Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3905
CASE REPORT
Blindness and ophthalmoplegia from metastatic breast carcinoma
S MapipaI; AL SibiyaI; I BuccimazzaII
IDepartment of Otorhinolaryngology, School of Clinical Medicine, University of KwaZulu-Natal, South Africa
IIBreast and Endocrine Unit, Department of Specialised Surgery, Inkosi Albert Luthuli Central Hospital, South Africa
SUMMARY
We report a very rare complication from metastatic breast cancer of right-sided blindness and ophthalmoplegia in a 70-year-old female. Cavernous sinus syndrome, superior orbital fissure syndrome and complicated sinusitis were considered in the differential diagnosis but involvement of cranial nerves II, III, IV, VI and the ophthalmic division of V were consistent with an orbital apex syndrome. She had been diagnosed with breast carcinoma 10 years previously. This report highlights the correct clinical and diagnostic pathway with computed tomography (CT) scan of the brain and paranasal sinuses to evaluate for the presence and extent of pathology and biopsy route for any causative mass. In this patient, the mass in the right parasellar region and orbital apex with extension into the sphenoid sinus was amenable to transsphenoidal biopsy which showed features suggestive of metastatic breast carcinoma. She was treated with palliative whole brain radiotherapy without resolution of symptoms.
Keywords: blindness, ophthalmoplegia, metastatic breast carcinoma, orbital apex syndrome
Case report
A 70-year-old female presented with a 6-month history of blindness in the right eye and loss of sensation on the ipsilateral forehead. The patient had previously been diagnosed with a locally advanced (cT4b N2 M0), oestrogen receptor positive, HER-2 negative invasive duct carcinoma of the left breast in 2011. She had completed six cycles of neoadjuvant chemotherapy (5 fluorouracil, epirubicin and cyclophosphamide) followed by a left total mastectomy and level II axillary lymph node dissection in 2012. Extended radiation fields were administered. For the next 5 years, she received anastrozole and had been on yearly surveillance for the 5 years with no evidence of disease recurrence.
Examination of the head revealed involvement of the optic nerve (CN II) resulting in blindness, of the oculomotor (CN III), trochlear (CN IV) and abducens (CN VI) nerves resulting in ophthalmoplegia and of the ophthalmic division of trigeminal nerve (CN V) causing loss of sensation over the forehead, all on the right side. These findings were suggestive of an orbital apex syndrome. The diagnoses of superior orbital fissure syndrome and cavernous sinus syndrome were considered, as they have overlapping symptoms with orbital apex syndrome. However, cavernous sinus syndrome is characterised by involvement of the maxillary division of the trigeminal nerve together with some of the cranial nerves affected in orbital apex syndrome (III, IV and VI), whereas the superior orbital fissure syndrome is a complex of impaired function of cranial nerves III, IV, VI and the ophthalmic division of the trigeminal nerve, and generally spares the optic nerve. Major precipitating factors for all these syndromes include trauma, tumour and inflammation.
The patient had not sustained any trauma and had no history of inflammatory disease such as sarcoidosis.
Physical examination did not show signs of loco-regional recurrence on the left chest wall. Mammography of the right breast showed benign intramammary calcifications. The ultrasound examination did not demonstrate features of tumour recurrence in the left anterior chest wall, either axillae or the right breast.
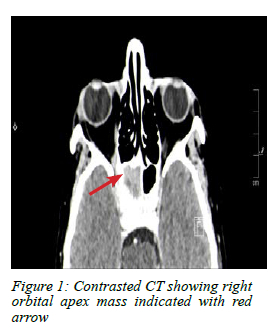
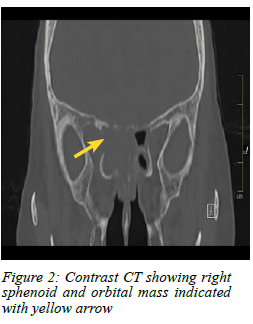
A computed tomography (CT) scan of the brain and paranasal sinuses showed a mass lesion in the right parasellar region and orbital apex with extension into the sphenoid sinus (Figure 1 and 2).
