Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.2 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3900
ENDOCRINE SURGERY
Mediastinal goitre - a South African case series
I BombilI; PN MoganeII; RA MuganzaI
IDepartment of Surgery, Faculty of Health Sciences, University of the Witwatersrand, South Africa
IIDepartment of Anaesthesia, Faculty of Health Sciences, University of the Witwatersrand, South Africa
ABSTRACT
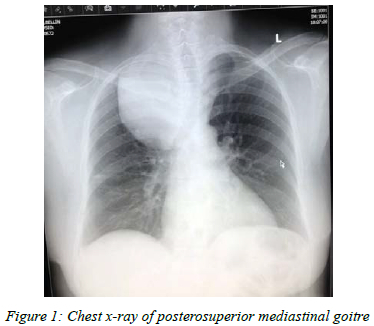
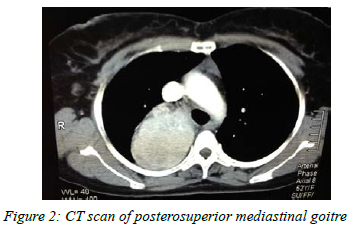
BACKGROUND: Mediastinal goitres are rare and may be diagnosed late since they are likely to manifest with non-specific cardiorespiratory symptoms especially when there is no visible cervical component. The imaging modality of choice is a contrast-enhanced computed tomography (CT) scan of the neck and chest after incidental finding of goitre on chest X-ray indicated for a condition unrelated to goitre
METHOD: This case series aims to highlight the peculiarity of mediastinal goitre in terms of clinical presentation, surgical approach, airway challenges at anaesthesia, specific complications and final histopathological report
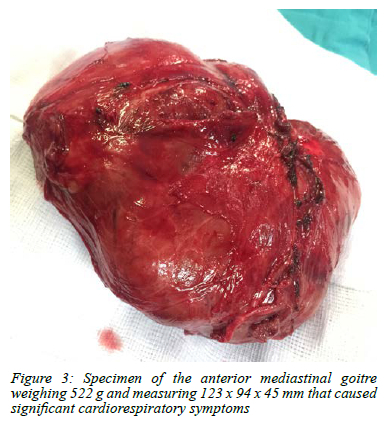
RESULTS: Over a nine-year period, four cases of euthyroid mediastinal goitre underwent sternotomy. The mean age was 57.5 years (45-71) and all patients were female. Most patients presented with non-specific cardiorespiratory symptoms. The difficult airway set was used in all cases and there were two instances of damage to the recurrent laryngeal nerve (RLN). All histopathological reports were benign
CONCLUSION: The presentation of the mediastinal goitres was atypical. Cervical incision and sternotomy were performed in all cases. There were two instances of RLN injury and no malignant histopathology. Despite the potential threat to the airway, all intubations were uneventful
Keywords: mediastinal goitre, euthyroid mediastinal goitre
Introduction
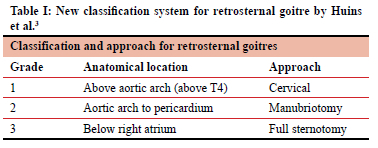
Goitre is classified by the World Health Organization (WHO) as Grade 0, 1, and 2.1 While grade 2 is noticeable on inspection and therefore allows for prompt investigations and appropriate management, grade 0 and 1 goitres will only be identified on imaging and on palpation respectively. Any retrosternal extension from grade 1 goitre (plunging goitre) is likely to manifest with atypical cardiorespiratory symptoms or may be discovered incidentally on imaging for investigation unrelated to the thyroid. Controversies arise regarding the definition of retrosternal extension of a goitre, but it is defined by DeSouza and Smith as a goitre with more than 50% of the gland located below the thoracic inlet.2 In most cases, it is possible to perform a thyroidectomy via the cervical approach alone. The shortcoming of the DeSouza and Smith classification is the inability to determine the level of mediastinal extension. Huins et al. described a classification system for goitres with retrosternal extension that is more suitable as it provides a better anatomical delineation and a well-defined surgical approach (Table I).3 The emphasis of this case report is on mediastinal goitre that we define as either a pure mediastinal goitre, or the grade 2 and 3 retrosternal goitre by Huins et al., without clinical evidence of a cervical component. The lack of a cervical component makes the diagnosis even more difficult. The delayed diagnosis can result in a goitre of significant size and subsequent pressure symptoms in the mediastinum.
