Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.3 Cape Town 2023
http://dx.doi.org/10.36303/sajs.3986
TRAUMA SURGERY
An audit of traumatic haemothoraces in a regional hospital in KwaZulu-Natal, South Africa
CM KithukaI; VC NtolaI; W SibandaII
ISchool of Clinical Medicine, College of Health Sciences, Department of General Surgery, University of KwaZulu-Natal, South Africa
IIBiostatistics Unit, Faculty of Health Sciences, Nelson Mandela University, South Africa
ABSTRACT
BACKGROUND: Haemothorax occurs in approximately 60% of all thoracic and polytrauma cases and is responsible for 15-30% of all trauma mortalities. Penetrating injuries to the thorax are a common presentation in South African hospitals. This study aims to audit the traumatic haemothoraces and their outcomes in regional hospitals in Durban, KwaZulu-Natal, South Africa
METHODS: In this study, patient characteristics were grouped as either continuous or categorical variables. Continuous variables, such as age were summarised as means (with standard deviations) or medians (interquartile range [IQR]), as appropriate. Categorical variables such as sex were summarised as proportions. Fisher's exact test was used to compare proportions. All analyses were performed using the Statistical Package for Social Sciences
RESULTS: A total of 118 patients were included comprising 110 (93%) males and eight (7%) females, with an average age of 29.7 years. Stab-chest was the most frequent mechanism of injury (76; 64.4%), followed by gunshot wound (GSW)-chest (27; 22.9%) and isolated blunt chest trauma (9; 7.6%). Other mechanisms of injury were stab-neck (3; 2.5%), stab-shoulder (2; 1.7%) and blunt chest trauma in the context of polytrauma (1; 0.8%). The most frequent type of injury was penetrating (108; 91.5%), with only 10 (8.5%) cases of blunt injury. This study found that there was a statistically significant association between patient age groups and type of injury
CONCLUSION: Haemothorax is a common sequela of chest trauma. Retained haemothorax (RH) results in worsened patient outcomes including increased hospital length of stay (LOS). This study points to the need for auditing of proper intercostal chest drain (ICD) positioning, which is crucial for the successful drainage of haemothorax
Keywords: haemothorax, VATS, thoracotomy, trauma
Background
Haemothorax (HTX) is a frequent consequence of chest injuries that occurs in approximately 60% of all polytrauma cases.1 Traumatic HTX can be due to either blunt or penetrating injury.2,3 Penetrating injuries to the thorax are a common presentation in emergency departments in South Africa due to an increase in interpersonal trauma and violent crime.4,5
The physiological response to injury consists of an early response manifesting as haemodynamic and respiratory instability and late response manifesting as empyema and fibrothorax which occur following retained haemothorax (RH). RH occurs in 5-10% of all chest injuries,6 and is a major risk factor for development of empyema and fibrothorax. These complications significantly increase overall patient morbidity and length of hospital stay (LOS).
Based on a study by Heniford et al., an algorithm was derived for use in patients with haemothoraces with tube thoracostomy being the first and most common modality of treatment.7 When this fails, strategies to circumvent these complications have included placement of additional thoracostomy tubes or early thoracotomy. In recent years, video-assisted-thoracoscopy (VAT) has emerged to provide another safe, effective and less invasive option for managing this problem.8,9 More recently, most of the published literature has focused on determining the optimal timing of VATs in the post-injury period.10-13 However, with its numerous advantages, it is yet to find a place in the algorithm used to manage HTX in third-world countries.14
This study seeks to audit traumatic haemothoraces in a regional hospital in Durban, KwaZulu-Natal, South Africa, with the aim of assessing whether there is a possibility of identifying variables that would likely predispose patients to development of RH and, in so doing, institute early aggressive surveillance and/or alternative management such as VATs to help avoid the poor outcomes related to RH.
