Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.4 Cape Town 2023
http://dx.doi.org/10.36303/sajs.4069
CASE REPORT
Transverse colon volvulus - a case report and literature review
L NikschI; M LockwoodII; PL van RooyenIII; NA NikschII; L LorentzII
IZuid-Afrikaans Hospital Accident and Emergency Unit, South Africa
IICapital Radiology, Life Groenkloof Hospital, South Africa
IIILife Groenkloof Hospital, South Africa
SUMMARY
Transverse colon volvulus is a rare diagnosis, with less than 100 cases reported up to 2019. The condition is complicated by the absence of characteristic radiological findings and is typically diagnosed intraoperatively. It is a surgical emergency as the condition can lead to bowel necrosis and is associated with a mortality rate of up to 33%. Bowel resection is the treatment of choice, and if a megacolon is present a subtotal colectomy is recommended. Due to the rarity of transverse colon volvulus, limited data is available on the long-term outcome of patients.
Keywords: transverse colon volvulus
Case report
A 46-year-old male presented with bloating and watery stools for several weeks. Prior to presentation, he was admitted to a different facility, where a colonoscopy was performed after which he was discharged. A colonic resection had been performed two years previously for sigmoid volvulus.
Clinical examination demonstrated a right sided distended abdomen and tympanic bowel sounds. C-reactive protein (CRP) was elevated at 187 mg/l.
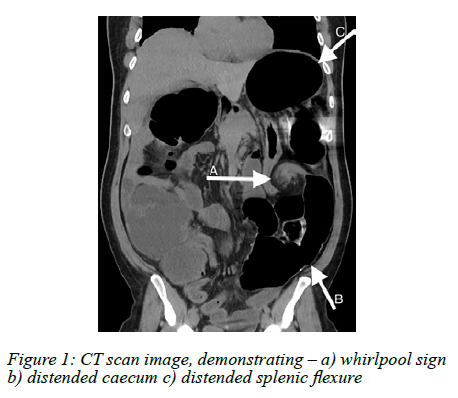
An abdominal radiograph demonstrated markedly distended large and distal small bowel loops with an associated 'coffee bean' sign, indicating large bowel obstruction. An abdominal computed tomography (CT) scan showed a classic 'whirlpool sign' of the mesentery in the left flank with a severely distended colon - caecum, through to splenic flexure (Figure 1). Distal colonic volvulus was considered.
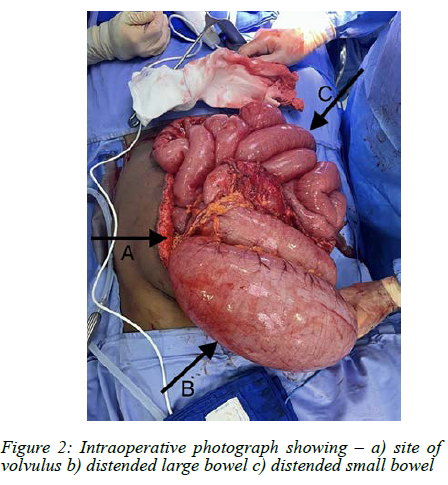
Intraoperatively a transverse colon volvulus was found with a suspicion of visceral myopathy. A subtotal colectomy was performed, with resection of the ascending, transverse and proximal descending colon (Figure 2). The postoperative course was uncomplicated.
Histopathological evaluation indicated degeneration of the smooth muscle, with replacement fibrosis in the distal part of the colon and overlying atrophic mucosa. The histopathological findings were non-specific and differentiation between primary and secondary myopathy was not possible.
