Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.3 Cape Town 2023
http://dx.doi.org/10.36303/sajs.4020
TRAUMA SURGERY
Surgical exploration for penetrating neck trauma - an audit of results in 145 patients
N LaherI; B Monzon-TorresII; M MauserIII
ITrauma Unit, School of Clinical Medicine, Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
IITrauma Unit, Steve Biko Academic Hospital, Faculty of Health Sciences, University of Pretoria, South Africa
IIITrauma Directorate, Department of Surgery, Chris Hani Baragwanath Academic Hospital, University of the Witwatersrand, South Africa
ABSTRACT
BACKGROUND: Selective non-operative management (SNOM) is the current gold standard for the treatment of patients with penetrating neck trauma. The policy revolves around the liberal use of computed tomography angiography (CTA) in those patients who are haemodynamically stable, irrespective of the anatomical zone of injury, aiming at reducing the incidence of negative and non-therapeutic interventions and their potential complications
METHOD: A retrospective audit of results of patients who underwent immediate surgical exploration at the Chris Hani Baragwanath Academic Hospital in Soweto between January 2010 and December 2015 was performed
RESULTS: One-hundred and forty-five (145) patients, with a median age of 28 years (range 18-67 years), predominantly males (93.8%), underwent immediate exploration. Most injuries were caused by stab wounds (92.4%) and affected zone 2 (54.1%) on the left side of the neck (69.6%). The most common presentations were active haemorrhage (29.4%), shock (24.1%) and expanding haematoma (15.1%). A major vascular injury was found in 40%, and aero-digestive organ injury in 19.3%. The rate of negative-non-therapeutic exploration in this cohort was 4.1%. Complications were recorded in 7.6%, and the overall mortality was 9.6% secondary to early uncontrolled haemorrhage, sepsis and occlusive strokes
CONCLUSION: The utilisation of SNOM with strict criteria for selection of patients who require immediate surgical exploration versus investigations with CTA results in a low rate of non-therapeutic interventions
Keywords: penetrating neck trauma, surgical exploration, selective non-operative management
Introduction
Selective non-operative management (SNOM) is the current gold standard for the treatment of patients with penetrating neck trauma (PNT). The selection of patients for surgical exploration based on clinical presentation (haemodynamic instability, hard signs) or investigations with the liberal use of computed tomography angiography (CTA) in those who are haemodynamically stable, irrespective of the anatomical zone of injury, are the cornerstones of this policy. This strategy is designed to reduce the incidence of negative and non-therapeutic interventions and their potential complications in patients with PNT.1-5
Many studies lack the significant numbers of patients managed in the busy trauma centres in South Africa due to the high incidence of interpersonal violence experienced in the country.6-11
The results of treatment in patients who require immediate surgical exploration for PNT are discussed in this study.
Methods
The Medibank (Vertical Apps CC, Johannesburg, SA) records of patients with PNT managed at the Chris Hani Baragwanath Academic Hospital Trauma Unit between 1 January 2010 and 31 December 2015 were reviewed using "penetrating neck trauma", and "immediate surgical exploration". Patients under 18 years, those with blunt trauma and incomplete records were excluded.
Data was exported to Excel worksheets and analysed using STATA (statistical package version 16, Stata Corporation, College Station, Texas, USA).
Variables included age, sex, mechanism of injury, affected neck zone, indications for surgical exploration, surgical findings, complications and mortality.
Surgical findings were defined in five categories: 1 - major vascular injuries, including injuries to the carotid, subclavian, and vertebral arteries, as well as mediastinal great vessels and major venous injuries (internal jugular and subclavian veins); 2 - aero-digestive organ injury (ADI), that included injuries to pharynx, larynx, trachea and the cervical or thoracic oesophagus); 3 - minor vascular injuries, including injuries to the named branches of the carotid and subclavian arteries and veins, other superficial branches and thoracic duct; 4 - patients with a major soft tissue injury requiring surgical haemostasis, debridement and closure, including injuries to the thyroid gland; and 5 - negative and non-therapeutic explorations, this included removal of foreign bodies and suture of skin lacerations without a finding related to the first four categories.
