Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.4 Cape Town 2023
http://dx.doi.org/10.36303/sajs.4060
PAEDIATRIC SURGERY
The impact of the COVID-19 pandemic on presentation of surgical disease in paediatric patients at a tertiary centre in Cape Town, South Africa
C Kohier; B Banieghbal
Department of Paediatric Surgery, Tygerberg Hospital, South Africa
ABSTRACT
BACKGROUND: Children are less susceptible to infection with SARS-CoV-2 and subsequent severe disease, yet especially vulnerable to the indirect effects of the pandemic. A constrained healthcare service, combined with the societal and behavioural changes observed during the pandemic, is likely to have altered the presentation of paediatric surgical disease. The objective was to investigate the impact of the COVID-19 pandemic on the volume of paediatric surgical admissions, the severity of disease and the type of surgical pathology treated at our centre.
METHODS: A retrospective cohort study compared paediatric surgical admissions in an eleven-month period before COVID-19 to the same period during the pandemic. Comparisons in volume and diagnoses were based on the number of admissions. Predetermined criteria for severity of disease using triage scores, intraoperative findings and intensive care admissions were compared.
RESULTS: A total of 1 810 admissions were recorded, 1061 in the pre-COVID group and 749 during COVID. Emergency admissions reduced by 9.2%, most notably due to a reduction in trauma, caustic ingestions and constipation. There was an increase in incarcerated inguinal hernias and helminth-related pathologies. Significantly more intussusceptions failed pneumatic reduction requiring surgical intervention with bowel resection. There was a two-fold increase in patients requiring emergency intensive care.
CONCLUSION: Paediatric surgical volumes at our centre decreased during the COVID-19 pandemic. There was evidence of more advanced disease on presentation of inguinal hernias and intussusception and a generalised increased demand for emergency ICU admission.
Keywords: COVID-19, paediatric surgery, inguinal hernia, intussusception
Introduction
The emergence of the novel coronavirus SARS-CoV-2 towards the end of 2019 in Wuhan, China, and the subsequent expansion towards a global pandemic has had far-reaching consequences on healthcare provision. Compared to the adult population, children have proven to be less susceptible to infection and severe disease, possibly due to a lower expression of angiotensin-converting enzyme-2 (ACE-2) receptors within the nasal passages and, therefore, fewer viral binding sites.12 However, the "hidden" burden due to the indirect effects of the pandemic may be disproportionately large in this vulnerable population, particularly in developing countries.3
In South Africa, on 15 March 2020, the government announced a national state of disaster in response to the early identification of the first COVID-19 cases in the country.4 The enforcement of a series of strict societal limitations followed, including the banning of public gatherings, shutting of schools, restrictions of movement, banning of alcohol and tobacco, and mandatory mask-wearing in public. The country saw various iterations of these lockdown measures according to the ebb and flow of positive cases nationally for 2 years ending with the cessation of the state of disaster on 5 April 2022.5 Hospital activity underwent drastic changes too, with the closing of outpatient clinics, cessation of elective surgeries, and the redirecting of resources to COVID-testing facilities, field hospitals, medical wards, and intensive care units.
The impact of the COVID-19 pandemic and its associated restrictions on the most common paediatric surgical diseases in South Africa is largely unknown. Although some studies have noted a possible role in the pathophysiology of appendicitis, intussusception, and testicular torsion,6-11 direct interaction of the virus in surgical pathophysiology is limited. Instead, it is expected that indirect factors would greatly impact on the presentation of surgical disease. Fearful avoidance of healthcare facilities, restrictions on movement and limited transport services may have led to delays in health seeking behaviour.3,1214 Other considerable factors include the disruption to the economic or social stability of homes, the closing of schools, the interruption of vaccination services and disease prevention strategies such as routine deworming, and the pausing of food programmes.3,14,15
The primary aim of this study was to compare all paediatric surgery admissions at our facility during the height of the COVID-19 pandemic to a similar period before the pandemic in terms of age and gender, surgical volume, type of pathology, severity of disease and length of stay. The secondary aim was to perform a sub-analysis of our centre's most common surgical emergencies to determine if these were more severe on presentation during the pandemic.
Methods
Study Design
A retrospective cohort study was undertaken. The control group included all admissions to the paediatric surgical department at Tygerberg Hospital over an eleven-month period between 15 March 2019 to 15 February 2020 prior to the COVID-19 outbreak in South Africa. The study group included all admissions for the period 15 March 202015 February 2021 during the height of the COVID-19 pandemic and the national state of disaster.
