Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.2 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3852
TRAUMA
Interpretation of emergency CT angiograms in vascular trauma - vascular surgeon vs radiologist
P ParagI, II; TC HardcastleIII, IV
IDepartment of Radiology, Inkosi Albert Luthuli Central Hospital, South Africa
IIDepartment of Radiology, Nelson R Mandela School of Clinical Medicine, University of KwaZulu-Natal, South Africa
IIITrauma and Burns Services, Inkosi Albert Luthuli Central Hospital, South Africa
IVDepartment of Trauma and Surgery, Nelson R Mandela, School of Clinical Medicine, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: This study aims to investigate any discrepancy in interpretation of computed tomography (CT) angiograms (CTA) in suspected traumatic arterial injury by vascular specialists and radiology specialists, and the influence of any discrepancies on patient outcome
METHODS: A prospective observational comparative study of 6-month duration was undertaken at a tertiary hospital in Durban, South Africa. Haemodynamically stable patients with suspected isolated vascular trauma admitted to a tertiary vascular surgery service who underwent a CTA on admission were reviewed. The interpretations of CTAs were compared between vascular surgeons, vascular trainees and radiology trainees with the consultant radiologist report as the gold standard comparator
RESULTS: Of 131 CTA consultant radiologist reports, the radiology registrar concurred with 89%, which was less than the vascular surgeon who correctly interpreted 120 out of 123 negative cases with three false positives. There were no false negatives or descriptive errors. A 100% sensitivity (95% CI 63.06-100) and 97.62% (95% CI 93.20-99.51) specificity was noted for the vascular surgeon. Overall agreement was 97.71 % with Cohen's kappa value = 0.83 (95% CI 0.64-1.00) indicating very good agreement. Apart from three negative direct angiograms, patient management and outcome were not impacted by the vascular surgeons' errors in interpretation
CONCLUSION: There is very good inter-observer agreement in the interpretation of CTAs in trauma between the vascular surgeon and radiologist with no negative impact on patient outcome
Keywords: CT angiogram, vascular trauma, injury, interpretation, surgeon
Introduction
In severe trauma, radiology is key to the early diagnosis and management of the injured patient. Computed tomography (CT) scanning is utilised as an important diagnostic tool in the assessment of trauma patients.1 CT angiography (CTA) is a non-invasive and rapid imaging technique with high sensitivity and specificity in the detection of vascular injuries.2 CTA is considered the initial diagnostic imaging examination of haemodynamically stable patients with suspected arterial injuries.3 The use of Duplex Doppler ultrasonography for diagnosis in the emergency setting has not been widely used where CT scanners are available as it has a lower sensitivity and is dependent on operator skill.4-7 The urgent nature of trauma and in particular vascular injury necessitates accuracy and speed in diagnosis and management.
Emergency CT scans are usually interpreted by the attending doctor and plans to manage the patient are implemented before the formal radiological report is available.1 This is particularly true in the case of vascular trauma patients where time is of the essence to prevent catastrophic haemorrhage, critical ischaemia and its sequelae including amputation.
In recent years, radiology department workloads have increased. Worldwide and particularly in low- and middle-income countries (LMICs), the availability of radiologists is inadequate.8-11. In low-income countries, there are 1.9 radiologists per million inhabitants.12 In South Africa in 2016, 913 radiologists were registered with the Health Professions Council of South Africa and Statistics South Africa (Stats SA) estimated the mid-year population as 55.91 million which equates to 16.3 radiologists per million people.13,14 This is in sharp contrast to the 97.9 radiologists per million inhabitants in high-income countries.12
Delays in imaging reporting and possible delayed urgent patient management are consequences of radiologist shortages.15 In the local scenario, several institutions with CT scanners in our catchment area do not have radiologists or after-hours radiological cover. The formal radiological report may be delayed even if the radiologist is on site as the radiologist may be reporting other emergency CT scans or be out of the reporting suite performing a fluoroscopic procedure or an ultrasound. Thus, the clinician becomes the primary interpreter of the emergency CT scan and manages the patient on the basis of his/her interpretation.16,17
The aim of this study was to investigate if there was a significant discrepancy in interpretation of emergency CT angiograms in suspected arterial injury by the vascular surgeon, radiology registrar and radiologist and to determine whether any discrepancies had an impact on patient management. The degree and extent of inter-observer agreement between the radiology trainee and consultant radiologist was also investigated.
