a career in surgery. The main challenges related to a poor home and work-life balance as reported by 72.1% (31/43) of the trainees. Regarding the number of working hours, 56.8% (25/44) felt that these were excessive compared to other disciplines, 31.8% (14/44) felt that the long hours were necessary for training in a surgical discipline and 11.4% (5/44) felt that the number of hours were the same as in other disciplines. One participant reported having to work shifts that often exceeded 30 hours. Two participants noted that the long working hours often left little time for academic reading.
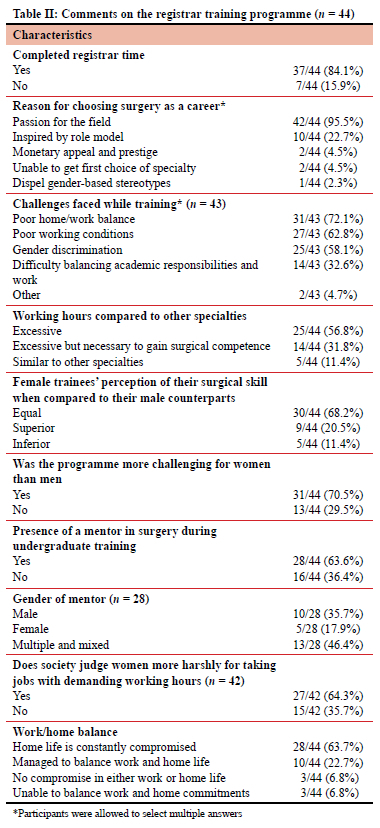
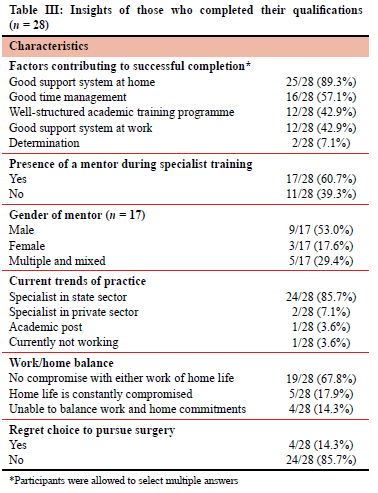
With respect to work-life balance, 63.6% (28/44) reported that their home life was constantly compromised, while 22.7% (10/44) were able to balance work and home life most of the time. Participants reported that they prioritised work over home during training, with one surgeon who commented that the training programme "was not designed to provide a work-life balance at all". One participant reported delaying starting a family until after training was completed. An improved work-life balance was reported once training was completed, with 67.9% (19/28) of participants reporting no compromise with either work or home life (Table III).
Participants perceived patients, senior medical staff and allied staff regarding female trainees as inferior when compared to male trainees - 65.9% (29/44), 61.4% (27/44) and 59.1% (26/44) respectively as shown in Figure 1.
However, 68.2% (30/44) of female surgeons perceived their own skills/abilities to be equal compared to male trainees, 20.5% (9/44) thought they had superior surgical skills and 11.4% (5/44) thought their surgical skills were inferior compared to men (Table II). One participant noted that a female surgeon always had to prove herself more. The majority of participants, 64.3% (27/42) compared to 35.7% (15/42), felt that society judges female surgeons more harshly for working long hours as compared to their male counterparts (Table II).
Table III describes insights from those who completed their training and had qualified. Successful completion of the training programme was attributed to a good support system at home, as reported by 89.3% (25/28) of female surgeons; 60.7% (17/28) of those who successfully completed the programme reported having a mentor during their postgraduate years. Most of these qualified surgeons (82.1%, 23/28) were interested or are currently involved in academic leadership roles or undergraduate teaching and had an interest in pursuing research on a part-time basis.
Those who successfully completed the general surgery fellowship were asked for suggestions to make the speciality more appealing to undergraduate students and junior doctors. Four main themes emerged and are listed in Table IV. Participants were also asked to share their thoughts on their journey through the registrar programme. The hindsight perspective of those who had completed training may be helpful to prospective candidates and encourage others to join. Two main themes emerged and are reported in Table IV.