Methods
The resuscitation room registry datasets at King Edward Hospital (KEH) and its referral hospital for cardiothoracic cases, King Dinizulu Hospital (KDH), were queried to identify adult patients with HTX who presented to the two hospitals between 1 October 2017 and 1 July 2018. Data collected from the resuscitation room registries at KEH included demographics (sex, age and area of residence), injury mechanism (blunt or penetrating), type of drain, amount of blood drained, radiological findings, blood results, LOS and further management; for patients referred to KDH for further management, data from the clinic registry was queried. All available records of patients who presented post-trauma with a blunting costophrenic angle on initial chest radiograph or fluid collection consistent with blood density on initial computed tomography (CT) imaging were considered as having HTX. Diagnosis of RH, which was defined as residual pleural blood > 500 ml in volume or blood occupying > one-third of the thoracic cavity, was made by use of chest radiograph and/or CT. In this study, outcome variables included radiological findings, progression-to-RH and LOS. Patient characteristics were grouped as either continuous or categorical variables. Continuous variables, such as age, were summarised as means (with standard deviations) or medians (interquartile range, IQR), as appropriate, and the Kolmogorov-Smirnov test was used to determine if the data was parametric or non-parametric. Categorical variables such as sex and area of residence were summarised with counts (proportions). Fisher's exact tests were used to compare proportions while means were compared using independent t-test. These analyses were performed using the Statistical Package for Social Sciences (Version 27.0. Armonk, NY: IBM Corp.) and Stata statistical software.
Results
Data collected constituted of 110 (93%) males and eight (7%) females. The average age of each patient was 29.7 ± 7.83 years, with a median age of 28.0 (IQR 23-34) years. The majority (87; 73.7%), of patients were young adults aged 19-34. Stab-chest was the most frequent mechanism of injury (76; 64.4%), followed by gunshot wound (GSW)-chest (27; 22.9%) and isolated blunt chest trauma (9; 7.6%). Other mechanisms of injury were stab-neck (3; 2.5%), stab-shoulder (2; 1.7%) and blunt chest trauma in the context of polytrauma (1; 0.8%). The majority type of injury was penetrating (108; 91.5%), with only 10 (8.5%) cases of blunt injuries. Two broad categories of progression to RH were experienced in six patients with blunt chest trauma (19.4% of total patients with RH) and 25 patients with penetrating injuries (80.6% of total patients with RH) (OR = 4.98, 95% CI 1.3-19.1, p = 0.018). A total of 109 (92.4%) patients had an intercostal chest drain (ICD) Malecot and only nine (7.6%) ICD Argyle, an observation likely due to the hospital's procurement bias for Malecot drains as opposed to PVC drains. The study, however, indicated no statistically significant association between type of drain (Argyle/Malecot) and progression to RH, using a Fisher's exact test, p = 0.240 but the odds of not progressing to RH were lower for ICD Argyle compared to ICD Malecot (OR = 0.41, 95% CI 0.10, 1.64, p = 0.10). Despite the evidence to support this observation being low, we speculate that it is likely due to the malleability of Malecot drains predisposing them to kinking that slows down or halts the drainage of haemothoraces leading to a likely progression to RH. Data on amount of initial blood drained was limited because the majority of patient records (112; 94.9%) did not provide this information; we attribute this finding to poor record keeping. In terms of severity of trauma, radiological findings indicated that most chest injuries were unilateral (100; 84.7%) and only 17 (14.4%) were bilateral. Most of the patients did not progress to RH (87; 73.7%), with only 31 (26.3%) progressing to RH. From the patient cohort, 41 patients experienced a prolonged LOS > 7 days. Out of those patients, six (14.6%) had blunt chest trauma and 35 (85.4%) had penetrating chest injuries. Most patients (77; 65.3%) had LOS < 7 days (Table I). All 31 patients with RH experienced a prolonged LOS in this study, six (19.4%) with blunt chest trauma and 25 (80.6%) with penetrating chest injuries.