Mediastinal goitres are either diagnosed in the work up of patient with superior vena cava syndrome, non-specific restrictive cardiorespiratory symptoms or incidentally during routine preoperative imaging.4,5 The largest mediastinal goitre (900 g) ever described presented with a longstanding history of respiratory symptoms associated later with stridor.4 The chest X-ray is often the initial imaging modality to identify a superior mediastinal mass that is further characterised on a CT scan. There is a paucity of literature about this rare condition, despite it being one of the most common causes of an anterosuperior mediastinal tumour (3-12%) and accounting for 0.02-0.5% of all goitres.4,5 In South Africa, Gvilia et al. from Pietersburg Hospital reported a case of retrosternal goitre that required sternotomy.6. We report our experience of mediastinal goitres diagnosed at our institution.
Objective
To describe the characteristics, clinical presentation and specific complications of mediastinal goitre treated with sternotomy at Chris Hani Baragwanath Academic Hospital (CHBAH).
Methods
In this observational descriptive study, we retrospectively reviewed all cases of mediastinal goitre treated at our institution over the past nine years (January 2013-September 2021). Parameters analysed included patient demographics, goitre characteristics (size, weight, anatomical localisation, function), clinical presentation, findings of pre- and postoperative laryngoscopy, surgical approach (sternotomy), intensive care unit (ICU) admission, comorbidity, histopathological reports, specific complications and anaesthetic considerations of the procedure.
For perspective, we also reviewed the total number of thyroidectomies performed during the study period.
All precautionary measures were taken to ensure safe anaesthesia. The cases were discussed at the multidisciplinary team (MDT) meeting that includes intensivists, anaesthetists and surgeons. The difficult airway set was available in all cases and included video laryngoscopy and bronchoscopy.
General and ENT surgeons were present during intubation in anticipation of rigid bronchoscopy. Cardiothoracic surgeons did not form part of the team.
All patients were managed with the endotracheal tube in place in the ICU postoperatively. The ICU requirement was due solely to the magnitude of surgery since there were no significant patient comorbidities.
Statistical analysis
Continuous variables are presented as means for normal distribution or as median with interquartiles ranges (IQRs) for data not normally distributed. Categorical variables are expressed as proportion by ratio or percentage.
Results
During the study period, there were four cases of mediastinal goitre out of 521 thyroidectomies performed (0.7%). All patients were female, and their mean age was 57.5 years (range 45-71 years). The patient and goitre characteristics are depicted in Table II, while patient outcomes are depicted in Table III.
Discussion
During embryology, the descent of the thyroid gland and the inferior parathyroid glands from the third pouch can arrest at any level in their course. The undescended lingual thyroid is by far the most common (90%) variation.7 Pure mediastinal goitre, arising de novo in the chest, is extremely rare.8 Embryologically, it may represent the type 4 thyroid remnant that is completely detached from the main thyroid tissue and derives its blood supply from the mediastinum.9,10 Our case series of four patients with mediastinal goitre over a nine-year period, accounting for 0.7% of all thyroidectomies performed over the same period, attests to the rarity of the condition. This incidence is slightly higher than the 0.02-0.5% reported in the literature, presumably due to the low number of thyroidectomies performed at our institution. The patients in our series presented mostly with compressive symptoms related to the mediastinal location of the goitre; those with pure mediastinal goitres were more symptomatic likely due to the more limited space in the anterior mediastinum vs the posterior mediastinum. The significant size and weight of the goitres were most likely due to the atypical presentation and the invisible cervical component that delayed diagnosis.
Surgical challenges
Sternotomy was required to deliver the goitre in all cases. The sternotomy has the benefit of providing improved access and preventing inadvertent bleeding, especially in the case of pure mediastinal goitre which derives its blood supply from the chest. Minimal access surgery is also a viable option through video-assisted thoracoscopy (VAT).11 The specimen needs to be morcellated to facilitate extraction through the port site. Minimal access thyroid surgery is not practiced at our institution.