Material and methods
This prospective observational study was conducted over a 6-month period (1 April-30 September 2016) at the Inkosi Albert Luthuli Central Hospital (IALCH), an academic tertiary hospital in Durban. IALCH is a Trauma Society of South Africa accredited level 1 trauma centre and at the time of the study, was the only state institution with a dedicated vascular surgery service in the KwaZulu-Natal Province.
Vascular surgery in South Africa is a subspecialty qualification obtained by general surgeons. CTA interpretation was done by the sub-specialist trainee in most cases. The IALCH vascular surgery department accepts patients from any hospital throughout the KwaZulu-Natal Province.
The study population comprised all patients (adults and children) accepted and/or admitted by the vascular surgeon to IALCH with suspected blunt or penetrating vascular trauma who underwent CTA of a single body part, namely chest, neck or extremity. Only patients with soft signs (non-expanding haematoma, diminished/unequal pulses and arterial proximity) were included. Patients with hard signs were taken directly to theatre if haemodynamically unstable or underwent direct angiography with a view to endovascular intervention by the vascular surgeon. Patients with concomitant head injury or polytrauma were excluded as they were managed by a multidisciplinary specialist team.
CTAs were performed on the relevant body part with the Siemens Definition Flash Dual Source Scanner (256 slice) or Siemens Somatom 128 slice Multidetector CT Scanner (Siemens AG, Wittelsbacherplatz, Germany). Intravenous contrast medium, Iohexol 350 mg/ml (Omnipaque™, GE Healthcare) was administered using an injector via a peripheral cannula to obtain precise arterial phase CT scan images. Post processing comprised reconstructed 3 mm axial, sagittal and coronal images, 3-D reformations using maximum intensity projections and volume rendering algorithms. These images were sent to the picture archiving and communications system (PACS).
The radiology registrar stays on site after hours and is responsible for the reporting of cases.
The vascular surgeon requests the CT scan from the radiology registrar, who due to the heavy workload and logistics in radiology is rarely able to report on the CTA immediately. The vascular trainee reviews the images as soon as the scan is complete, records the findings in the patient's electronic patient record on the Hospital Information System (HIS) and acts on their interpretation.
All CTAs reported by the radiology trainee during normal and after-hours, were reviewed by a consultant radiologist with a minimum of 5 years of experience. The consultant radiologist's interpretation of the CTA was the gold standard. If any errors were detected by the consultant radiologist in the report issued by the radiology registrar, the clinician was informed, and the report amended. The radiology registrars interpreting the CT scans were in the second, third or final year of training. Patient management and outcome were accessed from the clinical notes in the electronic patient record on the IALCH HIS.
The site and type of vascular injury were described. The types of injury were described as: intimal tear, dissection, aneurysm/pseudoaneurysm, extravasation, transection, thrombosis and arterio-venous fistula. Descriptive errors were also documented. These were vicinity injuries that were not accurately identified anatomically. The principal investigator compared the initial vascular surgeon interpretation of the CT scan, radiology trainee report and final radiological report.
Statistical analysis was performed using SPSS (Version 21.0. IBM, Armonk, NY). Using the consultant radiologist report as the gold standard, inter-rater reliability was assessed for the vascular surgeon and radiology registrar. Kappa values were calculated to measure inter-observer agreement: < 0.20 = poor; 0.21-0.40 = fair; 0.41-0.60 = moderate; 0.61-0.80 = substantial/good; 0.81-1.00 = very good/almost perfect.18A _p-value of < 0.05 and 95% confidence intervals (CIs) were used to indicate statistical significance.