Setting
Tygerberg Hospital is a tertiary hospital in Cape Town, South Africa, serving an area of the Western Cape with a population of 3.4 million people.16 Within this structure, the department of paediatric surgery serves as a referral centre for paediatric surgical care providing treatment for children from birth to 12 years of age across a broad range of pathologies.
Participants and variables
Each data entry reflects an admission of a patient treated by our department divided into pre-COVID-19 and COVID-19 groups based on the admission date. Children with a surgical disease treated by other departments were omitted, but those who were co-managed with the paediatric surgery team were included. Admissions included day case surgery and overnight hospital stays, but emergency room and ward consults were only included if surgical treatment followed. In cases where patients required multiple admissions, each was entered as a separate data entry, but readmissions for the same patient were indicated as such.
Variables captured included age, gender, diagnosis, urgency of admission (emergency vs elective), surgical procedures performed, average length of stay and features of severe or advanced disease. The diagnosis was defined by the admission's discharge summary. Elective admissions were defined as pre-scheduled hospital stays, and emergency admissions were unscheduled presentations through our emergency department or via referral. Elective procedures had been pre-booked and placed on an outpatient elective waiting list prior to the completion of surgery. Severe or advanced disease was graded using the following criteria: a TEWS (triage early warning score)17 on presentation of 5 or more or a PEWS (paediatric early warning score)18 on presentation of 3 or more, the requirement of a non-elective ICU bed and/or inotropic support.
A sub-analysis of the five most common surgical emergencies namely intussusception, appendicitis, inguinal hernia, soft tissue sepsis and trauma was performed. Disease-specific features of severe or advanced disease were defined as follows: intussusception - the failure of pneumatic reduction and/or the need for surgical resection; inguinal hernias - the presence of incarceration requiring sedation or surgery to reduce; appendicitis - an intraoperative grading score described by Gomes et al.19 of 3 or more; trauma and soft tissue sepsis - TEWS/PEWS scores of > 5 or 3 respectively or the need for inotropes or ICU admission.
Data analysis
All data were collected retrospectively by a single researcher using electronic hospital records. The RedCap™ online database system was used for data capture, and statistical analysis was performed using IBM SPSS™ software. Demographic and clinical categorical variables were cross-tabulated and compared pre- and post-COVID-19 using Pearson's chi-square tests. For variables with data groups smaller than 5, Fisher exact tests were used. Non-parametric data were compared using Mann-Whitney U tests. Significant differences between the groups were based on a probability (p-value) of < 0.05.
Results
A total number of 1 810 admissions were recorded. These included 1061 in the pre-COVID-19 group and 749 in the COVID-19 group; 239 (22.5%) of these admissions in the pre-COVID-19 group were re-admissions compared to 164 (21.9%) in the COVID-19 group (p = 0.751). The number of emergency admissions were 573 (54%) in the pre-COVID-19 group and 520 (69%) in the study group (p < 0.001).
The ratio of male to female patients was 2:1 in the pre-COVID-19 group and 1.8:1 in the COVID-19 group (p = 0.480). The mean age at presentation was 3 years and the median length of stay was 3 days in both cohorts.
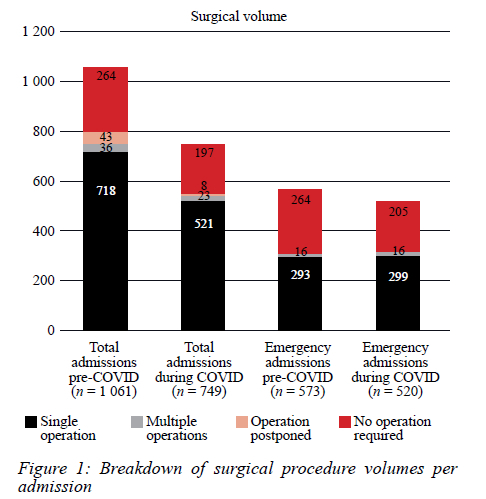
Surgical volume
Figure 1 shows a breakdown of admissions requiring surgery. There was no significant difference in the proportion of total admissions requiring surgery between the groups (pre-COVID-19 71% vs COVID-19 72%, p = 0.466). There was a small difference in the proportion of emergency admissions requiring surgery (pre-COVID-19 54% vs COVID-19 61%, p = 0.026) and the number of patients who had their surgeries postponed, (pre-COVID-19 43 vs COVID-19 8, p = 0.003).
