Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.3 Cape Town 2023
http://dx.doi.org/10.36303/sajs.4012
TRAUMA SURGERY
The mortality rate of patients with open abdomen and contributing factors -a three-year audit in a major academic trauma unit
E van der MerweI; MS MoengII, III; M JoubertII; M NelI
IDepartment of General Surgery, University of the Witwatersrand, South Africa
IIDepartment of Surgery, Faculty of Health Sciences, University of the Witwatersrand, South Africa
IIITrauma Unit, Charlotte Maxeke Johannesburg Academic Hospital, South Africa
ABSTRACT
BACKGROUND: Damage control surgery (DCS) is a widely used approach in trauma. An open abdomen carries complications, increased morbidity and mortality. This study aims to quantify the mortality rate, determine contributory factors and factors influencing the decision to perform DCS and assess morbidity in patients undergoing open abdomen
METHODS: A retrospective review was conducted on 205 patients in Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit. The mortality rate was evaluated over a 24-hour, 7-day and 28-day period. Data were collected by a data collection sheet from 1 January 2016 to 31 December 2018
RESULTS: Of the 205 patients, 193 were male and the median age was 34.34 years. Penetrating trauma was the most predominant mechanism of injury in 162 (79%), with gunshot injuries seen in the majority (130/162). The mortality rate was 55/205 (26.8%) for open abdomen patients, 19/55 (34.5%) within the first 24 hours, 22/55 (40%) in the 24-hours to 7-days period, and 14/55 (25.4%) in the 8-day to 28-day period. Statistically significant factors contributing to mortality were haemodynamic instability, hypothermia, coagulopathy, massive transfusion, vasopressors, and significant associated injuries. Morbidities were entero-atmospheric fistula (EAF) in 7.3% (Clavien-Dindo grade Ilia), surgical site infection in 45.3% (Clavien-Dindo grade I) and ventral hernia in 10.24% (Clavien-Dindo grade IIIb
CONCLUSION: Most open abdomens were performed in males, with gunshot injuries being the most common mechanism. The majority of mortalities were within the 24-hours to 7-days period. The most common morbidity associated with an open abdomen was surgical site infection
Keywords: open abdomen, damage control surgery, mortality rate
Introduction
Background
South Africa is a country with a high level of trauma caused by blunt and penetrating mechanisms. In the context of abdominal trauma, a laparotomy remains one of the effective ways of assessing and treating an intra-abdominal injury.1 Damage control surgery (DCS) is a well-known and widely used approach in trauma.1 Open abdomen has become one of the cornerstones in severe trauma, compartment syndrome and severe contamination.2
The concept of DCS was introduced to civilian trauma care by Burch et al. and Rotondo et al. in the early '90s, aiming to reduce mortality in severe trauma by performing abbreviated surgery to control bleeding and contamination, followed by active resuscitation in intensive care and return to theatre for definitive repair once the physiological and metabolic insults have reversed. A key element of DCS is the need to leave the abdomen open with a temporary closure device in place.3,4
Rationale behind the open abdomen
• The need to prevent the development of abdominal hypertension and abdominal compartment syndrome.
• The need to re-examine the abdominal cavity when intestinal viability is questionable or potential residual contamination is present.
• The need to shorten the surgical time during DCS by using temporary closure techniques.
• The need to return to the peritoneal cavity to remove packs and vascular shunts and perform complex gastrointestinal anastomoses and vascular repairs.3
Factors used to decide the need for an open abdomen Clinical
• Haemodynamic status - sustained hypotension, need for inotropic support
• Intraoperative thrombocytopaenia and increased prothrombin time test (PTT) and international normalised ratio (INR)
• Severe hypothermia < 35 °C.
Metabolic
• Metabolic status - severe metabolic acidosis (pH < 7.2, base excess [BE] < -8)
• The volume of crystalloids infused during initial resuscitation
• The volume of blood infused during initial resuscitation - massive transfusion is defined as the transfusion of 50% of blood volume in 6 hours, 100% of blood volume in 24 hours or ongoing transfusions needed.