Discussion
Volvulus is described as the twisting of a loop of intestine along the mesenteric axis that supplies it, leading to venous obstruction and subsequent arterial compromise.14 A common cause of large bowel obstruction is colonic volvulus, representing the leading cause of colonic obstruction in sub-Saharan Africa with a prevalence of up to 69%.15 Sigmoid volvulus remains common in the geographic region known as the 'Volvulus Belt', which includes the following regions: Africa, South America, Russia, the Middle East and Eastern Europe.5
The short mesentery of the transverse colon with fixed hepatic and splenic flexures inhibits mobility, making transverse colon volvulus uncommon. Transverse colon volvulus accounts for only around 5% of all causes of bowel obstruction; 60-80% of cases are related to the sigmoid colon and 20-40% to the caecum.26 Transverse colon volvulus was first described by Kallio, a Finnish surgeon, in 1932.23 Up to 2019, less than 100 patients were reported with this diagnosis.2 An even rarer medical diagnosis is that of a metachronous colonic volvulus.6 Colonic volvulus of the transverse colon and sigmoid colon can be either metachronous or synchronous.56
The aetiology of transverse colon volvulus can be grouped into congenital, physiological or mechanical causes.47 Mechanical causes include previous volvulus of the transverse or sigmoid colon, distal colonic obstruction, adhesions, mobility of right colon, malposition of colon following previous surgery, inflammatory strictures and carcinoma.4,7 Physiological causes include high-fibre diet and large bowel distention secondary to chronic constipation.7 Chronic constipation can promote elongation and chronic redundancy of the transverse colon.24 Other factors reported include Chilaiditi's syndrome (Chilaiditi sign is a radiographic finding of a segmental interposition of a loop of large or small bowel between the liver and diaphragm; when this is accompanied by gastrointestinal symptoms, it is known as Chilaiditi syndrome),8 clostridium difficile pseudomembranous colitis, and impaired intestinal motility associated with pregnancy.7
Visceral myopathies are defined by the presence of smooth muscle dysfunction.9 Hollow visceral myopathy is a pathological condition involving the smooth muscles of the gastrointestinal tract - the affected smooth muscles undergo progressive degeneration and fibrous replacement resulting in the loss of gastrointestinal motility.10 Several hereditary and systemic disorders are associated with gastrointestinal smooth muscle abnormalities and constipation; therefore, there is an existing association of abnormalities in smooth muscle function and constipation.11
The two congenital properties thought to cause volvulus are redundancy and non-fixation.7 The transverse colon, sigmoid colon and caecum are mobile structures within the peritoneum tethered by their mesentery, but the ascending and descending segments of the colon are fixed structures.3,4 The mobility of some of the colonic structures allows the occurrence of volvulus at these locations.3,4 Redundancy of any of these segments further enables the formation of a volvulus.3,4
Eisenstat et al. first categorised transverse colon volvulus as being either acute fulminating or subacute progressive.3 Acute fulminating transverse colon volvulus is associated with an acute onset of severe abdominal pain, rebound tenderness and vomiting but yet minimal abdominal distention.13,7 Bowel sounds are initially hyperactive, but may become absent later on.1,2,7 The clinical condition of the patient deteriorates rapidly.1,2
In our case, the patient presented with subacute progressive transverse colon volvulus. A progressive onset of symptoms can delay the diagnosis and treatment, potentially resulting in the progression of the disease to the acute fulminating type with bowel infarctions, peritonitis and death.2,7 The subacute type is associated with severe abdominal distention, mild abdominal pain without rebound tenderness, and little or no nausea and vomiting.2,3,7
A transverse colon volvulus does not have the same classical radiographic features as caecal and sigmoid volvuluses.2-4,7 Plain abdominal radiographs show nonspecific colonic dilatation and are frequently misinterpreted as signs of a sigmoid colon volvulus, as in this case.1 Abdominal CT is advised for early diagnosis.2,7
The diagnosis of a transverse colon volvulus before surgery is rarely observed and is usually only confirmed intraoperatively.1,2,7
Unlike in sigmoid and caecal volvulus, an attempt at endoscopic decompression and drainage of the colon is not recommended, mainly due to the high probability of necrosis. Thus, the volvulus must be surgically detorted.2,4,7 Surgical options include detorsion, detorsion with colopexy, resection with primary anastomosis, or resection with colostomy or ileostomy and mucous fistula.4 Both detorsion and detorsion with colopexy have a higher rate of recurrence than resection.2,4,7 Resection, with or without primary anastomosis, constitutes the treatment of choice to prevent recurrence.1,2,4,6,7 The incidence of recurrent volvulus after previous resection and primary anastomosis varies between 22-36%.2,7 Therefore, some authors recommend the consideration of a subtotal colectomy in the presence of a megacolon, instead of a partial resection of the involved bowel segment.2,7 Limited data is available on the long term post-surgical outcome due to the rarity of the disease.1
The mortality rate of transverse colon volvulus is 33%, which is higher than the mortality rate of sigmoid colon volvulus (21%) and caecal volvulus (10%).1,2 This is likely due to the delay in making the correct diagnosis.