Common diagnoses
Figure 2 reflects the most common emergency admissions per diagnosis. There was a noticeable decrease in cases of abscesses (-23%), constipation (-47%), caustic ingestions (-47%) and trauma (-53%) cases, and a marked increase in inguinal hernias presenting as emergencies (+47%) during COVID-19 (p < 0.001). Notably, there were 7 cases of complicated helminth infestation during COVID-19 compared to none pre-COVID-19 (p = 0.016).
Severity of disease
162 (33.2%) emergency admissions in the pre-COVID-19 group had PEWS or TEWS scores > 3 or 5 respectively, compared to 153 (32.7%) in the COVID-19 group (p = 0.862). In the pre-COVID-19 group, 63 (5.9%) admissions required non-elective ICU beds compared to 76 (10.1%) (p = 0.001) in the study group; 8 (0.8%) required inotropes on presentation against 14 (1.9%) (p = 0.081).
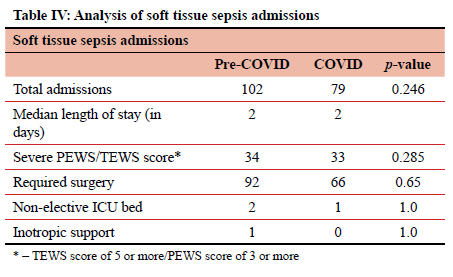
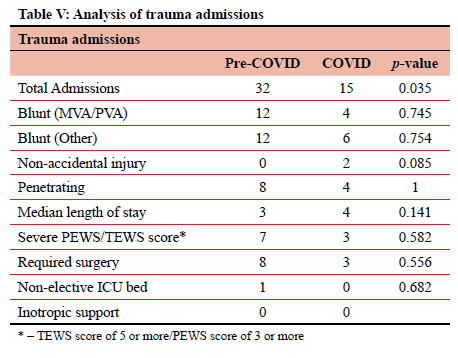
Sub-analyses of the most common surgical emergencies are depicted in Tables I-V.
Discussion
The overall reductions in admissions during COVID-19 was disproportionately due to fewer elective admissions. However, there was still a modest decrease in some emergencies. Children were more likely to be at home with adult supervision due to lockdown measures, which may explain the reduction in trauma and caustic ingestions. The reduction in abscesses may have been due hospital avoidance leading to spontaneous rupture and resolution at home, or that these were being drained at local hospitals and clinics rather than being referred. A halving in the number of constipation cases requiring admission likely reflects the chronic, indolent nature of symptoms that parents deemed appropriate to tolerate in a time of crisis. There were fewer inpatient operations cancelled or postponed during COVID-19. This excluded outpatients whose operations were delayed extensively due to the broad cancellation of elective lists. There are likely two explanations for this. Firstly, there were numerically fewer elective procedures being performed during COVID-19 with a greater proportion of emergency surgeries. Secondly, a lighter overall surgical load on our emergency surgical services during the pandemic, possibly due to a reduced trauma volume, may have allowed for more inpatient procedures to be done expediently. The equivalence in triage scores and length of stay between the two cohorts suggests overall parity of disease severity on presentation between the two groups. However, the two-fold increase in non-elective ICU admissions during a period where there were significant constraints on ICU bed availability is significant.
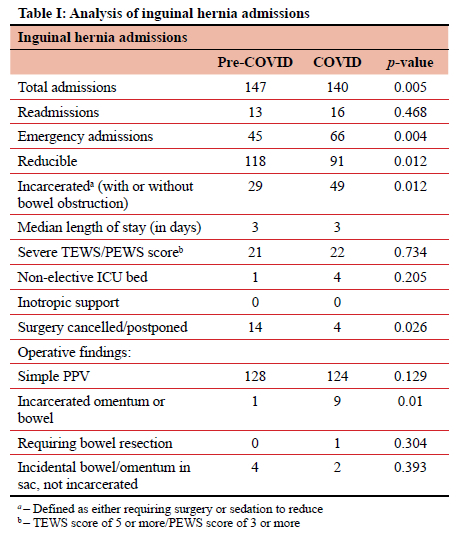
Inguinal hernias
Inguinal hernia is one of the most common problems encountered by the paediatric surgeon and this reflects accurately in our data. International studies indicate that incarceration risk of an untreated inguinal hernia in a child is between 7-12%.2021 A local study revealed a much lower incarceration rate of 4.9% in patients waiting for herniotomy.22 Most surgeons, however, would advocate for prompt surgical treatment to mitigate the risk of incarceration and strangulation.2122 The increase in cases of incarcerated inguinal hernias reflected in our data contradicts an American study reporting no increase in incarcerations due to surgical cancellations during the pandemic.23 The delay in the median interval to surgery in that study was a matter of days.23 Unfortunately, our study does not quantify the period between diagnosis and surgery, however, the significant increase in the number of incarcerated hernias seen during this period would suggest this to be significantly prolonged.
