Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.3 Cape Town 2023
http://dx.doi.org/10.36303/sajs.3992
CASE REPORT
A rare occurrence of multiple intestinal atresias, with successful one-procedure resection and primary anastomosis
DM WintertonI; U JoomaI, II; SG CoxI, II
IDivision of Paediatric Surgery, Red Cross War Memorial Children's Hospital, South Africa
IIDivision of Paediatric Surgery, University of Cape Town, South Africa
SUMMARY
Intestinal atresia is a common cause of neonatal bowel obstruction. Many theories exist relating to intestinal atresia, though the best explanation is related to vascular events. Duodenal atresia is thought to be due to a developmental anomaly of the intestine. A rare combination of concomitant Type III duodenal atresia, Type III B jejunal atresia, and Type I ileal atresia is presented. The differing pathogenesis of these atresias makes the condition exceptionally rare. This patient was successfully treated, via explorative laparotomy, with resection of the atretic segments and two primary anastomoses, without the need for enterostomies or stents.
Keywords: intestinal atresia, bowel obstruction, duodenal atresia, jejunal atresia, ileal atresia
Case report
A female of 30 weeks gestation was born via normal vertex delivery. The baby had a birth weight of 1 400 g and normal Apgar scores. She was admitted for supportive oxygen therapy to the referral hospital intensive care unit (ICU).
At the booking visit, the baby's 27-year-old mother's blood group was O positive and had normal antenatal bloods, however, there were no antenatal ultrasounds performed. She had two previous children with no congenital anomalies.
Upper abdominal distension was noted eight hours post-delivery and a nasogastric tube drained bile. At that time an abdominal radiograph showed a dilated stomach with no distal bowel gas. Over the next 48 hours, the baby's abdominal distension worsened, and the bilious nasogastric aspirates increased in volume. A further abdominal radiograph revealed a "double bubble", which raised the clinical suspicion of duodenal atresia (Figure 1). The patient was transferred to Red Cross War Memorial Children's Hospital (RCWMCH) ICU for further management.

On admission, the baby required intermittent positive pressure ventilation (IPPV), and was haemodynamically stable, requiring no cardiovascular support with a normal cardiac examination and a normal echocardiogram. She did not have any overt dysmorphic features. Her abdomen was soft and not distended. There was no organomegaly and had a clean umbilical stump.
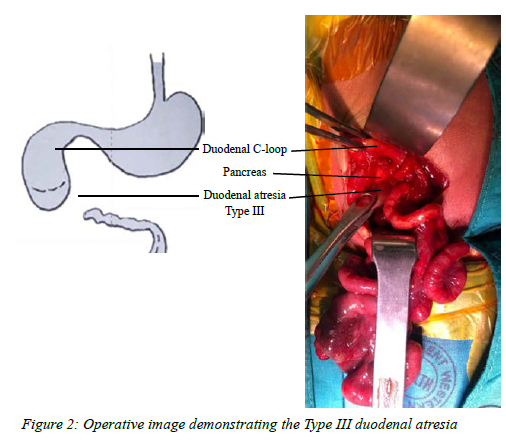
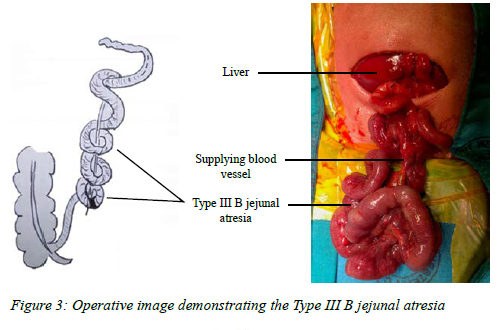
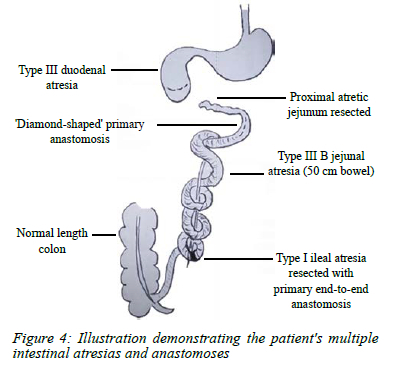
She had a hyponatraemic, hypochloraemic metabolic alkalosis that was corrected before an exploratory laparotomy, based on a presumptive diagnosis of duodenal atresia 60 hours after birth. A transverse supra-umbilical laparotomy was performed. There were multiple adhesive bands between the small bowel and colon and a dilated proximal duodenum. A Type III duodenal atresia distal to the ampulla of Vater (with bile present) was found, with no duodenum present to the left of the superior mesenteric artery (Figure 2). The proximal jejunum had an atretic segment of 2 cm, in addition to a Type III B (apple peel) jejunal atresia with 50 cm of viable small bowel (Figure 3). An enterotomy was made at the proximal jejunum and a 5 French feeding tube was inserted, the bowel was flushed with normal saline to assess distal patency. A Type I ileal atresia was also found at the distal end of the apple peel atresia. The bowel looked dusky, necessitating denotation of the apple peel which resulted in improved perfusion. The proximal jejunal atresia was resected. A transverse incision was made at the distal end of the duodenum, with a diamond-shaped anastomosis, using interrupted sutures, constructed between it and the proximal spatulated jejunum. The distal ileal atresia was resected, and a primary end-to-end anastomosis was performed (Figure 4). Another flush through the enterotomy confirmed patency of the small bowel and colon thereafter. No mesenteric defects were noted. Care was taken to return the bowel in an anatomical fashion and the abdomen was closed.