The diagnosis of transverse colon volvulus remains challenging. Abdominal CT is able to indicate colonic obstruction and volvulus; however, the level of colonic obstruction may only be established intraoperatively, as in this case. The patient's history of a previous sigmoid volvulus was a clear predisposing factor for the development of a transverse colon volvulus. Early diagnosis, a high level of suspicion and early surgical intervention is critical for positive patient outcomes.
Acknowledgements
Dr JS du Plessis for the histopathology report.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
This article does not contain any studies with human or animal subjects.
ORCID
L Niksch https://orcid.org/0000-0002-9637-9216
M Lockwood https://orcid.org/0009-0004-3883-7014
PL van Rooyen https://orcid.org/0009-0004-7493-3580
NA Niksch https://orcid.org/0009-0003-7633-009X
L Lorentz https://orcid.org/0000-0001-6033-1678
REFERENCES
1. Deshmukh SN, Maske AN, Deshpande AP, Shende SP. Transverse colon volvulus with Chilaiditis syndrome. Indian J Surg. 2010;72(4):347-9. https://doi.org/10.1007/s12262-010-0130-4. [ Links ]
2. Hasnaoui H, Laytimi F, Elfellah Y, et al. Transverse colon volvulus presenting as bowel obstruction: a case report. J Med Case Rep. 2019;13(1):156. https://doi.org/10.1186/s13256-019-2080-1. [ Links ]
3. Sparks DA, Dawood MY, Chase DM, Thomas DJ. Ischemic volvulus of the transverse colon: A case report and review of literature. Cases J. 2008;1(1):174. https://doi.org/10.1186/1757-1626-1-174. [ Links ]
4. Rahbour G, Ayantunde A, Ullah MR, Arshad S, Kerwat R. Transverse colon volvulus in a 15-year-old boy and the review of the literature. World J Emerg Surg. 2010;5(1):19. https://doi.org/10.1186/1749-7922-5-19. [ Links ]
5. Ndong A, Diao ML, Tendeng JN, et al. Synchronous sigmoid and transverse volvulus: A case report and qualitative systematic review. Int J Surg Case Rep. 2020;75:297-301. https://doi.org/10.1016/j.ijscr.2020.09.027. [ Links ]
6. Chinisaz F, Asefi H, Miratashi Yazdi SA. Volvulus of the transverse colon after resection of the sigmoid volvulus: A case report. J Taibah Univ Med Sci. 2022;17(4):626-9. https://doi.org/10.1016/j.jtumed.2021.08.011. [ Links ]
7. Sana L, Ali G, Kallel H, et al. Spontaneous transverse colon volvulus. Pan Afr Med J. 2013;14:160. https://doi.org/10.11604/pamj.2013.14.160.2073. [ Links ]
8. Nair N, Takieddine Z, Tariq H. Colonic interposition between the liver and diaphragm: "The Chilaiditi Sign". Can J Gastroenterol Hepatol. 2016;2016:2174704. https://doi.org/10.1155/2016/2174704. [ Links ]
9. Hashmi SK, Ceron RH, Heuckeroth RO. Visceral myopathy: clinical syndromes, genetics, pathophysiology, and fall of the cytoskeleton. Am J Physiol Gastrointest Liver Physiol. 2021;320(6):G919-G935. https://doi.org/10.1152/ajpgi.00066.2021. [ Links ]
10. Dahiya DS, Batth A, Batth J, et al. Hollow visceral myopathy, a rare gastrointestinal disorder: a case report and short review. J Investig Med High Impact Case Rep. 2021;9:23247096211034303. https://doi.org/10.1177/23247096211034303. [ Links ]
11. Knowles CH, Farrugia G. Gastrointestinal neuromuscular pathology in chronic constipation. Best Pract Res Clin Gastroenterol. 2011;25(1):43-57. https://doi.org/10.1016/j.bpg.2010.12.001. [ Links ]
 Correspondence:
Correspondence:
email: lizbeniksch@gmail.com