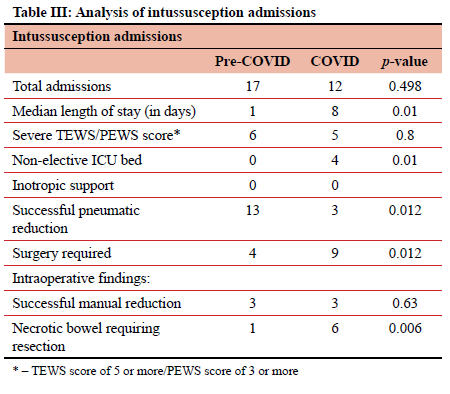
Intussusception
Intussusception is the most common cause of acute bowel obstruction in the age group between 3 months to 6 years and is a time-sensitive emergency. Delays in presentation or management lead to more significant morbidity and mortality.24 A South African study published before COVID-19, reflects a nationwide non-operative successful reduction rate far lower than international standards, with a wide variance between centres (from 67% to 9.1%), despite all employing similar technique protocols.24 In our data, the increase in failed reductions, requirement of bowel resections and ICU admissions undoubtedly reflects more advanced disease in the study group. Despite some reports suggesting that COVID-19 infection can cause severe intussusception in infants,11 none of our patients in this cohort tested positive for the virus, making a direct role of the virus in the advanced pathology unlikely.
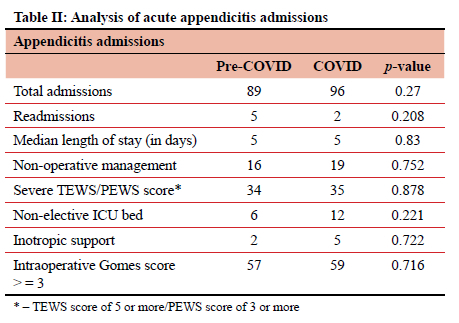
Appendicitis
Appendicitis is the single most common paediatric surgical emergency worldwide and one of the first surgical diseases to be examined in COVID-19.25 The CASCADE study in the UK analysed the management and outcomes of paediatric appendicitis during the pandemic and found that the use of diagnostic imaging and non-operative management increased, but outcomes remained relatively unaffected.25 These results were replicated in a similar study from Lithuania.26 A local study, albeit in the adult population, found no difference between severity of presentation or intraoperative findings during the pandemic.13
Our data suggest similar findings in children: - no difference in length of stay, severity of presentation or intraoperative findings during the pandemic. It should be noted that the rate of complicated appendicitis (Gomes score of 3 or more) in our pre-pandemic group was much higher (78%) than the cohort included in the UK CASCADE trial (35%) and the Lithuanian trial (35%), indicating that even prior to the pandemic, our patient population presented later and with more advanced disease than our international counterparts.25 This low-base effect may explain why there was no difference in severity of disease between pre- and COVID-19 groups in our local context.
Helminth infestation
Deworming programmes have been adopted in the Western Cape by government schools since 2009.27 With schools being closed during periods of the pandemic and local clinics also affected, the increase in complications due to worm infestation can be explained. Of the 7 cases recorded, 5 presented with partial or complete bowel obstruction, 1 presented with bile duct obstruction complicated by bile duct perforation, and 1 presented as an incidental finding in a patient with appendicitis.
Limitations of the study
Our data comes from a single centre and compares to a single period before the pandemic. All data were collected retrospectively and subject to recall bias. Some cases of paediatric surgical disease within our drainage area, especially significant polytrauma and burns, may bypass our centre and be admitted at a specialised referral unit nearby. This may lead to under-reporting of these conditions in our data. The same is true for instances where older children (> 5 years) with appendicitis or soft tissue sepsis receive surgical treatment by adult surgeons at secondary hospitals. The data compared separate admissions rather than individual patients and therefore does not reflect the true disease incidence in the population group. The study was not designed to investigate in detail the specific factors affecting the change in the pattern of surgical disease proven during COVID-19, and although reasonable explanations have been offered, these would need to be tested with further detailed study.