Age is reported as median and range; categorical variables are reported as percentages. Pearson's chi-square test or Fisher's exact test were used to determine statistical significance. A p-value equal or less than 0.05 was considered significant when applicable.
The study aimed at determining the common indication for surgery and the findings and results of surgical exploration in a high-volume centre that uses SNOM as the preferred management strategy for PNT.
Results
The database yielded records of 755 patients; 161 were initially excluded due to incomplete data. Of the remaining 594, a further 449 were also excluded as they were initially investigated with CTA, their characteristics are discussed in a separate study. The results of the 145 patients who underwent immediate surgical exploration are discussed here.
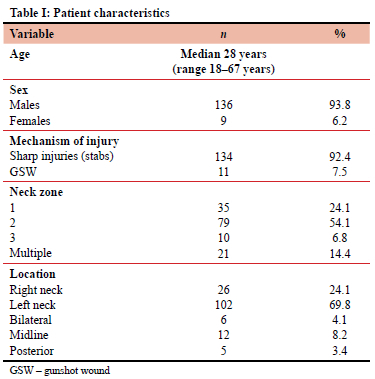
The patients had a median age of 28 years (range 1867 years), the vast majority were males (93.8%). Injuries caused by sharp objects (92.4%) were the most common mechanism of injury. Injuries affecting zone 2 (54.1%) on the left side of the neck (69.8%) predominate (Table I).
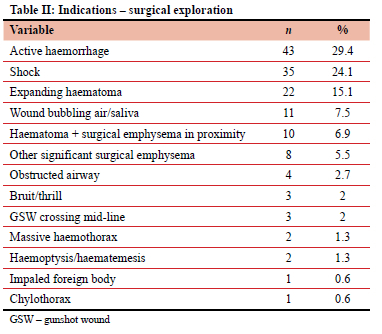
Active haemorrhage not controlled with pressure or balloon tamponade (29.4%), followed by shock (24.1%) and expanding haematoma (15.1%) were the dominant indications for surgical intervention (Table II).
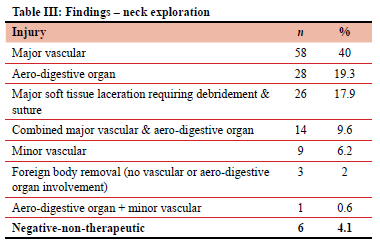
During the surgical exploration, major vascular injuries were identified in 40% of the patients and ADI were diagnosed in 19.3% of patients. Twenty-seven patients (17.9%) had major soft tissue laceration that required debridement and suture. Other findings during surgical exploration are shown in Table III. The rate of negative and non-therapeutic explorations in this series was 4.1%.
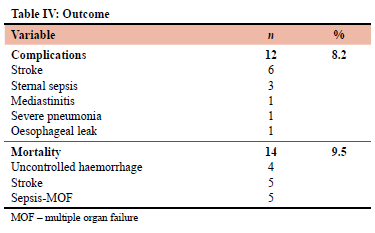
Major complications were reported in 12 patients (8.2%), and mortality in 14 (9.5%) at the expense of stroke, sepsis and uncontrolled haemorrhage (Table IV).
Discussion
There is universal agreement that SNOM is the best strategy to manage patients with penetrating neck trauma.1,3-29 The current iteration of the SNOM policy recommends that patients who are haemodynamically stable should be investigated with CTA and those who are unstable or present with "hard signs" of vascular or aero-digestive organ injury be explored, irrespective of the anatomical zone of injury ("no-zone approach"). The utilisation of SNOM has proven effective in reducing the rate of negative explorations in patients with penetrating neck trauma.1,3,4,7,11-23
This audit focused on the findings and results of treatment of 145 patients treated over 5 years who required immediate surgical exploration. Our patient demographics are similar to other local and international reports.1,3-20
When the need for surgery is determined by haemodynamic instability or the presence of hard signs, the rate of exploration ranges from 10-15%17 but can be as high as 60-62%.20,26
Active haemorrhage, shock and expanding haematomas remain the most common indications to perform surgical exploration;3,4,12-19 however, other reports have documented that the use of balloon tamponade to arrest the initial haemorrhage facilitates resuscitation and obtaining a CTA once stable, reducing even further the need for urgent surgery and the rate of negative exploration.18,19
The cohort discussed here represents nearly a quarter of patients treated at our hospital; some 70% of those had either active haemorrhage, shock or an expanding haematoma as the main indication for surgery.