The patient was managed postoperatively in the ICU with routine care, antibiotics, analgesia, and intravenous nutritional support. Trophic feeds were commenced on the third postoperative day. On day 10 postoperatively, the baby's abdominal distension settled, she passed stool and nasogastric aspirates decreased. During weaning from intravenous nutritional support, she developed E. faecalis and K. pneumoniae septicaemia, most likely due to central line sepsis, which responded to antimicrobials and central line removal.
By the 18th postoperative day, the baby was tolerating full enteral feeds. She was discharged one month later with a weight of 2 000 g. At one- and three-month follow-ups, the baby was clinically well, tolerating full breastfeeds and gaining weight.
Histology of the resected bowel specimens returned as unremarkable small bowel compatible with intestinal atresia.
Discussion
Atresia of the gastrointestinal tract (GIT) is a common cause of bowel obstruction in the neonatal period, with jejunoileal atresias occurring most frequently.1-3 Multiple atresias in the same patient are rarer than isolated atresias. Furthermore, concomitant atresias in different parts of the GIT (duodenum and jejunoileum) occur even less frequently.1,3-6 A cohort study by Miscia et al. revealed the incidence of duodenal atresia with additional bowel atresia to be 3%.6 In our case, the patient had an exceptionally rare combination of duodenal and jejunoileal atresias with an apple peel atresia, due to the distinct differences in the pathogenesis of the two entities.4-6 Congenital intestinal abnormalities may be detected on antenatal ultrasonography, allowing appropriate high-risk antenatal follow-ups, early referral for surgery, and anticipation of potential complications.2,7 Unfortunately, our patient hadn't had such a scan and therefore presented as an emergency case.
The gut tube arises from the endoderm in the fourth week of gestation and, during the sixth week, the gut lumen is obstructed after the luminal epithelium rapidly proliferates. During the following few weeks of gestation, the lumen is slowly recanalised.7 Duodenal atresia has been hypothesised to be due to the failure or error of the recanalisation of the intestinal lumen.2,4,6,7 Disruption of duodenal rotation, during the return of the bowel to the abdomen in the 10th week of gestation, may result in arterial occlusion, malrotation and volvulus.8 Up to 50% of patients with duodenal atresia may have other systemic anomalies, which may include an annular pancreas, congenital heart disease, and intestinal malrotation.7 Duodenal atresia occurs in 1 in 6 000 to 1 in 10 000 births, and though no genetic cause may be known, it has been reported to occur in multiple members of the same family as well as those with Trisomy 21. Our patient, and her siblings, have no dysmorphic features and no significant family history, and therefore genetic causes were not suspected.