Conclusion
During the COVID-19 pandemic, our institution saw a significant decrease in the number of paediatric surgical admissions and paediatric surgical procedures performed. However, the number of emergency admissions and surgery performed remained relatively unchanged. There was a decrease in emergency admissions for trauma, functional constipation, abscesses and caustic ingestions. There was a significant increase in the number of helminthic complications, incarcerated inguinal hernias, and cases of intussusception requiring surgery and bowel resection during the pandemic. Similarly, there was a two-fold increase in admissions requiring an ICU bed during COVID. These findings reflect the impact on paediatric surgical disease due to disruption to the primary healthcare service and delays in presentation and/or treatment due to numerous indirect factors relating to the pandemic.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval was obtained from the University of Stellenbosch Health Research Ethics Committee of the academic institution associated with the tertiary hospital at which the study was done. Reference Number [S21/03/003_ COVID-19].
ORCID
C Kohier https://orcid.org/0000-0001-5159-9971
B Banieghbal https://orcid.org/0000-0002-0061-9669
REFERENCES
1. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3. [ Links ]
2. Yonker LM, Neilan AM, Bartsch Y, et al. Paediatric severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Clinical presentation, infectivity, and immune responses. J Paediatrics. 2020;227:45-52.e5. https://doi.org/10.1016/j.jpeds.2020.08.037. [ Links ]
3. Adu PA, Stallwood L, Adebola SO, Abah T, Okpani AI. The direct and indirect impact of COVID-19 pandemic on maternal and child health services in Africa: a scoping review. Glob Health Res Policy. 2022;7:20. https://doi.org/10.1186/s41256-022-00257-z. [ Links ]
4. Department of Co-operative Governance and Traditional Affairs. Disaster Management Act (57/2002): Directions made in terms of Section 27(2) by the Minister of Cooperative Governance and Traditional Affairs [Internet]. Government Gazette, Republic of South Africa 2020. Available from: www.gpwonline.co.za. [ Links ]
5. Department of Co-operative Governance. Disaster Management Act: Regulations - Measures to address, prevent and combat the spread of Coronavirus COVID-19: Alert level amendment [Internet]. 2022 Apr. Available from: www.gpwonline.co.za. [ Links ]
6. Malhotra A, Sturgill M, Whitley-Williams P, et al. Paediatric COVID-19 and appendicitis: A gut reaction to SARS-CoV-2? Pediatr Infect Dis J. 2021;40(2):e49-55. https://doi.org/10.1097/INE0000000000002998. [ Links ]
7. Meyer JS, Robinson G, Moonah S, et al. Acute appendicitis in four children with SARS-CoV-2 infection. J Pediatr Surg Case Rep. 2021;64:101734. https://doi.org/10.1016/j.epsc.2020.101734. [ Links ]
8. Lishman J, Kohler C, de Vos C, et al. Acute appendicitis in multisystem inflammatory syndrome in children with COVID-19. Pediatr Infect Dis J. 2020;39(12):e472-e473. https://doi.org/10.1097/INF.0000000000002900. [ Links ]
9. Bašković M, Čizmić A, Bastić M, Župančić B. The impact of the COVID-19 pandemic on the most common diagnoses in paediatric surgery: Abdominal pain, acute scrotum, upper and lower extremity injuries - tertiary centre experience. Turk Arch Pediatr. 2022;57(1):38-45. https://doi.org/10.5152/TurkArchPediatr.2022.21230. [ Links ]
10. Shields LBE, Daniels MW, Peppas DS, et al. Surge in testicular torsion in paediatric patients during the COVID-19 pandemic. J Pediatr Surg. 2022;57(8):1660-3. https://doi.org/10.1016/j.jpedsurg.2021.07.008. [ Links ]
11. Noviello C, Bollettini T, Mercedes R, et al. COVID-19 can cause severe intussusception in infants - case report and literature review. Pediatr Infect Dis J. 2021;40(11):E437-8. https://doi.org/10.1097/INF.0000000000003257. [ Links ]