Anatomical/surgical
• Multiple injuries - lengthy operations
• Bowel oedema at the end of surgery4
Morbidities
An open abdomen carries complications, of which the most common are secondary and tertiary infections and enteric fistula formation. In addition, an open abdomen carries problems such as failure to perform anatomical fascial closure with a residual ventral hernia and the presence of stomas. These issues prolong intensive care unit (ICU) and hospital stay, delay recovery and return to a normal quality of life and impose the need for further surgeries, which add an array of new complications.2
Defined as an abnormal communication between the intestinal tract and the atmosphere, it is described in 2-43% of trauma patients. The number of laparotomies (relooks) performed and a delayed period increase the risk of these patients developing fistulae. These patients experience an ongoing cycle of repeated surgeries, continuous loss of intestinal fluid with essential electrolytes, re-infection, septic wounds, and malnutrition leading to mortality.5
Damage control resuscitation
Recent developments leading to a deeper understanding of the pathophysiology of traumatic bleeding and acute coagulopathy associated with trauma have changed the approach to the resuscitation of severely injured patients. Damage control resuscitation (DCR) was first described in 2007 in a warzone, with the emphasis on using lower volumes of crystalloids, early use of blood and blood products, permissive hypotension leading to decreased clot disruption, and the use of point-of-care coagulation testing to guide product resuscitation, allowing for a "better" resuscitated patient at the end of surgery.6
DCR is aimed at allowing volume re-expansion along with increased oxygen-carrying capacity.7 This resuscitation period is described as starting in the emergency department and continued in the theatre and ICU. These new strategies may significantly change the need to leave an open abdomen following a trauma laparotomy.8
The primary objective of the study was to (i) quantify the mortality rate of patients with an open abdomen over a 24-hour, 7-day and 28-day period in the major trauma unit of the Charlotte Maxeke Johannesburg Academic Hospital, and (ii) determine possible contributory factors to mortality. Secondary objectives were to (i) determine factors influencing the decision to perform DCS, and (ii) assess morbidity in the open abdomen patient - surgical site infection, hernia rate and entero-atmospheric fistula.
Methods
A retrospective review of patients (18 years and older) undergoing DCS and having an open abdomen post-surgery was performed. The mortality rates of these patients were assessed over a 24-hour, 7-day and 28-day period. The study was conducted at Charlotte Maxeke Johannesburg Academic Hospital Trauma ICU. Patient data were reviewed over a 3-year period from 1 January 2016 to 31 December 2018.
Retrospective data were collected from prospectively completed MediBank forms, RedCap trauma database and patient ICU files. Inclusion criteria were all patients above the age of 18 years who underwent DCS as decided by the surgeon, were transferred to ICU postoperatively for physiological optimisation, and subsequently underwent definitive surgery if they were suitable candidates. This included all patients who underwent DCS, whether they demised pre-relook, or had subsequent relooks. Exclusion criteria were patients transferred to the trauma unit with an open abdomen following a laparotomy performed at another institution.
A data collection sheet was completed for all patients included in this study. The data collection sheet included sex, age, mechanism of injury - gunshot wound (GSW), motor vehicle accident (MVA), stab and other (fall from heights, motor-bike accidents, pedestrian-vehicle accidents) - cause of injury, injury severity score (ISS) > 16, blood pressure (BP), fluids (crystalloids vs colloids) and blood given during resuscitation, factors used to decide on an open abdomen, number of laparotomies prior to definitive closure, length of ICU stay, whether the patient demised and when, and if any morbidities occurred. For this study, 24 hours post DCS was used as day one. Superficial site infection was defined as any infective changes of the skin or subcutaneous tissue requiring management.
Factors assessed to play a part in decision making for open abdomen were abnormal haemodynamics (shock defined as systolic blood pressure < 90 mmHg on arrival at emergency department), hypothermia (temperature < 35 °C), acidosis (pH < 7.2, BE < -2, lac > 2 ), coagulopathy, contamination, vasopressors, bowel oedema, severe associated injuries, massive transfusion (receiving 4 packed red blood cells, 4 fresh frozen plasma, 1 mega unit of platelets in emergency department or during surgery), complex bowel repair, packs in the abdomen, and temporary vascular shunt.