Results
CTAs of the extremities, neck or chest were performed on 134 patients who met the inclusion criteria. Three patients were excluded owing to suboptimal CT scan images. Of the remaining patients, 113 were male and 18 were female. The age demographics are depicted in Figure 1. The majority of patients were in the 18-30-year age group.
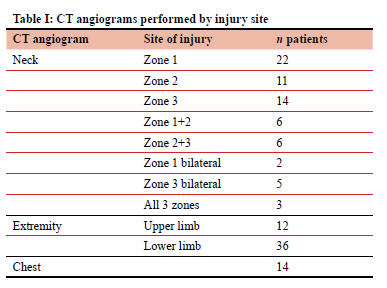
Of the 131 CTAs performed, 53% were of the neck. Table I summarises the CTAs by site of injury.
The interval between the completion of the scan and the availability of the radiology registrar's report varied between 23-247 minutes, with the majority (75%) of reports being issued within 120 minutes. The majority of suspected injuries were caused by stabs (50%) followed by gunshot wounds (GSW 34%). Motor vehicle collisions (MVC) and pedestrian-motor vehicle collisions (PMVC) accounted for 10% of the total. Two dog bites, an angle grinder injury and a vigilante hanging were the other adult aetiologies. One 3-year-old who sustained gunshot wounds and a 5-year-old child who had blunt trauma were the only children in the study cohort. Of the two patients older than 70 years, one sustained a fall and the other was involved in an MVC. Figure 1 shows the mechanisms of trauma by age group.
The soft sign indications for imaging were non-expanding haematoma in 12 patients (9.2%), diminished pulse in 27 patients (20.6%) and arterial proximity (chest and neck) in 92 patients (70.2%).
The consultant radiologist, as the gold standard, interpreted 123 (94%) out of 131 CTAs as normal and eight (6%) as abnormal. Of the positive CTAs, five were due to penetrating trauma and all cases had diminished pulses.
The vascular surgeon correctly identified 120 out of 123 negative cases with three false positives. No false negatives were identified. A 100% sensitivity (95% CI 63.06-100) and 97.6% (95% CI 93.2-99.5) specificity was noted for the vascular surgeon. The false positive rate was 2.44% and the positive predictive value (PPV) was 72.7% (95% CI 46.689.1). Concordance analysis revealed a concordance rate of 97.76% between the vascular surgeon and the radiologist. The difference in interpretation was not significant at p < 0.05. Overall agreement was 97.7 % with Cohen's kappa value = 0.83 (95% CI 0.64-1.00) indicating very good agreement.
There were 109 negative cases and eight positive cases correctly identified by the radiology registrar, compared to the radiologist interpretation, resulting in 89.1% overall agreement. The interpretations differed in 14 out of the total of 131 cases (10.7%) and the difference was statistically significant (p < 0.01). The 14 discrepant cases comprised nine false positives and five cases with descriptive error. The false positive rate was 7.32%. No false negatives were identified. Considering the 14 discrepant cases, the concordance rate was 90.35% with a kappa value of 0.49 (95% CI 0.27-0.71) indicating moderate overall agreement.
CTA positive findings correctly interpreted by the vascular surgeon and the radiology registrar were right superior thyroid artery contrast extravasation, intimal tear of left common carotid artery and occluded left vertebral artery.
Two CTAs were incorrectly reported as positive by both the vascular surgeon and radiology registrar with the same incorrect description (left subclavian artery intimal tear, left axillary artery pseudoaneurysm) in patients with gunshot wounds due to streak artefact. Two-thirds of the false positive interpretations by the radiology registrar were reported as arteriovenous fistula (AVF).
In the three CTAs interpreted as false positive by the vascular surgeon, the patients underwent urgent after-hours catheter-directed digital subtraction angiograms which were negative.
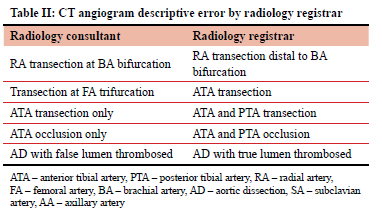
The descriptive errors by the radiology registrar (Table II) did not have an impact on the management of the patient or outcome since these were correctly interpreted by the vascular surgeon.
