Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.2 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3950
TRAUMA
The impact of thromboelastography on patients with penetrating abdominal trauma requiring intensive care
M HanningtonI; D NelI; M MillerII; A NicolI, III; P NavsariaI, III
IDepartment of General Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
IIDepartment of Critical Care, Groote Schuur Hospital, University of Cape Town, South Africa
IIITrauma Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Trauma-induced coagulopathy (TIC) is a complex multifaceted process which contributes to higher mortality rates in severely injured trauma patients. Thromboelastography (TEG) is effective in detecting TIC which assists in instituting goal-directed therapy as part of damage control resuscitation
METHODS: This retrospective study included all adult patients over a 36-month period with penetrating abdominal trauma who required a laparotomy, blood products and admission for critical care. Analysis included demographics, admission data, 24-hour interventions, TEG parameters and 30-day outcomes
RESULTS: Eighty-four patients with a median age of 28 years were included. The majority (93%; 78/84) suffered from a gunshot injury, with 75% (63/84) receiving a damage control laparotomy. Forty-eight patients (57%) had a TEG. Injury severity score and total fluid and blood product administered in the first 24 hours were all significantly higher in patients who had a TEG (p < 0.05). TEG profiles were: 42% (20/48) normal, 42% (20/48) hypocoagulable, 12% (6/48) hypercoagulable and 4% (2/48) mixed parameters. Fibrinolysis profiles were: 48% (23/48) normal, 44% (21/48) fibrinolysis shutdown and 8% (4/48) hyperfibrinolysis. Mortality rate was 5% (4/84) at 24 hours and 26% (22/84) at 30 days, with no difference between the two groups. High-grade complication rates, days on a ventilator and intensive care unit length of stay were all significantly higher in patients who did not have a TEG
CONCLUSION: TIC is common in severely injured penetrating trauma patients. The usage of a thromboelastogram did not impact on 24-hour or 30-day mortality but did result in a decreased intensive care stay and a decreased high-grade complication rate
Keywords: thromboelastography, penetrating abdominal trauma, critical care
Introduction
Uncontrolled haemorrhage with exsanguination is the leading cause of potentially preventable mortality in trauma patients, with rates of up to 40% of deaths due to haemorrhage.1-3 Despite a better understanding of trauma-induced coagulopathy (TIC), as well as a more adjusted and tailored approach to TIC, the high rate of haemorrhage-related mortality remains.4
The understanding of the fundamental factors that contribute to coagulopathy in trauma have been known for decades.4,5 However, a more intricate understanding of the clotting process has led to more directed tests and therapies being utilised.6 These ultimately act to avoid the consequences of the lethal triad of coagulopathy, hypothermia and acidosis.45 In addition, the recent discovery of the importance of calcium in coagulation, cardiac function and acid-base status has led to a fourth element making up the so called "diamond of death" in trauma patients.7 The detection and management of hypocalcaemia in severely injured trauma patients should now become ubiquitous. The cell-based understanding of haemostasis, which emphasises the importance of platelets and tissue factor, challenges the fundamentals that the conventional coagulation tests are based on and has led to more interest for the use of viscoelastic assays (VEA).46 One of the major advantages of VEA is detection of an altered fibrinolysis. This allows for assessing the balance of the risk of further bleeding against the consequences of uncontrolled harmful clotting. The assessment of which may be impossible to make without the information of a VEA.8 The aim of this study is to assess whether the use of thromboelastography (TEG) in a group of severely injured patients with penetrating abdominal trauma improves outcomes.
Materials and methods
All patients with penetrating abdominal trauma (PAT) from 1 January 2016 to 31 December 2018 (36 months) requiring a laparotomy and postoperative intensive care were included in the study. Patients over the age of 18 years, requiring a laparotomy for PAT and transfusion of any blood products during the first 24 hours of injury were included. Patients with severe traumatic brain injury were excluded. Files of all eligible patients were retrospectively reviewed, and relevant data extracted. Two groups were analysed based on whether a TEG was done. Only the results of the first TEG were examined.