Statistical analysis and management were conducted using STATA version 14. The Mann-Whitney U test was used to assess not normally distributed variables. Chi-square and Fisher's exact tests were conducted for analysis of categorical variables. Kaplan-Meier analysis was performed to assess how time to death varied among study participants according to different characteristics (demographic, clinical). The Cox regression model was used to relate risk factors/variables which were significant in the Kaplan-Meier analysis to survival time. A _p-value of < 0.05 was considered statistically significant.
Results
During the study period, a total of205 patients who underwent DCS at Charlotte Maxeke Johannesburg Academic Hospital trauma unit were identified. The mortality rate was quantified in patients with an open abdomen. The study found that 55 (26.8%) patients with an open abdomen demised within 28 days, 19 patients (34.5%) at < 24 hours, 22 (40%) between 24 hours and 7 days, and 14 (25.46%) between 8 and 28 days. The median mortality day was found to be five days.
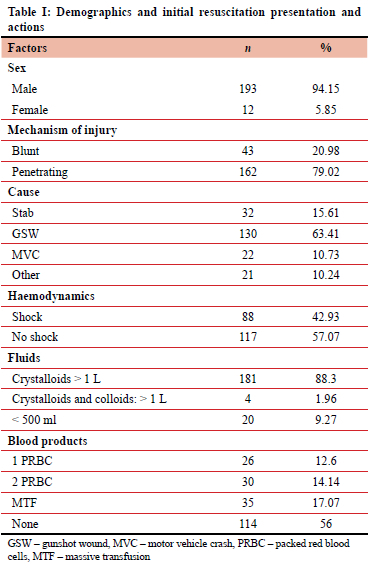
One hundred and ninety-three patients who underwent DCS were male (94.15%). Penetrating trauma accounted for 162 patients (79.02%), of which 130 (63.41%) were GSW-related. Eighty-eight patients presented in shock. One hundred and eighty-one patients (88.3%) received more than one litre of crystalloids during resuscitation, and 35 patients (17%) received enough transfusion to meet the criteria for massive transfusion.
Table I shows the demographics and initial resuscitation presentation and actions.
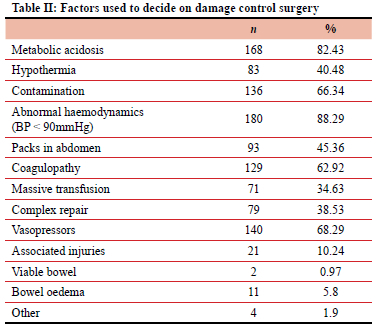
The factors shown in Table II were found to play a role in the decision to do DCS and leave the abdomen open. Our study found that the most common reasons for the surgeon to perform DCS were metabolic acidosis (168; 82.43%), contamination (136; 66.34%), abnormal haemodynamics (180; 88.29%), coagulopathy (129; 62.29%) and vasopressor usage (140; 68.29%).
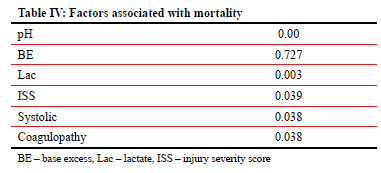
For survival analysis, the following factors were found to have statistical significance in patients who demised post DCS, as listed in Table III. The factors having a direct impact on length of survival was pH < 7.2 (p-value 0.00), lactate > 2 (p-value 0.003), ISS (p-value 0.039), systolic blood pressure < 90 mmHg (p-value 0.038) and coagulopathy (p-value 0.038), as listed in Table IV.
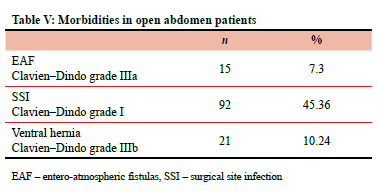
Morbidity assessment, listed in Table V, found that surgical site infection (Clavien-Dindo grade I) was the most common complication (45.36%), followed by ventral hernias (10.24%) (Clavien-Dindo grade IIIb), and then entero-atmospheric fistulas (EAFs) (7.3%) (Clavien-Dindo IlIa).