Jejunoileal atresia occurs in 1 in 1 500 to 1 in 20 000 births, of these 6-32% of patients have multiple intestinal atresias.1,2,4 Vascular events, such as infarction and mesenteric defects resulting in internal bowel herniation, best account for atresia of the jejunum, ileum, and colon.2-8 The intestinal loop is isolated and then resorbed if it has poor perfusion. Mesenteric vascular occlusions may be associated with volvulus, intussusception, malrotation, internal hernias, or tight anterior abdominal wall defects, such as gastroschisis. Intrauterine mesenteric peritonitis has been reported in patients with atresia.7 An inflammatory event or exposure to a teratogenic agent has been hypothesised by some, but this has been challenged.2,7,8 However, acute-on-chronic inflammation has been observed in patients with hereditary multiple intestinal atresia (HMIA), an autosomal recessive condition that results in numerous atresias throughout all parts of the GIT.2,4,7 Iatrogenic intestinal atresia has also been reported due to an occult omphalocele being clamped. Vascular abnormalities of the placenta may also affect intestinal perfusion and result in complex intestinal atresias. Multiple intestinal atresias have also been reported in patients with immunodeficiency.7 Our patient's histology did not demonstrate any inflammatory or infectious process, and therefore an intrauterine vascular event is hypothesised to be the cause of the described anomalies.
The surgical principles of maintaining enteral continuity and maximising bowel length were employed when treating this baby. Thus, only the atretic segments were resected with subsequent primary end-to-end anastomoses and restoration of the bowel in an anatomical fashion.3 This is supported by our patient's management and clinical success. Other surgical options, such as a possible ileostomy or damage control principles, would have been used if the baby was haemodynamically unstable or significantly nutritionally compromised. A laparoscopic approach could also have been employed; however, this would have been technically extremely challenging due to the presence of the concomitant Type III B jejunal atresia and ileal atresia. An open approach allowed the surgeon to appreciate the anatomy completely, in this rare circumstance, together with addressing all the adhesive bands to ensure the orientation of the bowel was correct once the anastomoses were complete.
Conflict of interest
The authors declare no conflict of interest.
Funding source
There are no financial or personal relationships, with others or organisations.
Ethical approval
Ethical approval was obtained from the legal guardian of the patient for the publication of the clinical case and the use of radiology and operative images.
ORCID
DM Winterton https://orcid.org/0000-0002-7678-1486
U Jooma https://orcid.org/0000-0002-9507-9289
SG Cox https://orcid.org/0000-0002-3175-8741
REFERENCES
1. Federici S, Domenichelli V, Antonellini C, Dòmini R. Multiple intestinal atresia with apple peel syndrome: successful treatment by five end-to-end anastomoses, jejunostomy, and transanastomotic silicone stent. J Pediatr Surg. 2003;38(8):1250-2. https://doi.org/10.1016/s0022-3468(03)00281-1. [ Links ]
2. Bilodeau A, Prasil P, Cloutier R, et al. Hereditary multiple intestinal atresia: thirty years later. J Pediatr Surg. 2004;39(5):726-30. https://doi.org/10.1016/j.jpedsurg.2004.01.031. [ Links ]
3. Rich B, Bott M, Spigland N. Multiple intestinal atresia with apple peel syndrome successfully treated with primary repair. J Pediatr Surg Case Rep. 2013;1(7):157-9. https://doi.org/10.1016/j.epsc.2013.05.015. [ Links ]
4. Lambrecht W, Kluth D. Hereditary multiple atresias of the gastrointestinal tract: report of a case and review of the literature. J Pediatr Surg. 1998;33(5):794-7. https://doi.org/10.1016/s0022-3468(98)90225-1. [ Links ]
5. Sasa RV, Ranko L, Snezana C, Lidija B, Djordje S. Duodenal atresia with apple-peel configuration of the ileum and absent superior mesenteric artery. BMC Pediatr. 2016;16(1):150. https://doi.org/10.1186/s12887-016-0690-y. [ Links ]
6. Miscia ME, Lauriti G, Chiesa PL, Zani A. Duodenal atresia and associated intestinal atresia: a cohort study and review of the literature. Pediatr Surg Int. 2018;35(1):151-7. https://doi.org/10.1007/s00383-018-4387-1. [ Links ]
7. Coran A, editor. Pediatric surgery. 7th ed. Philadelphia: Elsevier Saunders; 2012. p. 1051-71. [ Links ]
8. Pumberger W, Birnbacher R, Pomberger G, Deutinger J. Duodeno-jejunal atresia with volvulus, absent dorsal mesentery, and absent superior mesenteric artery: a hereditary compound structure in duodenal atresia? Am J Med Genet. 2002;109(1):52-55. https://doi.org/10.1002/ajmg.10309. [ Links ]
 Correspondence:
Correspondence:
DM Winterton
Email: devan.winterton@gmail.com