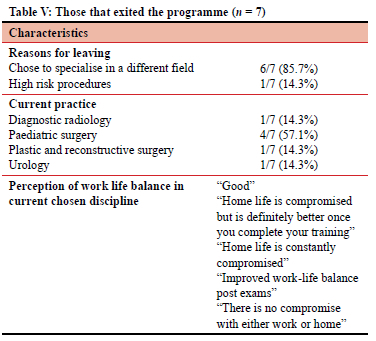
Seven participants prematurely exited the surgical training programme (Table V). The main reason for leaving was the desire to specialise in a different field. These participants were satisfied with their current jobs and placements. Nine participants had completed their training time but had outstanding academic components, such as the MMED and final fellowship examinations. It was reassuring to note that all participants planned to complete their degrees. Most of these participants (88.9%, 8/9) were currently employed as medical officers in the state sector. There were a range of factors that were reported as barriers to degree completion, such as poor time management, unsuccessful attempts at passing the final fellowship exam, falling pregnant whilst training and the COVID-19 pandemic.
Discussion
This study showed that the majority of the females who joined surgery did so because they were passionate about the field. The participants themselves suggested that more exposure to surgical procedures as young doctors or medical students may stimulate a passion for surgery. A further suggestion was a more formal or structured teaching programme during internship or a formalised mentoring holiday programme during undergraduate training.11-13
According to international studies, the presence of mentors in undergraduate training or during internship promotes the matriculation of females into surgical disciplines.8,12,14 Our study showed that only 22.7% of trainees were inspired by a role model to pursue a career in surgery. It is suggested that female students are more inspired by female role models; perhaps seeing a female general or orthopaedic surgeon at work makes the idea more plausible.1,13 We anticipate that as the number of female surgeons increases locally, this will inspire the younger generation of female medical students to pursue a career in general or orthopaedic surgery.
To improve the programme and make it more trainee friendly the participants identified the challenges they faced during their training. As in most studies on surgical training, poor work-life balance was the biggest challenge.4,14-17 The nature of surgical training, as well as the difficult and at times unpredictable working hours, was not attractive to either males or females but more so to the latter.13,14,18 Surgery, by nature, is physically and mentally demanding. The number of acute emergencies a surgeon has to deal with likely outweighs most other specialties. A number of our participants, however, recognised that the hours were long but necessary during their training time. We found it interesting that most participants who completed the programme, reported that there was no compromise between home and work as practising consultant surgeons. This is the narrative that female students need to be aware of and that will help in dispelling the myth that being a general or orthopaedic surgeon always means compromising your home life. One of the participants reported delaying having a child until after she had completed her training so as not to feel torn between home and work; she felt this strategy was successful for her.
Gender discrimination, in its many forms, was a challenge reported by 58.1% of the participants. Female surgeons felt that senior personnel, allied medical personnel as well as patients perceived them to be inferior to their male colleagues. None of the participants reported sexual harassment as a factor and this is in contrast to other similar studies.1,10,17 Internationally, discrimination based on race, gender or even religion has been a problem in the workplace and medicine is no exception. In 2016, the Royal Australian College of Surgeons introduced measures to reduce this behaviour, such as a mandatory course to be taken by all its members as well as launching anonymous complaints' lines and offering free counselling services when needed. They also collaborated with major hospital groups and health agencies, committing to resolve the grievances of junior doctors.19 Locally, there is a culture shift towards recognising the difficulties experienced in the workplace, but perhaps a formal briefing on appropriate workplace behaviour should be instituted by the Health Professionals Council of South Africa. We could also adapt this international course and introduce it at a university level to both undergraduates and postgraduates.
An international study suggested that women may have low self-esteem due to the perception that their colleagues and patients view them as inferior.20 Participants reported being mistaken for a nurse on numerous occasions and patients assuming that a junior male doctor is the surgeon. Many suggestions to tackle this issue have been proposed; one being the drive to change peoples' perceptions of what a surgeon should look like, with campaigns such as #IlookLikeASurgeon; changing the cover pictures of surgical journals or websites; and advertisements and television characters to reflect more women in the field.21,22 Literature supporting the competency of female surgeons has also recently been published in eminent journals.23,24 Although these campaigns are well underway in the western world, in South Africa and other African countries similar awareness campaigns are needed.
The main factor that contributed to successful completion of the surgical training programme at the UKZN was a good home support system followed by a good support system at work. Other factors cited were good time management and a structured training programme. Our study findings were also consistent with other international studies regarding delaying of childbearing until after completion of surgical training.8 One participant advised to "complete training and then start a family, that way you give your all to work without feeling guilty for sacrificing family."