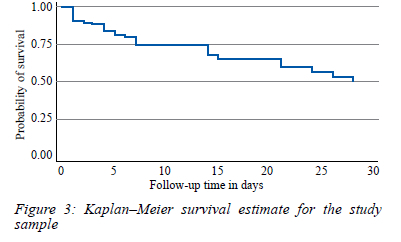
The length of ICU stay was reviewed and, as listed in Table VI, found that 26 (12.68%) patients stayed < 24 hours, 129 (62.93%) stayed 24 hours to 7 days, 36 (17.56%) stayed 8 to 28-days, and 14 (6.84%) more than one month.
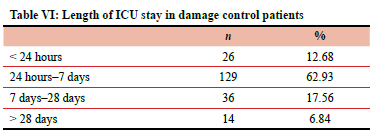
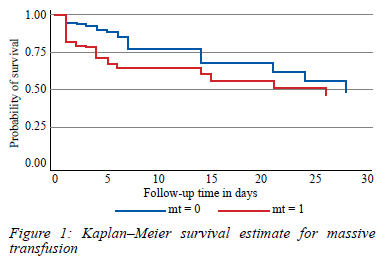
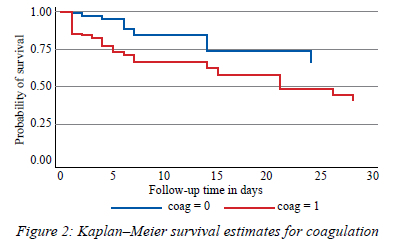
Kaplan-Meier analysis was performed to assess how time of death varied among study participants according to different characteristics. Severity of associated injuries, massive transfusion and coagulopathy were found to be of statistical significance. This is shown in Figures 1, 2 and 3.
Discussion
This retrospective study investigated patients undergoing DCS with subsequent open abdomens in ICU. The study quantifies the mortality rate in these patients, associated morbidity and factors reported to be used in deciding to employ DCS. In previous literature, DCS was associated with shorter operating times, decreased postoperative complications, and early multi-organ failure prevention.9
Mortality rate
Penetrating abdominal trauma is a major cause of hospitalisation in South Africa.11 Some of these patients require DCS due to their physiology or contamination, leading to lengthy stays in ICU, potential morbidities and mortality in an already resource-limited setting.10
The timelines chosen in this study were to try to determine at which period the patient is most vulnerable and at increased risk of mortality, to assess the length of stay and impact on the health system.
Our findings show that the majority of mortalities (40%) happen within 24 hours to 7 days. The percentage for less than 24 hours was 34.54%, and after 8 days, the mortality rate dropped to 25.46%. The median mortality was found to be five days. Compared to timelines used in previous studies, 24% were reported to demise in < 24 hours, and 27% demised > 24 hours. These studies were done on a smaller group of patients with a broader timeline but do correlate with our findings12. Local studies demonstrate a 27% mortality rate, not specifying certain time periods.11 We attribute the percentage of mortality within 24-hours-7-days to the fact that these patients are critically ill and still requiring resuscitation and correction of physiology in this time period.
In the literature, mortality rates of 64% were reported, with major causes relating to the primary injury, or complications developing from the open abdomen.13 In literature, other reported mortality rates were mentioned to be 46.7%, but the study populations were very small.14
In our study, we compared multiple variables, from the initial resuscitation to intraoperative findings. We found that the statistically significant contributions to mortality were haemodynamic instability (defined as a presenting systolic BP of < 90), hypothermia (temperature < 35 °C), metabolic acidosis (pH < 7.2), number of relooks, coagulopathy, massive transfusion, vasopressors, and associated injury.
This correlates with the recent findings of Strang and Esther that trauma patients in need of a damage control laparotomy due to acidosis, coagulopathy and hypothermia are at risk of intra-abdominal hypertension, abdominal compartment syndrome and increased mortality.15 On review of previous studies, metabolic acidosis has been associated with increased mortality rates, especially if accompanied by head injury.16
The ability to clear this acidosis, as analysed by lactate clearance, has been correlated to survival. In 1993, Abramson evaluated patients with trauma and found that if lactate was cleared within 24-hours, there was a 100% survival rate. If not, only 14% of patients would survive.17 The finding of lactate being statistically significant, but BE not, cannot be explained, as both reflect tissue hypo perfusion and correlates to metabolic acidosis. The data was reviewed again and these findings were confirmed.