Discussion
The high trauma burden and scarcity of radiologists in Africa emphasise the importance of the vascular surgeon's interpretation of a CT scan. Vascular injury is particularly time sensitive as life or limb are often at risk. There is only one study detailing errors in the interpretation of CTAs and none comparing the evaluation of vascular trauma CTAs between radiologists and non-radiologists.19 There have also been only a few studies internationally comparing the interpretation of body CT scans between surgeons and radiologists.20,21 One study evaluated surgical resident interpretation of CT of the head, chest, abdomen and pelvis in acute injury in which the surgical resident was accurate in 96% of CT head interpretation, 67% CT chest and 94% CT abdomen and pelvis.21 Studies have concluded that surgical residents can accurately interpret critical radiographic and CT brain images in the trauma setting with no change in clinical outcome as compared to the consultant radiologist interpretation.22,23
Wong et al. found a low error rate in surgical resident interpretation of after-hour CT scans of the head and abdomen in trauma with no impact on patient management or outcome.1 In a study comparing radiology resident and attending radiologist interpretation of torso CT scans at a level 1 trauma centre, no adverse patient effects were directly attributable to discrepant interpretations.24 Discrepancy rates in radiology resident and consultant radiologist interpretation of emergency CT scans (non-traumatic and traumatic) vary from 0.9-26%.25-29
This study demonstrates that the vascular surgeon can correctly interpret CTAs in trauma with an accuracy of 97.7%. The concordance rate between the vascular surgeon and the consultant radiologist was 97.8%. The three false positives by the vascular surgeon accounted for the discrepancy. This discrepancy was clinically but not statistically significant, as patient management was altered, and patients were subjected to conventional catheter-directed angiography which subsequently excluded an injury. Patient management was impacted, however patient outcome was not impacted as there were no angiographic complications, and the patient was discharged the next day.
The good concordance in this study was probably due to the interpretation of the scans being done by surgeons who were subspecialist trainees in vascular surgery or qualified vascular surgeons who have routine experience in the interpretation of CTAs in the elective setting and had the benefit of pre-scan clinical evaluation. The CTAs incorrectly reported as positive by both the vascular surgeon and the radiology registrar with the same incorrect description in patients with gunshot wounds were due to streak artefact. False positive interpretations as AVF by the radiology registrar were artefactual and probably reported incorrectly due to radiology registrar inexperience. However, an over-read remains better than a missed injury and can be defined with additional imaging. Fortunately, all the cases with false positives and descriptive errors reported by the radiology registrar were correctly identified by the vascular surgeon with no negative impact on patient management. This discrepancy may have affected outcome had the vascular surgeon not examined the images in person, just relying on the registrar report, a common practical error in clinical practice. A study by Meyer et al. reported a 13.5% discrepancy rate between interpretations by on-call radiology residents and attending physicians of neck CT angiograms but no adverse clinical outcome was detected.30 These are consistent with the findings in this study.
There have been non-trauma studies addressing the degree of agreement between radiologists and radiology residents' interpretations of CT pulmonary angiograms in an emergency context with very good interobserver agreement (kappa values ranging from 0.70-0.81).31-34 Interobserver agreement was reported as good for CT venograms with a kappa of 0.66 (95% CI 0.55-0.77).31 The overall agreement between the radiology registrar and the consultant radiologist in the present study was 89.1%, with a kappa of 0.49 (95% CI 0.3-0.7) indicating moderate agreement.
In an observational South African study at a level 1 trauma centre, an 11% and 5% yield of CTA was reported in penetrating lower extremity trauma, with soft signs and no clinical indication respectively.35 Another South African study revealed an 18% CTA yield in penetrating neck injuries, of which only 44% had abnormalities on catheter-directed angiography.36 The yield of our study was 6.1%. This is fairly comparable considering that the study population was restricted to isolated vascular injury with soft signs.
When only soft clinical signs are present, the prevalence of arterial injury is lower in penetrating trauma.37 Eighty-three per cent of the patients in this study sustained penetrating injury namely stabs and GSW.