The majority of participants who successfully completed the programme (61%) reported having a mentor during their postgraduate years. Most of the participants in our study reported having male mentors. This is likely due to the disparate male to female surgeon ratio in the general surgery and orthopaedic surgery departments. It is also worth mentioning that 39.3% of trainees did not find a suitable mentor. The current literature seems to favour female mentors for female trainees, which may explain the lack of mentors in a large number of our participants. One may argue that a mentorship develops organically between a teacher and trainee, however, current trends point to structured mentorship programmes to ensure that all trainees are at least allocated a mentor.12
Most female surgeons who qualified, were employed in the state sector. While this is favourable for the state hospitals, this trend of practice may represent an underlying gender bias. Female surgeons in private practice face unique challenges such as a difficult home and work-life balance and not being able to sustain an income as private patients have the choice of surgeon and may instinctively choose a male surgeon. One participant commented: "as a woman, a private practice in general surgery is very demanding and that leaves only state practice."
The department of surgery at the UKZN needs to find ways to improve the female intake into the surgical registrar training programme. Suggestions by the respondents to improve the programme related to an improvement in working hours and conditions. These are systemic problems that affect all surgical trainees. Improvement in resources and staffing will naturally improve these areas. Most participants suggested an improvement in support systems for staff, however they did not specify what these should be. Mental health support to avoid "burnout", channels to report discrimination and bullying and protected academic time are possible strategies to improve the work environment.
Seven participants who exited the general surgery programme completed the survey. Most left the programme to join parallel surgical specialties that they had always been interested in or had developed an interest in while rotating through those specialties during their general surgery training time. They were generally satisfied with their time in general surgery. However, one of the participants had the following comment: "After 22 months of training, I could not see myself in the role of a general surgeon due too long hours, laborious work requirements and high-risk procedures (human immunodeficiency virus [HIV] risk) in the long term, and I wanted a different career path that stimulated my mind more."
It is encouraging to note that most female surgical trainees who qualified did not regret their decision and none of those still completing their specialty training regretted their choice. This finding was consistent with the literature.9
There are limitations to this study; the study population is relatively small due to the limited number of female general and orthopaedic surgeons in the country. It is a single-centre study and findings may not be generalisable.
Conclusion
Over the past two decades, the number of female general and orthopaedic surgery specialists trained at the UKZN has increased, however the number is still not ideal. A passion for the field of surgery was the dominant reason for selecting surgery as a career. Significant challenges in the path to specialisation were a poor home and work-life balance and poor working conditions. Surgical training programmes need to employ strategies that improve work and home balance without compromising surgeon competence.
An improved visibility of female surgeons in leadership roles should be encouraged to promote recruitment of trainees, and this will also help in breaking down the male surgeon stereotype. Training programmes should also improve support systems for trainees at work and prioritise mentorship. This strategy will go a long way to attracting and retaining female surgeons in South Africa and other developing countries.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
This research was approved by the Biomedical Research Ethics Committee at the University of KwaZulu-Natal, South Africa (Protocol BREC 430/18).
ORCID
S Govender https://orcid.org/0000-0003-4589-0513
R Naidoo https://orcid.org/0000-0002-1992-5615
S Ebrahim https://orcid.org/0000-0001-9822-6347
B Singh https://orcid.org/0000-0003-0799-256X
REFERENCES