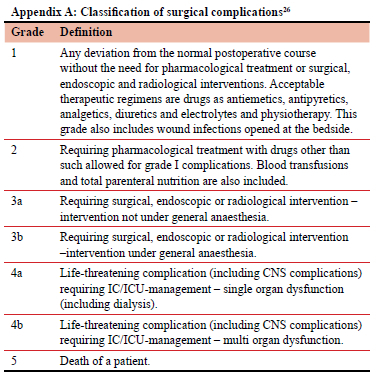
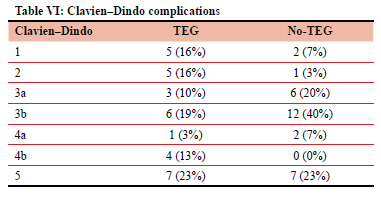
Reviewed data included basic demographics, mechanism of injury, admission vital signs and blood gas analysis. Injury severity was categorised by the penetrating abdominal trauma index (PATI), injury severity score (ISS) and the trauma and injury severity score (TRISS). Interventions in the first 24-hours including details of fluid and blood product usage and details of laparotomy were recorded. First recorded TEG parameters were analysed. Coagulation was assessed as normal, hypocoagulable, hypercoagulable or mixed based on reference range values suggested by the manufacturer. Fibrinolysis was assessed as a percentage of clot breakdown on Ly-30 and described as: normal (0.92.9%), hyperfibrinolysis (> 3%) and fibrinolysis shutdown (< 0.8%).9,10 Outcomes at 30-days included: length of stay (LOS) in ICU, ventilation days, and complications as per Clavien-Dindo (CD) categorisation. CD grading greater than two was considered high-grade (HG) complications. Mortality was determined at 24 hours and 30 days.
Analysis was performed using the R language for statistical computing (version 3.6.3, R Foundation for Statistical Computing, Vienna, Austria). Parametric numerical comparisons were done after interrogating the data for normality. Non-parametric methods were used when these assumptions failed. Data was expressed as median or mean based on this. Where central tendency for more than two continuous variables was compared, the ANOVA and Kruskal-Wallis tests were used as appropriate. Categorical data were analysed using Fisher's exact and chi-squared test of independence. An alpha-value of 0.05 was used as discriminant for significance.
Results
Description of patients
Eighty-four patients with PAT were included in the study. Seventy-eight (93%) patients sustained gunshot wounds, and the rest stab injuries. The median age was 28 (IQR 25-34) years. Forty-eight (57.1%) patients had at least one TEG performed within the first 24 hours and 36/84 (42.9%) patients did not have a TEG done. Admission parameters showed no difference between these two cohorts (Table I). Patients with a TEG had significantly higher ISS (p < 0.01) and TRISS (p = 0.02) scores. The PATI showed a median score of 28 (IQR 22-40) with no difference between the groups.
Interventions within 24 hours
All patients underwent a laparotomy. Overall, 63/84 (75%) patients had a damage control laparotomy (DCL). At 24 hours, the median number of blood products in the patients who had a TEG was: red cell concentrate (RCC) (7 [IQR 4-11] units), fresh frozen plasma (FFP) (3 [IQR 2-6]) units, platelets (1 [IQR 0-2] megaunit) and one standard issue of cryoprecipitate (cryo) (1 [IQR 0-2]). Patients who did not have a TEG done had statistically significant less blood products (p < 0.01) administered with a median of four RCC (IQR 3-5) units with no other blood products given. The overall 24-hour total fluid administered (clear fluid and blood products) was significantly different between the two groups with a median 10 150 (IQR 8 375-12 000) millilitres (ml) being administered to the TEG group and 8 320 ml (IQR 6 850-10 025) to the no-TEG group (p < 0.01) (Table II).