The rate of negative and non-therapeutic exploration may be used to indirectly assess the accuracy of clinical and imaging diagnostic methods in patients with PNT. We found that only six of the 145 patients who underwent surgical exploration had no positive finding requiring surgical management, representing a negative exploration rate of 4.1%.
Negative exploration rates vary; when presenting clinical signs alone are used to determine need for surgery, negative explorations of 57%19 and 67%25 have been reported; more recent reports have shown a lower rate of negative explorations, mainly due to the addition of CTA to the management algorithm.10,12-15
Vascular injuries remain the prevalent findings during surgical exploration, which clearly correlates with the indications for surgery already discussed.16-18,20,25
The relative low accuracy of serial physical examination and CTA in the detection of aero-digestive organ injuries have been extensively discussed in the literature.21,22 When assessing the clinical indication for surgery in our patients, signs of aero-digestive organ involvement, such as air bubbles and saliva spillage from the wound, surgical emphysema, obstructed airway, dysphagia, haematemesis or haemoptysis were present in 17.2% of cases, which corresponds to 28 cases (19.3%) having a demonstrable injury, either involving the airway, cervical oesophagus or pharynx. A 2001 Canadian study25 found injuries involving the airway, pharynx and oesophagus in 14.6% of cases explored for PNT. One study from Stellenbosch19 found an incidence of aero-digestive organ involvement in 12.4% cases, of which 28.6% were clinically silent. Other reports, including two from military practice show similar findings.8,12-15,28,29
Missed injuries, particularly oesophageal resulting in mediastinal sepsis, as well as occlusive strokes are the most feared complications following PNT;6,7 our analysis found a complication rate of 8.2%, without missed injuries. Mahmoodie and colleagues7 reported a 9.3% complication rate, however their study included the need for intubation and tracheostomy as complications; when those are removed, the actual incidence of stroke and septic complications was zero; only deep vein thrombosis was a significant cause of morbidity in their report.
Ghnnam and colleagues6 also report a low incidence of complications (wound sepsis in 8.1% and hoarseness of voice in 4.1% of cases). No occlusive strokes were reported in their study.
The mortality rate for PNT has declined significantly over the years; better resuscitation methods, improved diagnostic modalities and postoperative care are the main reasons for this decline.28,29 Before World War II, non-operative management resulted in near absolute mortality, forcing the adoption of the mandatory exploration policy.1,3,4,21,22,28,29
Currently, mortality for PNT in civilian practice is expected to be between 2-6% or as high as 11% overall;26 mortality for major vascular injuries can be as high as 66%;26 spinal cord injury and stroke also play a significant role in civilian mortality. Of note, military reports mostly dealing with high velocity projectile injuries also showed a low mortality,28,29 similar to a civilian report of Biffl and colleagues published in 1997.27 The authors attribute these results to the availability of CTA in their management algorithm as well as shorter interval between injury and definitive surgery, the involvement of skilled surgeons and the implementation of damage control principles.
Conclusion
This study is limited by its retrospective nature, particularly the lack of information regarding the interval between injury and actual surgical exploration that could play a major role in the final outcome of patients with PNT. Despite the limitations, the results support the notion that SNOM remains the best strategy to manage patients with PNT. Surgery, using strict clinical indications for neck exploration (poor physiology-shock, hard signs) can be accomplished with a low negative exploration rate, as well as low morbidity and mortality incidence.
Conflicts of interest
The authors declare no conflict of interest.
Funding source
The study was conducted without financial support from third parties.