An endoscopic nasal trans-sphenoidal biopsy was undertaken because this technique provided favourable access into the orbital apex. Macroscopically abnormal mucosa on the medial wall of the right sphenoid sinus was biopsied and revealed features of metastatic oestrogen receptor positive breast carcinoma. The E-cadherin and GATA-3 immunopositivity confirmed the ductal breast origin of the malignancy.
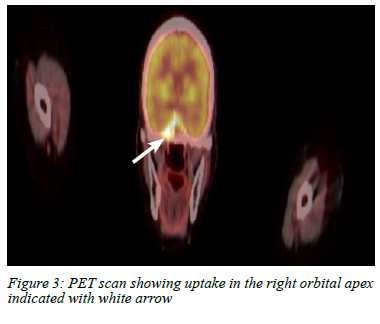
Full body positron emission tomography (PET) scan performed for staging purposes demonstrated the mass in the apex of the right orbit and superior aspect of the sphenoid sinus with no other areas of suspicious uptake (Figure 3). The patient was discussed at a multidisciplinary team (MDT) meeting where palliative radiotherapy to the metastatic site and a second-line aromatase inhibitor were proposed. She completed palliative whole brain radiotherapy with no resolution of symptoms. The patient is alive, but unfortunately remains blind in the right eye.
Discussion
Breast carcinoma usually metastasises to the bone (4760%), liver (19-30%), lung (16-34%) and brain (10-16%).1 There are a few case reports of metastatic breast cancer to either the orbit or paranasal sinuses.1-4 When this does occur, the condition is usually unilateral and appears 4.5 to 6.5 years after treatment of the primary lesion. Metastatic breast cancer concurrently to both the orbit and paranasal sinuses are rare and, to our knowledge, have not been reported in the literature. In our case, the patient presented with metastases to both the orbit and sphenoid sinus after a disease-free interval of 10 years, and without any clinical features of breast carcinoma recurrence or evidence of other distant disease, making this a unique and atypical presentation.
As of 2018, 40 cases of metastatic breast carcinoma to the orbit, presenting as orbital apex syndrome have been reported. Accurate examination of the cranial nerves differentiates it from other types of ophthalmoplegia.4 Orbital apex syndrome involves impairment of cranial nerves II (optic), III (oculomotor), IV (trochlear), VI (abducens) and V2 (maxillary division of the trigeminal nerve), and patients usually present with orbital pain as well as impaired eye movements,5 as was the case in our patient. There are overlapping signs and symptoms with cavernous sinus syndrome and superior orbital fissure syndrome; however, in these latter two syndromes, the optic nerve is generally spared.
Common causes of orbital apex syndrome include inflammatory diseases (e.g., sarcoidosis, granulomatosis with polyangiitis), infectious diseases (aspergillosis) or primary neoplastic lesions of anatomical structures in the area (e.g., nasopharyngeal carcinoma).5 The most common primary that metastasises to the paranasal sinuses is renal cell carcinoma.2
There are two main histological types of invasive breast carcinoma. Ductal carcinoma accounts for the majority of cases (78%), while only around 11% of invasive breast cancers arise from the breast lobules.6 Typically, invasive lobular carcinoma accounts for most breast carcinoma metastases to the orbit.7 Curiously, in our patient, the metastasis was from breast duct origin.
Metastases of primary breast cancer to the paranasal sinuses is very rare - the most commonly involved sinus is the maxillary (23%), and sphenoid sinus involvement is rare (15%).8
Commonly patients with metastases to the paranasal sinuses present with signs similar to those of complicated rhinosinusitis, namely peri-orbital swelling, proptosis, loss of vision and ophthalmoplegia. Our patient presented with both blindness and ophthalmoplegia, which resulted in a prompt search for the cause. Typically, in patients with a non-specific presentation, diagnosis and management are delayed. Practitioners should look out for red flags such as failure to improve on standard treatment and cranial nerve palsies.