Coagulation and fibrinolysis profiles
Normal coagulation parameters were found in 20/48 (42%) patients. This was equalled by 20/48 (42%) patients who had hypocoagulable TEG parameters. The remaining patients had hypercoagulable (6/48; 12%), or mixed TEG parameters (2/48; 4%), demonstrating both elements of hyper and hypocoagulability. No significant differences were found between the four different coagulation phenotypes with regards to patient characteristics, admission parameters and ISS. Only patients with hypocoagulable TEG parameters received FFP (Table III). The majority of patients had normal fibrinolysis (23/48; 48%) or fibrinolysis shutdown (21/48; 44%). The remaining 4/48 (8%) of patients manifested hyperfibrinolysis. Patients with hyperfibrinolysis had significantly lower lactate (2.7 [IQR 1.9-3.3]), 24-hour total fluid (7 300 ml [IQR 6 525-7 900]) and 24-hour blood products (p < 0.05). All other parameters when compared across the three groups did not demonstrate statistical significance as depicted in Table IV.
Outcomes
The overall mortality rate was 5% (4/84) at 24 hours and 26% (n = 22) at 30 days (Table V). All four mortalities occurring in the first 24 hours demonstrated a hypocoagulable TEG. Two of these patients had a normal fibrinolysis profile and the other two had fibrinolysis shutdown. No mortalities occurred within 24 hours in the patients who did not have a TEG done. Thirty-day mortality was 31% (15/48) in patients who had a TEG done and 19% (7/36) in patients with no TEG (p = 0.33). No difference in mortality at 24 hours or 30 days was demonstrated in patients with different coagulation and fibrinolysis profiles (Tables IV and V). HG complication rate, days on a ventilator and ICU LOS were all significantly higher in patients who did not have a TEG done (p < 0.01). No statistically different rates of HG complications were noted in the different coagulation and fibrinolysis groups (Tables III and IV). Table VI lists the complications as per CD classification in the two groups.
Discussion
TEG has evolved as the gold standard test to recognise TIC. A better understanding of the complexities of coagulation has led to an increased utilisation of viscoelastic assays. It is also reliable and effective in guiding damage control resuscitation.4,8,11
This retrospective study analysed the TEGs of severely injured patients with PAT. The two cohorts, those who had a TEG and those who did not, were comparable except for a higher ISS and TRISS in the patients who had a TEG. The premise that more severely injured patients had TEGs done in this study was supported by a significantly higher 24-hour total fluid requirement and blood product usage seen in this group. Despite this, the 24-hour and 30-day mortality rates were not significantly different. This is in keeping with a systematic review which showed no mortality advantage associated with the usage of VEA in trauma patients.6 Three quarters of patients underwent damage control surgery (DCS) with an overall mortality of 5% (4/84) and 26% (22/84) at 24 hours and 30 days, respectively. The high mortality rate of 50% associated with DCS as reported at the turn of the century have improved.12 Local studies have reported mortality rates of 29-60% associated with DCS in trauma patients.13-16 There was a higher rate of HG complications (CD > 3) and ICU LOS in patients who did not have a thromboelastogram. This is in keeping with the current trauma literature that demonstrates lower complication rates and decreased ICU stay in patients receiving a VEA to guide resuscitation.2,11,17 This may be the result of more limited fluid volumes and absence of unnecessary blood products that may have been utilised if not directed by VEA. In our study, the higher complication rate despite lower overall fluid volumes needs to be interpreted in the context of the sample size and the retrospective nature of the study.