1. Xepoleas MD, Munabi NCO, Auslander A, Magee WP, Yao CA. The experiences of female surgeons around the world: a scoping review. Hum Resour Health. 2020;18(1):80. https://doi.org/10.1186/s12960-020-00526-3. [ Links ]
2. Oslock WM, Satiani B, Way DP, et al. A contemporary reassessment of the US surgical workforce through 2050 predicts continued shortages and increased productivity demands. Am J Surg. 2022;223(1):28-35. https://doi.org/10.1016/j.amjsurg.2021.07.033. [ Links ]
3. Dell AJ, Kahn D. Where are general surgeons located in South Africa? S Afr J Surg. 2018;56(1):12-20. https://doi.org/10.17159/2078-5151/2018/v56n1a2393. [ Links ]
4. Kwong A, Chau WWW, Kawase K. Work-life balance of female versus male surgeons in Hong Kong based on findings of a questionnaire designed by a Japanese surgeon. Surg Today. 2014;44(1):62-72. https://doi.org/10.1007/s00595-013-0583-8. [ Links ]
5. The Lancet. Bringing women to the forefront of science and medicine. Lancet. 2012;379(9819). https://doi.org/10.1016/S0140-6736(12)60286-4. [ Links ]
6. Seemann NM, Webster F, Holden H, et al. Women in academic surgery: why is the playing field still not level? Am J Surg. 2016;211(2):343-9. https://doi.org/10.1016/j.amjsurg.2015.08.036. [ Links ]
7. Bernardi K, Lyons NB, Huang L, et al. Gender disparity among surgical peer-reviewed literature. J Surg Res. 2020;248:117-22. https://doi.org/10.1016/jjss.2019.11.007. [ Links ]
8. Anderson KT, Hyman S, Henry MCW. Demographics in general surgery programs: relationship between female faculty and proportion of female residents. Am J Surg. 2020;220(5):118993. https://doi.org/10.1016/j.amjsurg.2020.06.044. [ Links ]
9. Umoetok F, Van Wyk J, Madiba TE. Does gender impact on female doctors' experiences in the training and practice of surgery? A single centre study. S Afr J Surg. 2017;55:8-12. [ Links ]
10. Greenup RA, Pitt SC. Women in academic surgery: a double-edged scalpel. Acad Med. 2020;95(10):1483-4. https://doi.org/10.1097/ACM.0000000000003592. [ Links ]
11. Naidu P, Buccimazza I. Surgery in South Africa: challenges and barriers. S Afr J Surg. 2021;59(3). https://doi.org/10.17159/2078-5151/2021/v59n3a3391. [ Links ]
12. Naidu P, Buccimazza I. Surgery in South Africa: the attitudes toward mentorship in facilitating general surgical training. S Afr J Surg. 2021;59(3):82-5. https://doi.org/10.17159/2078-5151/2021/v59n3a3597. [ Links ]
13. Singh C, Loseth C, Shoqirat N. Women in surgery: a systematic review of 25 years. BMJ Leader. 2021;5(4):283-90. https://doi.org/10.1136/leader-2019-000199. [ Links ]
14. Trinh LN, O'Rorke E, Mulcahey MK. Factors influencing female medical students' decision to pursue surgical specialties: a systematic review. J Surg Educ. 2021;78(3):836-49. https://doi.org/10.1016/jjsurg.2020.08.050. [ Links ]
15. Rasmussen JM, Najarian MM, Ties JS, et al. Career satisfaction, gender bias, and work-life balance: a contemporary assessment of general surgeons. J Surg Educ. 2021;78(1):119-25. https://doi.org/10.1016/jjsurg.2020.06.012. [ Links ]
16. Roodt L. Female general surgeons - current status, perceptions and challenges in South Africa. A pilot study at a single academic complex. Master's thesis, University of Cape Town. 2016 [cited 2022 Nov 01]. p. 1-100. Available from: https://open.uct.ac.za/handle/11427/2366. [ Links ]
17. Hutchison K. Four types of gender bias affecting women surgeons and their cumulative impact. J Med Ethics. 2020;46(4):236-41. https://doi.org/10.1136/medethics-2019-105552. [ Links ]
18. Edge J. Editorial: Look like a surgeon. S Afr J Surg. 2017;55(3):5-6. [ Links ]
19. Coopes A. Operate with respect: how Australia is confronting sexual harassment of trainees. BMJ. 2016;354:i4210. https://doi.org/10.1136/bmj.i4210. [ Links ]
20. Cochran A, Hauschild T, Elder WB, et a;. Perceived gender-based barriers to careers in academic surgery. Am J Surg. 2013;206(2):263-8. https://doi.org/10.1016/j.amjsurg.2012.07.044. [ Links ]
21. Wall SL, Troisi K. Impact of gender bias on women surgeons: a South African perspective. J Med Ethics. 2020;46(11):785-6. https://doi.org/10.1136/medethics-2020-106442. [ Links ]
22. Rayne S. "I see you": gender representation and unconscious bias in images of surgeons. S Afr J Surg. 2017;55(3):62-3. [ Links ]
23. Wallis CJ, Ravi B, Coburn N, et al. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:j4366. https://doi.org/10.1136/bmj.j4366. [ Links ]
24. Sharoky CE, Sellers MM, Keele LJ, et al. Does surgeon sex matter? Practice patterns and outcomes of female and male surgeons. Ann Surg. 2018;267(6):1069-76. https://doi.org/10.1097/SLA.0000000000002460. [ Links ]
 Correspondence:
Correspondence:
R Naidoo
Email: ruvashni@gmail.com