The diagnostic algorithm includes a full physical examination and imaging. CT scan of the brain and paranasal sinus is the primary imaging modality of choice as it can demonstrate a mass in the orbit. Magnetic resonance imaging (MRI) scans help delineate the mass from the surrounding soft tissue structures.2-49 In our patient, MRI was not performed as the CT scan clearly delineated the pathology and site.
PET scan is used to identify other areas of metastases. In our patient the absence of other metastatic sites guided the MDT treatment decision to only administer palliative local therapy.
Histopathological examination helps determine if the tumour is primary (arising de novo) or metastatic.2,3,9
Conclusion
Blindness and ophthalmoplegia from breast cancer metastases to the orbital apex and sphenoid sinus after a 10-year disease-free interval is very rare. Involvement of the optic nerve differentiates this presentation from other forms of ophthalmoplegia found in the superior orbital fissure and cavernous sinus syndrome. A high-resolution CT scan is often sufficient to delineate the location and extent of the disease, and guide biopsy which is necessary to determine the aetiology and origin of the disease. A PET scan is used for oncological staging and to guide appropriate treatment. Prognosis for orbital metastasis of breast cancer is poor with an average survival of 31 months.4
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
This confirms that the case referenced in this report was retrieved from the Ethics Committee approved retrospective and prospective KwaZulu-Natal Otorhinolaryngology Database [Class Approval BREC/00002826/2021]. The Ethics Committee has approved this database with a waiver of an informed consent requirement.
ORCID
S Mapipa https://orcid.org/0000-0002-1238-369X
AL Sibiya https://orcid.org/0000-0002-4901-9269
I Buccimazza https://orcid.org/0000-0002-5399-3101
REFERENCES
1. Johnston J, George M. Late metastasis to macroscopically normal paranasal sinuses from breast carcinoma. Ecancermedicalscience. 2013;7:298. https://doi.org/10.3332/ecancer.2013.298. [ Links ]
2. Reitsma S, Schuil PJ. Metastasis of breast carcinoma to the paranasal sinuses - report of two cases and systematic review of literature. Rhinol Online. 2018;1:3-8,20. https://doi.org/10.4193/RHINOL/18.001. [ Links ]
3. Maity A, Maughan E, Vasani S, Alusi G. Ethmoidal metastasis as a first presentation of breast cancer: a case report. Ann R Coll Surg Engl. 2018;100(6):e139-41. https://doi.org/10.1308/rcsann.2018.0065. [ Links ]
4. El Bakraoui K, El Morabit B. Orbital metastasis from a triple negative breast cancer: case report and literature review. Case Rep Oncol. 2020;13(2):1042-6. https://doi.org/10.1159/000509348. [ Links ]
5. Badakere A, Patil-Chhablani P. Orbital apex syndrome: a review. Eye Brain. 2019;11:63-72. https://doi.org/10.2147/EB.S180190. [ Links ]
6. Li CI, Uribe DJ, Daling JR. Clinical characteristics of different histologic types of breast cancer. Br J Cancer. 2005;93(9):1046-52. https://doi.org/10.1038/sj.bjc.6602787. [ Links ]
7. Blohmer M, Zhu L, Atkinson JM, et al. Patient treatment and outcome after breast cancer orbital and periorbital metastases: a comprehensive case series including analysis of lobular versus ductal tumour histology. Breast Cancer Res. 2020;22(1):70. https://doi.org/10.1186/s13058-020-01309-3. [ Links ]
8. Al Amer L, Al Khatib A, Azzah G, Almomen A. Breast carcinoma metastasis to the sphenoid sinus: a case report. Pan Arab J Rhinol. 2018;8:19-20. [ Links ]
9. Chang CC, Tsou YA, Lin MH, Tseng GC. Metastasis of breast cancer to the sphenoid sinus presenting as Tolosa-Hunt syndrome. Tzu Chi Med J.2010;22(3):153-6. https://doi.org/10.1016/S1016-3190(10)60062-6. [ Links ]
 Correspondence:
Correspondence:
S Mapipa
Email: solethumapipa@gmail.com