The median age of those who died was 34, and of survivors was 39. In comparison to international studies, the median age of mortality varies between 39 and 55 years. Most of these studies do however have much less penetrating trauma (87% blunt, 13% penetrating), and the patients studied are older (median age 47) and mostly blunt trauma.18
The Kaplan-Meier graphs clearly demonstrate how patients receiving a massive transfusion had a higher chance of mortality at 15-days than the group without. Coagulopathy and the severity of injuries also decreased survival time significantly. Probability of survival decreased with length of stay, with a 64% chance of mortality at 15 days.
The most common factors associated with the decision to leave an abdomen open at DCS were found to be abnormal haemodynamics (88.29%), metabolic acidosis (82.43%), contamination (66.34%) as well as vasopressor usage (68.29%). The Eastern Association for the Surgery of Trauma (EAST) practice management committee performed a literature review of the management of the open abdomen in trauma and emergency general surgery in 2010. According to their published guidelines, level III evidence exists to support the use of the open abdomen technique in a trauma setting in the presence of acidosis (pH < 7.2), hypothermia (temperature < 35 °C), and clinical coagulopathy with transfusion of > 10 units of red blood cells (RBCs). Our findings indicate that the use of DCS and open abdomen in this study was in accordance with the published guidelines.19 A local study found that pH < 7.2 is the best indicator of the need for DCS. Anatomic injuries in themselves are not predictive of the need for DCS.20
Our study showed that an increased number of relooks was associated with increased survival. We attribute this to the fact that these patients were still critically ill in the first 48 hours. Some relooks were on-demand before physiology had been corrected, while others, even once taken back for a planned relook, were still unstable and at high risk for decompensation and mortality, mostly with significant other injuries. Patients having survived longer have the opportunity of going for relook laparotomies, where those who demised do not, and thus this does not advocate that more relooks decrease mortality.
The ISS was derived by Baker et al. as a standardised scoring system to assess the severity of injuries. It takes the three most severely injured compartments and adds up the squares of these.18 This has been shown in the literature to have a direct correlation to increased mortality. In our retrospective review, the higher the ISS, the higher the chances of mortality. In earlier literature, ISS was found much more elevated in non-survivors, with p-values of 0.050. This is in line with earlier studies where an ISS > 24 was associated with 25% mortality rate, > 45 had a 68% mortality rate, and > 70 had a 100% mortality rate.22
A trauma centre should have an agreement with the blood bank to have a protocol in place for massive transfusions. One study done on open abdomen patients found that an institutional protocol aimed at the early administration of blood products in a ratio of 3:2 RBC:FFP and 5:1 RBC to platelets for patients in haemorrhagic shock improved 30-day survival (56.8% vs 37.6%, p = 0.001). The patients in the protocolised arm of the study also had a significantly lower incidence of abdominal compartment syndrome (ACS) (0% vs 7%, p < 0.001). These studies were, however, performed in general surgery patients with an open abdomen.23
Morbidity
Morbidity assessment found that surgical site infection (Clavien-Dindo grade I) was the most common complication (45.36%), followed by ventral hernias (10.24%) (Clavien-Dindo grade IlIb), and then EAFs (7.3%) (Clavien-Dindo grade IIIa). In literature reviews, fistula rates were documented at 1-15% and ventral hernia formation at 25%.11 These percentages were documented after a 21-month follow-up and might be why there is a discrepancy in comparison to our findings. Our patients were either identified during admission, or at any follow-up visit, not within a specific time frame.
Further studies showed EAF (19.1%), ventral hernia (8.5%), and surgical site infections (19%). We had a large number of patients in comparison to these studies.16 Local studies demonstrate 41% of patients had a ventral hernia, with 30% undergoing delayed fascial closure.24
ICU stay
ICU stay was reviewed and found that 12% of patients stayed < 24 hours (this is mostly patients demising in this time as damage control patients do not get discharged from ICU in this short time period), 62.93% stayed 24 hours to 7 days, 17.56% were in ICU for 8 days to 28 days, and 6.84% were in ICU > 28 days.