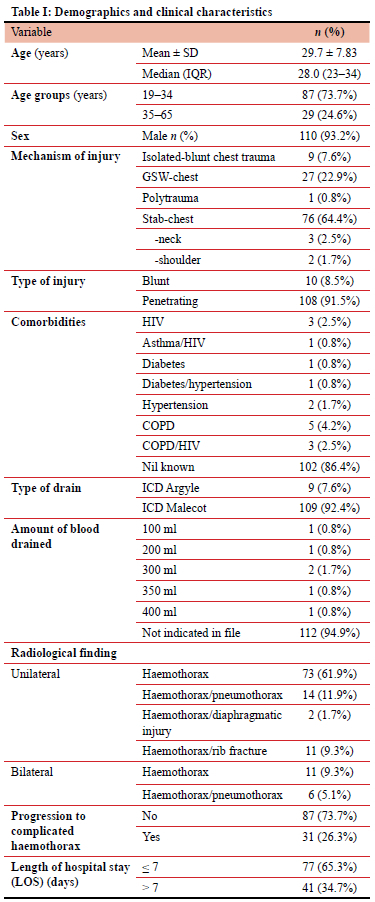
An investigation of the relationship between demographic characteristics and type of injury indicated that there was a statistically significant association between age groups and type of injury, using chi-square test, p = 0.03. Even though for both age groups, young adults (19-34 years) and middle-aged adults (35-65 years), most injuries were penetrating, a higher proportion of blunt injuries were reported among the older group (35-65 years) (5; 17.2%). The odds of having blunt injury for the younger age (19-34 years) were lower than the odds of blunt injury for the older patients (35-65 years) (odds ratio [OR] = 0.23, 95% CI 0.06, 0.93, p = 0.02) (Table II).
There was a statistically significant association between mechanism of injury and LOS, using a chi-square test of association, p < 0.00001. Within each mechanism of injury, the highest proportion of patients who stayed > 7 days in hospital were GSW-chest (84%, n = 21) and the highest proportion of patients who stayed for < 7 days in hospital were blunt-chest patients (92.5%, n = 62). The OR of < 7 days LOS for GSW-chest were OR = 0.44, 95% CI 0.11, 1.87, compared with stab-chest patients. Furthermore, OR of < 7 days LOS for stab-chest compared with blunt-chest were OR = 0.03, 95% CI 0.009, 0.13. Using a Fisher's exact test, no statistically significant association was observed between sex and LOS, p = 0.72. The OR of < 7 LOS for males was 0.66 (95% CI 0.13, 3.4) compared with females. A statistically significant association was observed between presence of other injuries and LOS, using a chi-square exact test, p = 0.0008. In investigating the effect of other injuries on LOS, the study indicated that those who had a LOS > 7 days had confirmed other injuries, while a higher proportion of patients who stayed < 7 days did not have other injuries. A statistically significant association was observed between severity of chest trauma with LOS, p < 0.00001. The majority (71%, n = 71) of unilateral injuries had LOS < 7 days, while most bilateral injuries (70.6%, n = 12) had LOS > 7 days. An OR of 5.88 (95% CI 1.9, 18.2) was observed for < 7 days LOS for unilateral chest trauma compared with bilateral chest trauma, implying that the odds of LOS < 7 days were 5.88 times higher among unilateral patients compared with bilateral patients (Table III).
There is a statistically significant association between the age group of patient and mechanism of injury, p < 0.001 (using a chi-square test). Using the same method, we found a statistically significant association between the sex of the patient and the mechanism of injury, stab chest, p < 0.001. With respect to patient's sex, we observed that males were more prone to stabs to the chest compared to females and amongst females the most prevalent mechanism of injury was GSW. In addition, our study observed a statistically significant association between patients with bilateral haemothoraces and progression to RH, p = 0.03 (Table IV).
Discussion
Following initial drainage of an HTX, approximately 20% of patients will develop an RH, increasing the odds of developing empyema and fibrothorax.15 These complications consequently lead to the requirement of morbid procedures that increase the patient's overall morbidity and hospital LOS. In this study, progression to RH was observed in 31 (26.3%), patients, however, those who developed empyema or fibrothorax and other complications were not identified in this study; early diagnostic evaluation and intervention could be credited for this observation, therefore in this study, a focus on RH specifically was placed as the complication audited.
Our study expands on previous reports documenting the detrimental impact of RH on LOS. Results revealed that sociodemographically, haemothoraces were a much more common occurrence in younger male patients (age group 19-34) with the majority of the injuries in this group being described as penetrating in nature. Blunt chest injury patterns were more commonly reported in the older (age group 35-65) population. We observed in this study that those who presented older, with bilateral chest injuries and other associated injuries on admission experienced RH and prolonged LOS. Patients who experienced high-velocity penetrating injuries (those caused by gunshot wounds) to the chest had longer LOS in comparison to those with blunt chest trauma. The study also showed a trend towards shorter LOS in the younger age group, and this could be attributed to the decreased likelihood of comorbidities in this age group allowing faster recuperation.