There were two instances of recurrent laryngeal nerve (RLN) palsy (both on the right) in the cases of goitre with posterior mediastinal extension. The literature reports a higher incidence of complications related to mediastinal goitre.8 RLN palsy and temporary hypoparathyroidism can be as high as 8% and 40% respectively, whereas tracheomalacia and mortality (1.1%) are rare.8 The extension of the goitre to the posterior mediastinum moves the RLN anteriorly making it vulnerable to injury.12 Up to 32% of patients with RLN palsy may be asymptomatic, therefore both pre-and postoperative laryngoscopy is mandatory.8
It is not surprising that there was no malignancy since the most common thyroid pathology is multinodular goitre and cancer is less than 5%.5
Anaesthetic challenges
The anaesthetic management of mediastinal goitres depends on the initial assessment, and the various types of airways may be classified as "safe", "uncertain" and "unsafe" according to Erdös and Tzanova.13
The "safe" airways are managed in a conventional manner that consists of intravenous or inhalation anaesthetic drugs with neuromuscular blockade. In "uncertain" airways, the patients are allowed to breathe spontaneously until they are intubated safely. The idea is to preserve the negative intrapleural pressure which maintains the airway patent.14 The "unsafe" airways qualify for an awake fibreoptic intubation (AFOI) that requires adequate patient cooperation.15 The use of sedation and topical anaesthesia facilitates the process. The incidences of difficult intubation, difficult mechanical ventilation, and tracheomalacia are generally low.16
The management of the patient with a retrosternal goitre presents a further challenge to the perioperative anaesthetic care due to the potential threat of acute cardiopulmonary decompensation that may occur during induction.17 Literature on the topic is scanty and limited to isolated case reports and small case series. Even among the international airway experts, there is no consensus on the best plan to secure the airway.18 However, it is agreed that rigid bronchoscopy (RB) should be part of the contingency plan to secure a compromised airway. Moreover, when failure of RB is anticipated like in the case of CICV (cannot intubate, cannot ventilate) or mediastinal mass syndrome, cardiopulmonary bypass (CPB) or extracorporeal membrane oxygenation (ECMO) should be considered.19
Conclusion
In our series, all four cases of euthyroid mediastinal goitre had an atypical presentation and sternotomy was successfully performed in all cases with no morbidity. There were two instances of RLN injury and no malignant histopathology. Despite the potential threat to the airway, all intubations were successful and uneventful.
Awareness of this rare subcategory of goitre is important, as the non-specific symptoms make diagnosis challenging. An MDT approach is required to ensure adequate preparation for the anaesthetic and surgical challenges this condition poses and to ensure a successful outcome.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethical approval was obtained from the Human Research Ethics Committee of the University of the Witwatersrand and the research review board of CHBAH (clearance certificate No M211043).