Hypocoagulability was the most frequent (42%) abnormal finding, followed by hypercoagulability (12%) and mixed parameters (4%). A large study by Moore et al. evaluating the coagulation status of 2 540 severely injured trauma patients (median ISS 25) demonstrated 15% hypocoagulable, 38% hypercoagulable and 11% mixed parameters on initial TEG.18 In contrast to our study, the majority of patients (83%) sustained blunt trauma and all TEGs were conducted within an hour of injury, which may explain the difference in coagulation phenotypes. Plotkin et al. retrospectively reviewed 44 patients with penetrating trauma and showed that 52% of patients manifested a hypocoagulable state within the first 24 hours of injury. Similar median ISS and 24-hour blood product usage may make this study of exclusively penetrating trauma patients a more contextually relevant comparator to our study. However, the Plotkin et al. study did not elaborate on the anatomic details of injury or surgical intervention required.19
Hypercoagulability may vary considerably within the first 24 hours following injury. This may be affected by injury mechanism and severity, clear fluid and blood products or tranexamic acid (TXA) administration.19 TXA was administered to 35% (17/48) of patients who received a TEG in our study, with only 5% (5/48) requiring TXA based on a prolonged Lysis-30 result on the TEG. A mix of hypercoagulability and hypocoagulability may also be present in the same patient following trauma. This is a result of a combination of tissue injury and a state of shock working in opposing mechanisms.4,18 This initial mixed state often transitions to a hypercoagulable state in the 48 hours following trauma. A large prospective study of 948 trauma patients found that 10% of patients were hypercoagulable at some point in the first 24 hours following injury.20 This is in keeping with our findings of a hypercoagulable state in 12% (6/48) of patients. None of these patients died within the first 24 hours. However, a 30-day mortality rate of 50% (3/6) was found in this group. This is consistent with other reports that show an increase in delayed mortality in patients with hypercoagulable TEGs. This is likely a result of sepsis, thrombotic complications or organ failure in severely injured patients.18
There was a trend toward higher 24-hour total fluid and blood product administration in hypocoagulable patients, although this did not reach statistical difference. Despite this, 30-day mortality and HG complication rate was lowest in hypocoagulable patients when compared to the other groups with abnormal TEG parameters. Again, this did not reach statistical significance, likely owing to the small sample size. This is in contrast to a study by Johansson et al. who demonstrated a higher rate of ventilator days, renal replacement therapy and mortality in patients with a hypocoagulable state on admission to ICU.21 In their cohort of all comers to ICU, 42% of patients were hypocoagulable with a 30-day mortality of 42%. This compares to our study of 42% (20/48) of patients being hypocoagulable with a 30-day mortality of 40% (8/20). Only four (5%) mortalities occurred in the first 24 hours and all four of these patients were hypocoagulable. This is in keeping with a study by Branco et al. who reported the 24-hour mortality rates in patients with the following coagulation profiles as: hypercoagulable (0%), normal (6%) and hypocoagulable (28%).22
The ideal response following trauma is to establish a balance of arresting ongoing haemorrhage without causing harmful thrombosis.18 Both hyperfibrinolysis and fibrinolysis shutdown have been implicated in higher mortality rates in the trauma population.4,9,10,23 Three distinct phenotypes, namely normal or physiological fibrinolysis, hyperfibrinolysis and fibrinolysis shutdown, have been used to evaluate fibrinolysis in previous studies.9,10 In this study, the two dominant phenotypes were normal (48%) and fibrinolysis shutdown (44%), with hyperfibrinolysis only present in four (8%) patients. This is a similar distribution to a large study of 2 540 patients by Moore et al. which described fibrinolysis shutdown as the most predominant phenotype at 46% and hyperfibrinolysis the least at 18%.10
In contrast to that study, which reported the highest mortality with hyperfibrinolysis (34%), no deaths or HG complications were seen in the four patients with hyperfibrinolysis in this study.10 The small study sample may have contributed to this difference. The patients in our study with hyperfibrinolysis had a significantly lower lactate and 24-hour clear fluid and blood product administration than the other two groups with a trend to lower ISS and TRISS, which did not reach statistical difference. Independent effects of hypothermia and acidosis on fibrinolysis have been evaluated on in vitro24 and in vivo (porcine) models.25 Both of these studies demonstrated no significant effect of induced hypothermia or acidosis on the fibrinolytic system as measured by thromboelastometry.24,25 These are in keeping with our results which also showed no difference in pH or temperature across the fibrinolysis phenotypes. All patients with confirmed hyperfibrinolysis received TXA.
The retrospective observational nature of this study and small sample size are the major limiting factors when considering whether these results are generalisable to a local population. In addition, although the local policy adopts a 1:1:1 ratio of blood products, the execution is dependent on the surgical and anaesthetic team involved. The timing of the TEG was also at the discretion of the treating physicians and as such no standard timing of the acquisition of a TEG was undertaken, although all the TEGs that were included were attained within the first 24 hours of injury.