The sample size was a limitation of the study. A further limitation was that this study data did not quantify the technical quality of the CTAs, as this certainly would affect study interpretation and has been previously identified as a reason for discrepancies. The level of radiology registrar training was not considered in the assessments, and most of the false positive CT angiogram interpretations may have been attributable to a less experienced registrar. The Hawthorne effect was another limitation but was negligible as most of the vascular surgeons and trainee radiologists were unaware of the methods of evaluation and details of the study.
Conclusion
The shortage of radiologists in South Africa and LMICs has been well documented and is likely to remain. This study highlights that there is very good interobserver agreement in the interpretation of CTAs in vascular trauma between the vascular, subspecialist trainees and surgeons and consultant radiologists with no false negatives.
This study is potentially applicable to major trauma hospitals in the country and is important because in several instances immediate patient management decisions depend on the vascular surgeons' interpretation of the CTAs. Further investigation at multiple South African centres would be valuable.
Conflict of interest
Both authors have reviewed articles for SAJS previously. TCH is an associated editor of SAJS. The authors have no other financial or non-financial interests to disclose.
Funding source
No funding was required.
Ethical approval
Ethical approval was obtained from the Biomedical Research Ethics Committee (BREC), College of Health Sciences, University of KwaZulu-Natal (BE488/15). The study was approved and the need for consent to participate in the study was waived. As per the norm in South Africa, routine written informed consent to perform the CT angiogram was obtained.
ORCID
P Parag https://orcid.org/0000-0003-4830-0523
TC Hardcastle https://orcid.org/0000-0002-3967-0234
REFERENCES
1. Wong C, Taubman K, Hoehne F, et al. The quality of surgical resident interpretation of after-hour CT scans of the head and abdomen in trauma. Am Surg. 2005;71(9):772-5. https://doi.org/10.1177/000313480507100916. [ Links ]
2. Miller-Thomas MM, West OC, Cohen AM. Diagnosing traumatic arterial injury in the extremities with CT angiography: pearls and pitfalls. Radiographics. 2005;25(Suppl 1):S133-42. https://doi.org/10.1148/rg.25si055511. [ Links ]
3. Pieroni S, Foster BR, Anderson SW, et al. Use of 64-row multidetector CT angiography in blunt and penetrating trauma of the upper and lower extremities. Radiographics. 2009;29(3):863-76. https://doi.org/10.1148/rg.293085517. [ Links ]
4. Bynoe RP, Miles WS, Bell RM, et al. Noninvasive diagnosis of vascular trauma by duplex ultrasonography. J Vasc Surg. 1991;14:346-52. https://doi.org/10.1016/0741-5214(91)90087-B. [ Links ]
5. Fry WR, Smith RS, Sayers DV, et al. The success of duplex ultrasonographic scanning in diagnosis of extremity proximity trauma. Arch Surg. 1993;128:1368-72. https://doi.org/10.1001/archsurg.1993.01420240076015. [ Links ]
6. Meissner M, Paun M, Johansen K. Duplex scanning for arterial trauma. Am J Surg. 1991;161:552-5. https://doi.org/10.1016/0002-9610(91)90897-M. [ Links ]
7. Knudson MM, Lewis FR, Atkinson K, Neuhaus A. The role of duplex ultrasound arterial imaging in patients with penetrating extremity trauma. Arch Surg. 1993;128:1033-7. https://doi.org/10.1001/archsurg.1993.01420210097013. [ Links ]