ORCID
I Bombil https://orcid.org/0000-0002-4819-0785
PN Mogane https://orcid.org/0000-0002-5523-4539
RAMuganza https://orcid.org/0000-0001-5832-6095
REFERENCES
1. World Health Organization. United Nations Children's Fund, International Council for the Control of Iodine Deficiency Disorders 2007. Assessment of iodine deficiency disorders and monitoring their elimination. Geneva, Switzerland: World Health Organization; 2007. p. 14-16. [ Links ]
2. DeSouza FM, Smith PE. Retrosternal goitre. J Otorlaryngol. 1983;12:393-6. [ Links ]
3. Huins CT, Georgalas C, Mehrzad H, Tolley NS. A new classification system for retrosternal goitre based on a systemic review of its complications and management. Int J Surg. 2008;6:71-76. https://doi.org/10.1016/j.ijsu.2007.02.003. [ Links ]
4. Shah PJ, Bright T, Singh SS, et al. Large retrosternal goitre: a diagnostic and management dilemma. Heart Lung Circ. 2006;15:151-2. https://doi.org/10.1016/j.hlc.2005.10.011. [ Links ]
5. Sadler GP, Mihai R. The thyroid gland. In: Lennard TWJ, editor. Endocrine surgery. Saunders Elsevier; 2009. p. 39-72. [ Links ]
6. Gvilia T, Jonas L, Van As AB. Retrosternal goitre at Pietersburg Hospital, Limpopo Province, South Africa: a case report. S Afr Med J. 2021;111(11b):1140-1. https://doi.org/10.7196/SAMJ.2021.v111i11b.16102. [ Links ]
7. Oueriachi FE, Hammoumi MME, Arsalane A, et al. Primary mediastinal goiters. Springerplus. 2014;3:503. https://doi.org/10.1186/2193-1801-3-503. [ Links ]
8. Morita SY, Zeiger MA. Thyroidectomy for large or substernal goiters. In: Duh Q-Y, Clark OH, Kebebew E, editors. Atlas of endocrine surgical techniques. Saunders Elsevier; 2010. p. 47-59. [ Links ]
9. Agarwal A, Mishra AK, Lombardi CP, Raffaelli M. Applied embryology of the thyroid and parathyroid. In: Randolph GW, editor. Surgery of the thyroid and parathyroid glands. Saunders Elsevier; 2013. p. 15-24. [ Links ]
10. Sackett WR, Reeve TS, Barraclough B, Delbridge L. Thyrothymic thyroid tests: incidence and relationship to the thyroid gland. J Am Coll Surg. 2002;195(5):635-40. https://doi.org/10.1016/S1072-7515(02)01319-4. [ Links ]
11. Gupta P, Lau KKW, Rizvi I, Rathinam S, Waller DA. Video assisted thoracoscopic thyroidectomy for retrosternal goitre. Ann R Coll Surg Engl. 2014 Nov;96(8):606-8. https://doi.org/10.1308/003588414X14055925058634. [ Links ]
12. Gregory GW, Rameau A, Netterville JL. Surgery of cervical and substernal goiter. In: Randolph GW, editor. Surgery of the thyroid and parathyroid glands. Saunders Elsevier; 2013. p. 63-77. [ Links ]
13. Erdös G, Tzanova I. Perioperative anaesthetic management of mediastinal mass in adults. Eur JAnaesthesiol. 2009;26(8):627-32. https://doi.org/10.1097/EJA.0b013e328324b7f8. [ Links ]
14. Tan PC, Esa N. Anesthesia for massive retrosternal goiter with severe intrathoracic tracheal narrowing: the challenges imposed: a case report. Korean J Anesthesiol. 2012;62(5):474-8. https://doi.org/10.4097/kjae.2012.62.5.474. [ Links ]
15. Bacuzzi A, Dionigi G, Del Bosco A, et al. Anaesthesia for thyroid surgery: perioperative management. Int J Surg. 2008;6(Suppl 1):S82-S85. https://doi.org/10.1016/j.ijsu.2008.12.013. [ Links ]
16. Dempsey GA, Snell JA, Coathup R, Jones TM. Anaesthesia for massive retrosternal thyroidectomy in a tertiary referral centre. Br J Anaesth. 2013;111(4):594-9. https://doi.org/10.1093/bja/aet151. [ Links ]
17. Pan Y, Chen C, Yu L, Zhu S, Zheng Y. Airway management of retrosternal goitres in 22 cases in a tertiary referral centre. Ther Clin Risk Manag. 2020;16:1267-73. https://doi.org/10.2147/TCRM.S281709. [ Links ]
18. Cook TM, Morgan PJ, Hersch PE. Equal and opposite expert opinion. Airway obstruction caused by a retrosternal thyroid mass: management and prospective international expert opinion. Anaesthesia. 2011;66(9):828-36. https://doi.org/10.1111/j.1365-2044.2011.06650.x. [ Links ]
19. Wong P, Chieh Liew GH, Kothandan H. Anaesthesia for goitre surgery: a review. Proc Singapore Healthc. 2015;24(3):165-70. https://doi.org/10.1177/2010105815596095. [ Links ]
 Correspondence:
Correspondence:
Email: leilahartford@gmail.com