Conclusion
TIC is commonly found in severely injured penetrating trauma patients. Forty-two per cent of patients with PAT requiring a laparotomy and postoperative critical care admission were hypocoagulable. This group showed a high mortality of 40%. While only 12% of our patients portrayed a hypercoagulable profile, fibrinolysis shutdown was seen in 44% of patients. This latter group showed a high mortality rate of 38%. The overall use of TEG did not impact on 24-hour or 30-day mortality but did result in a decreased intensive care stay and a lower HG complication rate.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
This study was approved by the University of Cape Town Human Research Ethics Committee HREC Ref no.: 545/2019.
ORCID
M Hannington https://orcid.org/0000-0002-4346-9656
D Nel https://orcid.org/0000-0002-3265-1049
M Miller https://orcid.org/0000-0001-6137-7723
A Nicol https://orcid.org/0000-0001-5181-1151
P Navsaria https://orcid.org/0000-0002-5152-3317
REFERENCES
1. Nystrup KB, Windelev NA, Thomsen AB, Johansson PI. Reduced clot strength upon admission, evaluated by thromboelastography (TEG), in trauma patients is independently associated with increased 30-day mortality. Scand J Trauma Resusc Emerg Med. 2011;19:52. https://doi.org/10.1186/1757-7241-19-52. [ Links ]
2. Gonzalez E, Moore EE, Moore HB, et al. Goal-directed Haemostatic resuscitation of trauma-induced coagulopathy 2017;263:1051-9. https://doi.org/10.1097/SLA.0000000000001608. [ Links ]
3. Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: The PROPPR randomised clinical trial. JAMA. 2015;313:471-82. https://doi.org/10.1001/jama.2015.12. [ Links ]
4. Kornblith LZ, Moore HB, Cohen MJ. Trauma-induced coagulopathy: the past, present, and future. J Thromb Haemost. 2019;17:852-62. https://doi.org/10.1111/jth.14450. [ Links ]
5. Rossaint R, Cerny V, Coats TJ, et al. Key issues in advanced bleeding care in trauma. Shock. 2006;26:322-31. https://doi.org/10.1097/01.shk.0000225403.15722.e9. [ Links ]
6. Da Luz LT, Nascimento B, Shankarakutty AK, Rizoli S, Adhikari NKJ. Effect of thromboelastography (TEG®) and rotational thromboelastometry (ROTEM®) on diagnosis of coagulopathy, transfusion guidance and mortality in trauma: descriptive systematic review. Crit Care. 2014;18:1-26. https://doi.org/10.1186/s13054-014-0518-9. [ Links ]
7. Wray JP, Bridwell RE, Schauer SG, et al. The diamond of death: Hypocalcemia in trauma and resuscitation. Am J Emerg Med. 2021;41:104-9. https://doi.org/10.1016/j.ajem.2020.12.065. [ Links ]
8. Dhara S, Moore EE, Yaffe MB, Moore HB, Barrett CD. Modern management of bleeding, clotting, and coagulopathy in trauma patients: what is the role of viscoelastic assays? Curr Trauma Rep. 2020;6:69-81. https://doi.org/10.1007/s40719-020-00183-w. [ Links ]
9. Moore HB, Moore EE, Gonzalez E, et al. Hyperfibrinolysis, physiologic fibrinolysis, and fibrinolysis shutdown. J Trauma Acute Care Surg. 2014;77:811-7. https://doi.org/10.1097/TA.0000000000000341. [ Links ]
10. Moore HB, Moore EE, Liras IN, et al. Acute fibrinolysis shutdown after injury occurs frequently and increases mortality: a multicentre evaluation of 2540 severely injured patients. J Am Coll Surg. 2016;222:347-55. https://doi.org/10.1016/j.jamcollsurg.2016.01.006. [ Links ]
11. Spahn DR, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:1-74. https://doi.org/10.1186/s13054-019-2347-3. [ Links ]