8. Diagnostic imaging. Radiologist sightings drop around the world. 2003 Jul 14 [Internet]. Available from: https://www.diagnosticimaging.com/article/radiologist-sightings-drop-around-world/. Accessed 8 Jul 2018. [ Links ]
9. Webber A. Shortage of radiologists could lead to service collapse. 2018 Aug 23. In NHS; latest news, recruitment & retention, labour turnover, retention of staff [Internet]. Available from: https://www.personneltoday.com/hr/radiologist-shortage-make-service-collapse/. Accessed 3 Mar 2019. [ Links ]
10. Greene W. Philippine startup takes on global radiologist shortage [Internet]. 2014 Nov 8. Available from: https://www.forbes.com/sites/techonomy/2014/11/08/philippine-startup-takes-on-global-radiologist-shortage/#174ea3e31235. Accessed 1 Jun 2017. [ Links ]
11. Hlongwane ST, Pitcher RD. Accuracy of after-hour 'red dot' trauma radiograph triage by radiographers in a South African regional hospital. S Afr Med J. 2013;103(9):638-40. [ Links ]
12. Hricak H, Abdel-Wahab M, Atun R, et al. Medical imaging and nuclear medicine: a Lancet oncology commission. Lancet Oncol. 2021;22(4):e136-72. https://doi.org/10.1016/S1470-2045(20)30751-8. [ Links ]
13. Section 27. Radiologists ask panel for help on pricing. 2016 May 5. Available from: https://section27.org.za/2016/05/radiologists-ask-panel-for-help-on-pricing/. Accessed 8 Jul 2018. [ Links ]
14. Mid-year population estimates 2016. Statistics South Africa. Available from: https://www.statssa.gov.za/publications/P0302/P03022016.pdf. Accessed 19 Nov 2018. [ Links ]
15. BBC.com. Delays in radiology results affecting patient care. 2018 Jul 19 [Internet]. Available from: https://www.bbc.com/news/health-44871476?intlink_from_url=https://www.bbc.com/news/topics/cmw2w95pz95t/radiology&link_location=live-reporting-story/. Accessed 8 Jul 2018. [ Links ]
16. Alfaro D, Levitt MA, English DK, Williams V, Eisenberg R. Accuracy of interpretation of cranial computed tomography scans in an emergency medicine residency programme. Ann Emerg Med.1995;25(2):169-74. https://doi.org/10.1016/S0196-0644(95)70319-5. [ Links ]
17. Al-Reesi A, Stiell IG, Al-Zadjali N, Cwinn AA. Comparison of CT head interpretation between emergency physicians and neuroradiologists. Eur J Emerg Med. 2010;17(5):280-2. https://doi.org/10.1097/MEJ.0b013e32833483ed. [ Links ]
18. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74. https://doi.org/10.2307/2529310. [ Links ]
19. Lian K, Bharatha A, Aviv RI, Symons SP. Interpretation errors in CT angiography of the head and neck and the benefit of double reading. Am J Neuroradiol. 2011;32(11):2132-5. https://doi.org/10.3174/ajnr.A2678. [ Links ]
20. Parag P, Hardcastle T. Interpretation of emergency CT scans in polytrauma: trauma surgeon vs radiologist. Afr J Emerg Med. 2020;10(2):90-94. https://doi.org/10.1016/j.afjem.2020.01.008. [ Links ]
21. Arentz C, Griswold JA, Halldorsson A, Quattromani F, Dissanaike S. Best poster award: accuracy of surgery residents' interpretation of computed tomography scans in trauma. Am J Surg. 2008;196:809-12. https://doi.org/10.1016/j.amjsurg.2008.08.007. [ Links ]
22. Fakhoury E, Abolghasemi D, McKinney J, et al. Surgical residents' interpretation of diagnostic radiologic imaging in the traumatically injured patient. J Trauma Acute Care Surg. 2018;84(1):146-9. https://doi.org/10.1097/TA.0000000000001701. [ Links ]
23. Vorhies RW, Harrison PB, Smith RS, Helmer SD. Senior surgical residents can accurately interpret trauma radiographs. Am Surg. 2002;68(3):221-6. https://doi.org/10.1177/000313480206800302. [ Links ]
24. Chung JH, Strigel RM, Chew AR, Albrecht E, Gunn ML. Overnight resident interpretation of torso CT at a level 1 trauma center an analysis and review of the literature. Acad Radiol. 2009;16(9):1155-60. https://doi.org/10.1016/j.acra.2009.02.017. [ Links ]