Ethical approval
Ethical approval for the study was obtained from the Human Research Ethics Committee (Medical) of the University of Witwatersrand (Certificate No M190123).
ORCID
N Laher https://orcid.org/0000-0002-6372-2006
B Ignacio Monzon https://orcid.org/0000-0002-3543-6352
M Mauser https://orcid.org/0000-0002-4292-3685
REFERENCES
1. Siau RTK, Moore A, Ahmed T, Lee MSW, Tostevin P. Management of penetrating neck injuries at a London trauma centre. Eur Arch Otorhinolaryngeal. 2013;270:2123-8. https://doi.org/10.1007/s00405-012-2324-9. [ Links ]
2. Shah K, Lee J, Medlej K, Weingart S, eds. Trauma. In: Practical emergency resuscitation and critical care. Cambridge: Cambridge University Press; 2013. p. 41-114. https://doi.org/10.1017/CBO9781139523936. [ Links ]
3. Prichayudh S, Choadrachata-anun J, Sriussadaporn S, et al. Selective management of penetrating neck injuries using 'no zone' approach. Injury. 2015;46:1720-5. https://doi.org/10.1016/j.injury.2015.06.019. [ Links ]
4. Shiroff AM, Gale SC, Martin ND, et al. Penetrating neck trauma: A review of management strategies and discussion of the 'no zone' approach. Am Surg. 2013;791:23-29. https://doi.org/10.1177/000313481307900113. [ Links ]
5. Low GMI, Inaba K, Chouliaras K, et al. The use of the anatomic 'zones' of the neck in the assessment of penetrating neck injury. Am Surg. 2014;8010:970-4. https://doi.org/10.1177/000313481408001013. [ Links ]
6. Ghnnam W, Al-Mastour A, Bazeed M. Penetrating neck trauma in a level II trauma hospital, Saudi Arabia. ISRN Emergency Medicine. 2012:1-6. https://doi.org/10.5402/2012/672948. [ Links ]
7. Mahmoodie M, Sanei B, Moazeni-Bistgani M, Namgar M. Penetrating neck trauma: review of 192 cases. Arch Trauma Res. 2010;11:14-18. https://doi.org/10.5812/atr.5308. [ Links ]
8. Kasbekar AV, Combellack EJ, Derbyshire SG, Swift AC. Penetrating neck trauma and the need for surgical exploration: six-year experience within a regional trauma centre. J Laryngol Otol. 2017;131:8-12. https://doi.org/10.1017/S0022215116009506. [ Links ]
9. Bordoni LS, Assis ALM, Silva GA, et al. Neck trauma deaths in Brazil: review of 541 cases. Braz J Forensic Sci. 2016;54:441-57. https://doi.org/10.17063/bjfs5(4)y2016441. [ Links ]
10. Diaz-Martinez J, Marin JC, Gruezo RB. Review of the penetrating neck injuries in 279 patients, analysis of a single institution. J Gen Surg. 2019;31:1-4. [ Links ]
11. Sethi RKV, Kozin ED, Fagenholz PJ, et al. Epidemiological survey of head and neck injuries and trauma in the United States. Otolaryngol Head Neck Surg. 2014;1515:776-84. https://doi.org/10.1177/0194599814546112. [ Links ]
12. Madsen AS, Bruce JL, Oosthuizen GV, et al. The selective non-operative management of penetrating cervical venous injuries is safe and effective. World J Surg. 2018;42(10):3202-9. https://doi.org/10.1007/s00268-018-4595-9. [ Links ]
13. Madsen A, Laing GL, Bruce JL, Oosthuizen GV, Clarke DL. An audit of penetrating neck injuries in a South African trauma service. Injury. 2016;47:64-69. https://doi.org/10.1016/j.injury.2015.07.032. [ Links ]
14. Madsen AS, Laing GL, Bruce JL, Clarke DL. A comparative audit of gunshot wounds and stab wounds to the neck in a South African metropolitan trauma service. Ann R Coll Surg Engl. 2016;98:488-95. https://doi.org/10.1308/rcsann.2016.0181. [ Links ]