In the literature, 25-31 days of ICU stay was reported as an average stay for these patients; in our study we found the average to be 5 days.22 In our setting, we are resource-limited and need to have a quick turnover of cases to open beds for new patients arriving in extremis. This is most likely why our patients are discharged sooner from ICU than in reported studies.
Study limitations
Study limitations included incomplete records for some patients and having to rely on accurate record keeping. The study may also be biased with limited applicability outside of the setting in which the research is conducted. As this was a retrospective study, some aspects were difficult to interpret accurately as the sample size was small, e.g., bowel oedema, bowel viability and associated injuries. The study was also performed in only one centre, and this might be attributed to certain findings. With regard to DCR, incomplete pre-hospital records are a weakness in this study as we were unable to assess the use of permissive hypotension prior to arrival in the emergency department.
Conclusion
Our data demonstrated that patients undergoing DCS are at risk of mortality due to multiple contributing factors. The majority of patients demised within 24 hours to 7 days (40%). The most common morbidity associated with an open abdomen was surgical site infection (45.46%). Open abdomen management remains an appropriate management in critically ill patients but does carry a high risk of mortality and morbidity.
Acknowledgements
This study has been made possible thanks to the encouragement, support and guidance of my supervisors Prof. Steve Moeng, Dr Marissa Joubert and Dr Marietha Nel. Prof. Moeng, acting as a mentor, set an example of how I strive to be, teaching and encouraging my growth in this journey. He is never too busy to offer guidance, with his broad knowledge, expertise and experience. I will forever be grateful for his ongoing support, and I am honoured to have done this study with him. Dr Marissa Joubert, for her clinical input and support during this dissertation, always available for a meeting and for guidance. Dr Nel without whom this would not have been possible, guiding me through every step of the research aspect, interpretation of results, proofreading multiple drafts, and help in the final submission.
Conflict of interest
The author declares no conflict of interest.
Ethical approval
This research received ethical clearance from the University of Witwatersrand Human Research Ethics Committee with clearance number M190982. Permission to perform the study was granted by the CEO of Charlotte Maxeke Johannesburg Academic Hospital.
ORCID
E van der Merwe https://orcid.org/0000-0002-1694-1564
MS Moeng https://orcid.org/0000-0001-7459-3388
M Joubert https://orcid.org/0000-0002-5255-9100
M Nel https://orcid.org/0000-0002-8206-3392
REFERENCES
1. Waibel BH, Rotondo MF. Damage control surgery: it's evolution over the last 20 years. Rev Col Bras Cir. 2012;39(4):314-21. https://doi.org/10.1590/s0100-69912012000400012. [ Links ]
2. Frazee RC,Abenathy S,JupiterD,et al. Long-termconsequences of open abdomen management. Trauma. 2013;16(1):37-40. https://doi.org/10.1177/1460408613507686. [ Links ]
3. Burch JM, Ortiz VB, Richardson RJ, et al. Abbreviated laparotomy and planned reoperation for critically injured patients. Ann Surg. 1992;215(5):476-83. https://doi.org/10.1097/00000658-199205000-00010. [ Links ]
4. Rotondo MF, Schwab CW, McGonigal MD, et al. 'Damage control': an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35(3):373-82. [ Links ]
5. Falconi M, Pederzoli P. The relevance pf gastrointestinal fistuale in vlinival practice: a revuew. Gut. 2001;49(Suppl 4):iv2-10. https://doi.org/10.1136/gut.49.suppl_4.iv2. [ Links ]
6. Godat L, Kobayashi L, Constantini T, et al. Abdominal damage control surgery and reconstruction: world society of emergency surgery position paper. World J Emerg Surg. 2013;8(1):53. https://doi.org/10.1186/1749-7922-8-53. [ Links ]
7. Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003;54(6):1127-30. https://doi.org/10.1097/01.ta.0000069184.82147.06. [ Links ]
8. Lamb CM, MacGoey P, Navarro AP, Brooks AJ. Damage control surgery in the era of damage control resuscitation. Brit J Anaesth. 2014;113(2):242-9. https://doi.org/10.1093/bja/aeu233. [ Links ]
9. Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62(2):307-10. https://doi.org/10.1097/ta.0b013e3180324124. [ Links ]
10. Asensio JA, McDuffie L, Petrone P, et al. Reliable variables in the exsanguinated patient which indicate damage control and predict outcome. Am J Surg. 2001;182(6):743-51. https://doi.org/10.1016/s0002-9610(01)00809-1. [ Links ]
11. Steenkamp CJ, Kong VJ, Clarke DL, et al. A selective vacuum assisted mesh mediated fascial traction approach following temporary abdominal containment for trauma laparotomy is effective in achieving closure. S Afr J Surg. 2018;56(4):28-32. [ Links ]
12. Cotton BA, Reddy N, Hatch QM, et al. Damage control resuscitation is associated with a reduction in resuscitation volumes and improved survival in 390 damage control laparotomy patients. Ann Surg. 2011;254(4):598-605. https://doi.org/10.1097/sla.0b013e318230089e. [ Links ]
13. Morais M, Goncalves D, Bessa-Melo R, et al. The open abdomen: analysis of risk factors for mortality and delayed fascial closure in 101 patients. Porto Biomed J. 2018;3(2):e14. https://doi.org/10.1016/j.pbj.0000000000000014. [ Links ]
14. Young UC, Seung HL, Jae GL, et al. Management of an open abdomen considering trauma and abdominal sepsis: a single-center experience. J Acute Care Surg. 2019;9(2):39-44. https://doi.org/10.17479/jacs.2019.9.2.39. [ Links ]
15. Strang SG, Esther M. Recognition and management of intra- abdominal hypertension and abdominal compartment syndrome, a survey by Dutch surgeons. Eur J Trauma Emerg Surg. 2017;43(1):85-98. https://doi.org/10.1007/s00068-016-0637-x. [ Links ]
16. Kritayakirana K, Maggio PM, Brundage S, et al. Outcomes and complications of open abdomen technique for managing non trauma patients. J Emerg Trauma Shock. 2010;3(2):118-22. https://doi.org/10.4103/0974-2700.62106. [ Links ]
17. Abramson D, Scalea TM. Lactate clearance and survival following injury. J Trauma. 1993;35(4):584-8. https://doi.org/10.1097/00005373-199310000-00014. [ Links ]
18. Boolaky KN, Tariq AH, Hardcastle TC. Open abdomen in the trauma ICU patient: who? when? why? and what are the outcome results? Eur J Trauma Emerg Surg. 2022;48(2):953-61. https://doi.org/10.1007/s00068-020-01543-6. [ Links ]
19. Diaz J, Cullinane D, Dutton WD, et al. Open abdomen in trauma and emergency general surgery. J Trauma. 2010;68(6):1425-38. https://doi.org/10.1097/ta.0b013e3181da0da5. [ Links ]
20. Weale R, Long V, Buitendag J, et al. Damage control or definitive repair? A retrospective review of abdominal trauma at a major trauma center in South Africa. Trauma Surg Acute Care Open. 2019;4(1):e000235. https://doi.org/10.1136/tsaco-2018-000235. [ Links ]
21. Baker SP, O'Neill B Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187-96. [ Links ]
22. Oshita KO, Nakahara H, Oshita A, et al. Outcomes of damage control surgery for abdominal trauma evaluated using the trauma and injury severity score and lethal triad in a single institution. Hiroshima J Med Sci. 2020;69(1):9-14. https://doi.org/10.24811/hjms.69.1_9. [ Links ]
23. Chabot E, Nirula R. Open abdomen critical care management principles: resuscitation, fluid balance, nutrition, and ventilator management. Trauma Surg Acute Care Open. 2017;2(1):e000063. https://doi.org/10.1136/tsaco-2016-000063. [ Links ]
24. Shamrock AE, Barker T, Yuen HM, et al. Management and closure of the open abdomen after damage control laparot-omy for trauma. A systematic review and meta-analysis. Injury. 2016;47(2):296-306. https://doi.org/10.1016/j.injury.2015.09.008. [ Links ]
 Correspondence:
Correspondence:
E van der Merwe
Email: estelle.vdmerwe@yahoo.com