25. Briggs RH, Rowbotham E, Johnstone AL, Chalmers AG. Provisional reporting of polytrauma CT by on-call radiology registrars. Is it safe? Clinl Rad. 2010;65(8):616-22. https://doi.org/10.1016/j.crad.2010.04.010. [ Links ]
26. Miyakoshi A, Nguyen QT, Cohen WA, Talner LB, Anzai Y. Accuracy of preliminary interpretation of neurologic CT examinations by on-call radiology residents and assessment of patient outcomes at a level I trauma center. J Am Coll Radiol. 2009;6:864-70. https://doi.org/10.1016/j.jacr.2009.07.021. [ Links ]
27. Lal NR, Murray UM, Eldevik OP, Desmond JS. Clinical consequences of misinterpretations of neuroradiologic CT scans by on-call radiology residents. Am J Neuroradiol. 2000;21(1):124-9. [ Links ]
28. Terreblanche OD, Andronikou S, Hlabangana LT, et al. Should registrars be reporting after-hours CT scans? A calculation of error rate and the influencing factors in South Africa. Acta Radiol. 2012;53:61-68. https://doi.org/10.1258/ar.2011.110103. [ Links ]
29. De Witt JF, Griffith-Richards S, Pitcher RD. The accuracy of after-hour registrar computed tomography (CT) reporting in a South African tertiary teaching hospital. S Afr J Rad. 2014;18(1);591. https://doi.org/10.4102/sajr.v18i1.591. [ Links ]
30. Meyer RE, Nickerson JP, Burbank HN, et al. Discrepancy rates of on-call radiology residents' interpretations of CT angiography studies of the neck and circle of Willis. Am J Roentgenol. 2009;193(2):527-32. https://doi.org/10.2214/AJR.08.2169. [ Links ]
31. Tamjeedi B, Correa J, Semionov A, Mesurolle B. Interobserver agreement between on-call radiology resident and general radiologist interpretations of CT pulmonary angiograms and CT venograms. PLoS ONE. 2015;10(5):e0126116. https://doi.org/10.1371/journal.pone.0126116. [ Links ]
32. Shaham D, Heffez R, Bogot NR, Libson E, Brezis M. CT pulmonary angiography for the detection of pulmonary embolism: interobserver agreement between on-call radiology residents and specialists (CTPA interobserver agreement). Clin Imaging. 2006;30(4):266-70. https://doi.org/10.1016/j.clinimag.2006.01.001. [ Links ]
33. Ginsberg MS, King V, Panicek DM. Comparison of interpretations of CT angiograms in the evaluation of suspected pulmonary embolism by on-call radiology fellows and subsequently by radiology faculty. Am J Roentgenol. 2004;182(1):61-66. https://doi.org/10.2214/ajr.182.1.1820061. [ Links ]
34. Yavas US, Calisir C, Ozkan IR. The interobserver agreement between residents and experienced radiologists for detecting pulmonary embolism and DVT with using CT pulmonary angiography and indirect CT venography. Korean J Radiol. 2008;9(6):498-502. https://doi.org/10.3348/kjr.2008.9.6.498. [ Links ]
35. Le Roux A, Du Plessis AM, Pitcher R. Yield of CT angiography in penetrating lower extremity trauma. Emerg Radiol. 2021;28(4):743-9. https://doi.org/10.1007/s10140-021-01902-9. [ Links ]
36. Madsen AS, Laing GL, Bruce JL, Oosthuizen GV, Clarke DL. An audit of penetrating neck injuries in a South African trauma service. Injury. 2016;47(1):64-69. https://doi.org/10.1016/j.injury.2015.07.032. [ Links ]
37. Dennis JW, Frykberg ER, Veldenz HC, Huffman S, Menawat SS. Validation of nonoperative management of occult vascular injuries and accuracy of physical examination alone in penetrating extremity trauma: 5- to 10-year follow-up. J Trauma. 1998;44:243-52. https://doi.org/10.1097/00005373-199802000-00001. [ Links ]
 Correspondence:
Correspondence:
P Parag
Email: priyaparag05@gmail.com