A focus in literature and practice is placed on identification of RH via radiographic evaluation. Approximately 20% of patients with an HTX initially managed by tube thoracostomy will continue to have a residual clot.7 Routinely, a plain chest radiograph is used to confirm proper chest tube placement and for evaluation of resolution of the HTX/PTX. This modality has, however, been shown to underestimate the amount of residual collection present. CT chest has been established to be more sensitive in this evaluation, however routine screening with this modality would not only be too expensive but would expose > 80% of patients to unnecessary radiation. In those identified with RH, about 40% will require a thoracotomy to drain residual clots,7 although in this study, patients with RH were treated more conservatively by reinserting a new thoracostomy tube and allowing dependant tube thoracostomy drainage and chest physiotherapy to facilitate improvement in lung function. If untreated, the natural history of blood in the chest is variable as some collections may absorb, develop into a fibrothorax, or become infected and become an empyema. In the recent body of literature, early intervention with VATs prior to hospital admission day 5-6 has been advocated9,16,17 as an alternative to the traditional approach of insertion of a secondary tube thoracostomy drain, use of fibrinolytics or thoracotomy. It is also associated with a shorter LOS, decreased risk of development of empyema and lower conversion to operative management, such as decortication.6,14 This is credited to the visualisation afforded by VATs that allows for a thorough inspection to assess for evidence of ongoing bleeding, evacuation of the pleural space, and accurate placement of drains to optimise ongoing drainage as necessary.6 VATs was the most common initial approach after diagnosis of RH in the 2012 AAST study, and patients managed by this approach required no further therapy in 70% of cases.7 Despite these benefits, the procedure appears to be underutilised all over the world, and while some institutions in South Africa appear to have adopted this practice in their management, it is yet to find a place in the algorithm used to manage haemothoraces in most institutions within South Africa and other third-world countries. A focus on patients likely to get RH in our population would significantly reduce the burden of the morbidity and LOS in this patient population which would be beneficial in our resource-limited environment. Our results suggest a focus placed on elderly patients, those with bilateral high-velocity injury and other associated injuries, as these groups of patients are at a heightened risk of development of RH and can therefore be more aggressively surveilled. This subset of patients would likely benefit from early VATs as part of the management algorithm in centres where this is accessible.
The insertion of ICDs is usually perceived as a trivial procedure, hence no special effort is undertaken to facilitate special training for this procedure or close supervision while it is being performed, predisposing patients to complications from improper placement. It is often performed by the casualty/emergency staff.
Study limitations
The retrospective nature of this study limited us due to the amount of information available in the medical records, part of that information includes ICD position. The initial drain output was not reported in the majority of the patients in the study biases. Although the study is relevant to our practice, raising important points, the low number of patients in the study reduced the power of the study.
Conclusion
HTX is a common sequela of chest trauma. RH results in worsened patient outcomes including increased hospital LOS. This study points to the need for auditing of proper ICD positioning, which is crucial for the successful drainage of HTX. An audit of other contributing factors such as ICD displacement, ICD blockage and lack of patient mobilisation as likely contributing factors to RH is also needed. There is a need for training ofjunior doctors in terms of management of haemothoraces. It further emphasises the importance of ICD output monitoring. Further prospective studies are required to address and minimise the risk of RH.
Acknowledgements
The authors wish to thank Sr Ntuli who assisted with the data collection process.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study protocol was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE501/18) and KZN DOH (KZ_ 201902 023). Permission to conduct the study was obtained from the Hospital Research Review Board.