12. Shapiro MB, Jenkins DH, Schwab CW, Rotondo MF. Damage control: Collective review. J Trauma and Acute Care Surgery. 2000;49:969-78. https://doi.org/10.1097/00005373-200011000-00033. [ Links ]
13. Boolaky KN, Tariq AH, Hardcastle TC. Open abdomen in the trauma ICU patient: who? when? why? and what are the outcome results? Eur J Trauma Emerg Surg. 2020;48:953-61. https://doi.org/10.1007/s00068-020-01543-6. [ Links ]
14. Oshun N, Hardcastle TC. Validation of the mortality prediction equation for damage control surgery in an independent severe trauma population. S Afr J Surg. 2015;53:3-5. [ Links ]
15. Twier K, Hartford L, Nicol A, et al. Indications, mortality and long-term outcomes of 50 consecutive patients undergoing damage control laparotomy for abdominal gunshot wounds. J Surg Trauma. 2019;7:76-85. https://doi.org/10.32592/Jsurgery.2019.7.3.101. [ Links ]
16. Timmermans J, Nicol A, Kairinos N, et al. Predicting mortality in damage control surgery for major abdominal trauma. S Afr J Surg. 2010;48:6-9. [ Links ]
17. Schöchl H, Nienaber U, Maegele M, et al. Transfusion in trauma: thromboelastometry-guided coagulation factor concentrate-based therapy versus standard fresh frozen plasma-based therapy. Crit Care. 2011;15(2):R83. https://doi.org/10.1186/cc10078. [ Links ]
18. Moore HB, Moore EE, Liras IN, et al. Targeting resuscitation to normalization of coagulating status: Hyper and hypocoagulability after severe injury are both associated with increased mortality. Am J Surg. 2017;214:1041-5. https://doi.org/10.1016/j.amjsurg.2017.08.036. [ Links ]
19. Plotkin AJ, Wade CE, Jenkins DH, et al. A reduction in clot formation rate and strength assessed by thromboelastography is indicative of transfusion requirements in patients with penetrating injuries. J Trauma. 2008;64(2 Suppl):S64-68. https://doi.org/10.1097/TA.0b013e318160772d. [ Links ]
20. Müller MCA, Balvers K, Binnekade JM, et al. Thrombo-elastometry and organ failure in trauma patients - a prospective cohort study. Crit Care. 2014;18:1-8. https://doi.org/10.1186/s13054-014-0687-6. [ Links ]
21. Johansson PI, Stensballe J, Vindelev N, Perner A, Espersen K. Hypocoagulability, as evaluated by thromboelastography, at admission to the ICU is associated with increased 30-day mortality. Blood Coagul Fibrinolysis. 2010;21:168-74. https://doi.org/10.1097/MBC.0b013e3283367882. [ Links ]
22. Branco BC, Inaba K, Ives C, et al. Thromboelastogram evaluation of the impact of hypercoagulability in trauma patients. Shock. 2014;41:200-7. https://doi.org/10.1097/SHK.0000000000000109. [ Links ]
23. Kashuk JL, Moore EE, Sawyer M, et al. Primary fibrinolysis is integral in the pathogenesis of the acute coagulopathy of trauma. Ann Surg. 2010;252:434-42. https://doi.org/10.1097/SLA.0b013e3181f09191. [ Links ]
24. Shenkman B, Budnik I, Einav Y, et al. Model of trauma-induced coagulopathy including haemodilution, fibrinolysis, acidosis, and hypothermia: Impact on blood coagulation and platelet function. J Trauma Acute Care Surg. 2017;82:287-92. https://doi.org/10.1097/TA.0000000000001282. [ Links ]
25. Martini WZ, Pusateri AE, Uscilowicz JM, et al. Independent contributions of hypothermia and acidosis to coagulopathy in swine. J Trauma. 2005;58:1002-10. https://doi.org/10.1097/01.TA.0000156246.53383.9F. [ Links ]
26. Clavien PA, Barkun J, De Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-96. https://doi.org/10.1097/SLA.0b013e3181b13ca2. [ Links ]
 Correspondence:
Correspondence:
P Navsaria
Email: pradeep.navsaria@uct.ac.za