12. Ahmed SAKS, Ajisola M, Azeem K, et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health. 2020;5(8):e003042. https://doi.org/10.1136/bmjgh-2020-003042. [ Links ]
13. Moustakis J, Piperidis AA, Ogunrombi AB. The effect of COVID-19 on essential surgical admissions in South Africa: A retrospective observational analysis of admissions before and during lockdown at a tertiary healthcare complex. S Aír Med J. 2020;110(9):910-5. https://doi.org/10.7196/SAMJ.2020.v110i9.15025. [ Links ]
14. Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):e901-8. https://doi.org/10.1016/S2214-109X(20)30229-1. [ Links ]
15. Coker M, Folayan MO, Michelow IC, et al. Things must not fall apart: the ripple effects of the COVID-19 pandemic on children in sub-Saharan Africa. Pediatr Res. 2021;89:1078-86. https://doi.org/10.1038/s41390-020-01174-y. [ Links ]
16. Western Cape Department of Health. Tygerberg Hospital Information Pamphlet. 2016 [cited 2022 Nov 5]; Available from: https://www.westerncape.gov.za/assets/departments/health/tygerberg_hospital_information_pamphlet_-_2016.pdf. [ Links ]
17. Gottschalk SB, Wood D, DeVries S, Wallis LA, Bruijns S; Cape Triage Group. The Cape triage score: A new triage system South Africa. Proposal from the Cape Triage Group. Emerg Med J. 2006;23(2):149-53. https://doi.org/10.1136/emj.2005.028332. [ Links ]
18. Gold DL, Mihalov LK, Cohen DM. Evaluating the paediatric early warning score (PEWS) system for admitted patients in the paediatric emergency department. Acad Emerg Med. 2014;21(11):1249-56. https://doi.org/10.1111/acem.12514. [ Links ]
19. Gomes CA, Nunes TA, Fonseca Chebli JM, Soares Junior C, Gomesy CC. Laparoscopy grading system of acute appendicitis: New insight for future trials. 2012;22(5):463-6. https://doi.org/10.1097/SLE.0b013e318262edf1. [ Links ]
20. Zamakhshary M, To T, Guan J, Langer JC. Risk of incarceration of inguinal hernia among infants and young children awaiting elective surgery. CMAJ. 2008;179(10):1001-5. https://doi.org/10.1503/cmaj.070923. [ Links ]
21. Olesen CS, Mortensen LQ, Öberg S, Rosenberg J. Risk of incarceration in children with inguinal hernia: a systematic review. Hernia. 2019;23(2):245-54. https://doi.org/10.1007/s10029-019-01877-0. [ Links ]
22. Botes SN, Edge J, Apffelstaedt JP, Sidler D. Assessment of the delayed repair of uncomplicated inguinal hernias in infants. S Afr J Surg. 2020;58(1):18-21. https://doi.org/10.17159/2078-5151/2020/v58n1a3056. [ Links ]
23. Hu A, Reiter AJ, Gerardo R, et al. Association between COVID-19 related elective surgery cancellations and paediatric inguinal hernia complications. A nationwide multicentre cohort study. Surgery (United States). 2022;172(3):989-96. https://doi.org/10.1016/j.surg.2022.05.011. [ Links ]
24. Cox S, Withers A, Arnold M, et al. Clinical presentation and management of childhood intussusception in South Africa. Pediatr Surg Int. 2021;37(10):1361-70. https://doi.org/10.1007/s00383-021-04946-7. [ Links ]
25. Bethell GS, Gosling T, Rees CM, Sutcliffe J, Hall NJ; CASCADE Study Collaborators and the RIFT Study Collaborators. Impact of the COVID-19 pandemic on management and outcomes of children with appendicitis: The Children with AppendicitiS during the CoronAvirus panDEmic (CASCADE) study. J Pediatr Surg. 2022;57(10):380-5. https://doi.org/10.1016/j.jpedsurg.2022.03.029. [ Links ]
26. Vansevičienė I, Bučinskaitė D, Malcius D, et al. Did the COVID-19 pandemic prolong the time till diagnosis and worsen outcomes for children with acute appendicitis? Medicina (Lithuania). 2021;57(11):1234. https://doi.org/10.3390/medicina57111234. [ Links ]
27. Theron M, Western Cape Education Department. WCED Minute: School based deworming programme. Specialised education support minute. 2009:0009. [ Links ]
 Correspondence:
Correspondence:
email:charliefkohler@gmail.com