ORCID
CM Kithuka https://orcid.org/0000-0002-4726-4957
VC Ntola https://orcid.org/0000-0002-9667-1591
W Sibanda https://orcid.org/0000-0001-5702-2436
REFERENCES
1. Boersma WG, Stigt JA, Smit HJM. Treatment of haemothorax. Respir Med. 2010;104(11):1583-7. https://doi.org/10.1016/j.rmed.2010.08.006. [ Links ]
2. Zeiler J, Idell S, Norwood S, Cook A. Haemothorax: a review of the literature. Clin Pulm Med. 2020;27(1):1-12. https://doi.org/10.1097/CPM.0000000000000343. [ Links ]
3. Broderick SR. Haemothorax: aetiology, diagnosis, and management. Thorac Surg Clin. 2013;23:89-96, vi-vii. https://doi.org/10.1016/j.thorsurg.2012.10.003. [ Links ]
4. Lewis C, Skinner DL. The utility of serial chest X-rays for detection of delayed pneumothorax, haemothorax or haemopneumothorax following penetrating thoracic injury. Afr J Emerg Med. 2020;10(4):215-8. https://doi.org/10.1016/j.afjem.2020.07.008. [ Links ]
5. Moodley NB, Clarke DL, Aldous C. Current trauma patterns in Pietermaritzburg. S Afr J Surg. 2015;53(4):42-44. [ Links ]
6. Meyer DM, Jessen ME, Wait MA, Estrera AS. Early evacuation of traumatic retained haemothoraces using thoracoscopy: A prospective, randomised trial. Ann Thorac Surg. 1997;64:1396-401. https://doi.org/10.1016/S0003-4975(97)00899-0. [ Links ]
7. Heniford BT, Carrillo EH, Spain DA, et al. The role of thoracoscopy in the management of retained thoracic collections after trauma. Ann Thorac Surg. 1997;63:940-3. https://doi.org/10.1016/S0003-4975(97)00173-2. [ Links ]
8. Inci I, Ozçelik C, Taçyildiz I, et al. Penetrating chest injuries: Unusually high incidence of high-velocity gunshot wounds in civilian practice. World J Surg. 1998;22:438-42. https://doi.org/10.1007/s002689900412. [ Links ]
9. Lin HL, Huang WY, Yang C, et al. How early should VATs be performed for retained haemothorax in blunt chest trauma? Injury. 2014;45:1359-64. https://doi.org/10.1016/j.injury.2014.05.036. [ Links ]
10. Huang FD, Yeh WB, Chen SS, et al. Early management of retained haemothorax in blunt head and chest trauma. World J Surg. 2018;42:2061-6. https://doi.org/10.1007/s00268-017-4420-x. [ Links ]
11. Fair KA, Gordon NT, Barbosa RR, et al. Traumatic diaphragmatic injury in the American College of Surgeons national trauma data bank: a new examination of a rare diagnosis. Am J Surg. 2015;209:864-9. https://doi.org/10.1016/j.amjsurg.2014.12.023. [ Links ]
12. Lee SS, Hyun SY, Yang HJ, et al. Comparison of penetrating and blunt traumatic diaphragmatic injuries. J Trauma Inj. 2019;32:210-9. https://doi.org/10.20408/jti.2019.034. [ Links ]
13. Prakash PS, Moore SA, Rezende-Neto JB, et al. Predictors of retained haemothorax in trauma: Results of an Eastern Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care Surg. 2020;89(4):679-85. https://doi.org/10.1097/TA.0000000000002881. [ Links ]
14. Vinck EE, Ángel EP, Barrios RV, et al. Video-assisted thoracoscopy for penetrating cardiac box injury in stable patients. Braz J Cardiovasc Surg. 2021;36:550-6. https://doi.org/10.21470/1678-9741-2020-0361. [ Links ]
15. Karmy-Jones R, Holevar M, Sullivan RJ, et al. Residual haemothorax after chest tube placement correlates with increased risk of empyema following traumatic injury. Can Respir J. 2008;15(5):255-8. https://doi.org/10.1155/2008/918951. [ Links ]
16. Morales Uribe CH, Villegas Lanau MI, Petro Sánchez RD. Best timing for thoracoscopic evacuation of retained post-traumatic haemothorax. Surg Endosc Other Interv Tech. 2008;22:91-95. https://doi.org/10.1007/s00464-007-9378-6. [ Links ]
17. Vassiliu P, Velmahos G, Toutouzas K. Timing, safety and efficacy of thoracoscopic evacuation of undrained post-traumatic haemothorax. Am Surg. 2001;67:1165-9. https://doi.org/10.1177/000313480106701210. [ Links ]
 Correspondence:
Correspondence:
VC Ntola
Email: vuyolwe@yahoo.com