15. Madsen AS, Oosthuizen GV, Laing GL, Bruce JL, Clarke DL. The role of computed tomography angiography in the detection of aerodigestive tract injury following penetrating neck injury. J Surg Res. 2016;205:490-8. https://doi.org/10.1016/j.jss.2016.06.044. [ Links ]
16. Thoma M, Navsaria P, Edu S, Nicol A. Analysis of 203 patients with penetrating neck injuries. World J Surg. 2008;32:2716-23. https://doi.org/10.1007/s00268-008-9766-7. [ Links ]
17. Van Waes OJ, Cheriex KCAL, Navsaria PH, et al. Management of penetrating neck injuries. Br J Surg. 2012;99(Suppl 1):149-54. https://doi.org/10.1002/bjs.7733. [ Links ]
18. Navsaria P, Omoshoro-Jones J, Nicol A. An analysis of 32 surgically managed penetrating carotid injuries. Eur J Vasc Endovasc Surg. 2002;24(4):349-55. https://doi.org/10.1053/ejvs.2002.1736. [ Links ]
19. Apffelstaedt JP, Müller R. Results of mandatory exploration for penetrating neck trauma. World J Surg. 1994;18:917-20. https://doi.org/10.1007/BF00299107. [ Links ]
20. Narrod JA, Moore EE. Selective management of penetrating neck injuries.A prospective study. Arch Surg. 1984;119(5):574-8. https://doi.org/10.1001/archsurg.1984.01390170070014. [ Links ]
21. Ibraheem K, Wong S, Smith A, et al. Computed tomography angiography in the "no-zone" approach era for penetrating neck trauma: a systematic review. J Trauma Acute Care Surg. 2020;89(6)1233-8. https://doi.org/10.1097/TA.0000000000002919. [ Links ]
22. Paladino L, Baron BJ, Shan G, Sinert R. Computed tomography angiography for aerodigestive injuries in penetrating neck trauma: a systematic review. Acad Emerg Med. 2021;28(10):1160-72. https://doi.org/10.1111/acem.14298. [ Links ]
23. Sperry JL, Moore EE, Coimbra R, et al. Western Trauma Association Critical Decision in Trauma: penetrating neck trauma. J Trauma Acute Care Surg. 2013;75(6):936-40. https://doi.org/10.1097/TA.0b013e31829e20e3. [ Links ]
24. Inaba K, Branco BC, Menaker J, et al. Evaluation of multidetector computed tomography for penetrating neck injury. J Trauma Acute Care Surg. 2012;72(3):576-84. https://doi.org/10.1097/TA.0b013e31824badf7. [ Links ]
25. Nason RW, Assuras GN, Gray PR, Lipschitz J, Burns CM. Penetrating neck injuries: analysis of experience from a Canadian trauma centre. Can J Surg. 2001;44(2):122-6. [ Links ]
26. Asensio JA, Valenziano CP, Falcone RE, Grosh JD. Management of penetrating neck injuries: the controversy surrounding zone II injuries. Surg ClinNorthAm. 1991;71:267-96. https://doi.org/10.1016/S0039-6109(16)45379-X. [ Links ]
27. Biffl WL, Moore EE, Rehse DH, et al. Selective management of penetrating neck trauma based on cervical level of injury. Am J Surg. 1997;174:678-82. https://doi.org/10.1016/S0002-9610(97)00195-5. [ Links ]
28. Brennan J. Head and neck trauma in Iraq and Afghanistan: different war, different surgery, lessons learned. Laryngoscope. 2013;123:2411-7. https://doi.org/10.1002/lary.24096. [ Links ]
29. Brennan J, Lopez M, Gibbon MD, et al. Penetrating neck trauma in operation Iraqi freedom. Otolaryngol Head Neck Surg. 2011;144(2):180-5. https://doi.org/10.1177/0194599810391628. [ Links ]
30. Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;859:695-702. https://doi.org/10.2471/BLT.06.037184. [ Links ]
 Correspondence:
Correspondence:
N Laher
Email: naadiyahlaher@gmail.com














